- English
- ePUB (mobile friendly)
- Available on iOS & Android
About this book
The book is intended as a concise overview of current orthopaedic practice. It will be of interest to orthopaedic surgeons in practice and to orthopaedic trainees - both specialist and basic surgical, in particular, orthopaedic specialist registrars in the UK preparing for the FRCS Orth. exam, or trainees in other countries at an equivalent stage of orthopaedic training. Medical students doing orthopaedic attachments will find it a practical reference tool. In addition, individuals involved in the care of orthopaedic patients, such as physiotherapists and nurse practitioners, will find the book useful. With increasing subspecialisation in orthopaedic surgery, it is more difficult for the specialist to keep abreast of recent changes and current trends in the management of orthopaedic conditions other than their own area of interest. This book aims to fill that void and will be an easily readable source with information that is concise and current. Emphasis is placed on the current literature and an effort has been made to provide evidence on controversial topics with annotated references incorporated into the text. These will be a useful resource for further reading. Any reader wishing to gain insight into 21st century orthopaedic surgery will find this book of interest and value.
Tools to learn more effectively

Saving Books

Keyword Search

Annotating Text

Listen to it instead
Information
Chapter 1 Arthroplasty
Total hip replacement
Indications
Contraindications
Assessment and investigations
Informed consent
Cemented femoral component design
Offset
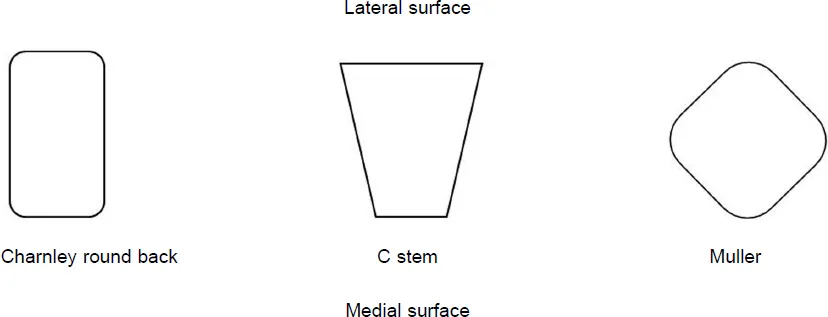
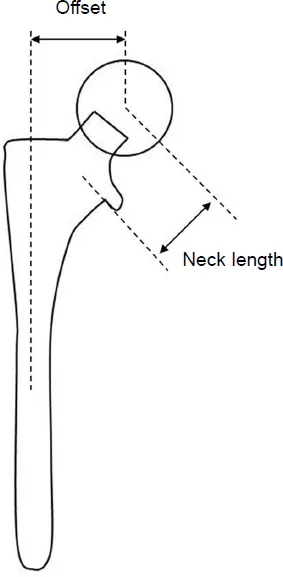
Table of contents
- Cover Page
- Title Page
- Copyright Page
- Contents
- Contributors
- Foreword
- Abbreviations
- Chapter 1: Arthroplasty
- Chapter 2: Shoulder disorders
- Chapter 3: Sports medicine
- Chapter 4: Spine and nerve injuries
- Chapter 5: Foot and ankle
- Chapter 6: Hand
- Chapter 7: Bone and soft tissue tumours
- Chapter 8: Infections
- Chapter 9: Non-union
- Chapter 10: Inflammatory joint disorders
- Chapter 11: Arthrodesis and amputations
- Chapter 12: Disorders in children
- Chapter 13: Trauma
- Chapter 14: Nerve injuries and neuromuscular disorders
- Chapter 15: Imaging
- Chapter 16: Clinical examination
- Chapter 17: Surgical approaches
- Index
Frequently asked questions
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app