![]()
Case 1
A 44-year-old woman presents to the emergency room with right upper quadrant pain. The pain began about 20 minutes after eating dinner. It is described as a "shooting pain" that is constant, radiates to her back, and is 6/10 in intensity. The pain is worse on deep inspiration, and a tablet of oxycodone offers some relief. She denies nausea or vomiting. Her bowel movements are regular. She has never had this pain before.
What is your differential diagnosis?
The differential diagnosis includes cholelithiasis, acute cholecystitis, pancreatitis, gastritis, peptic ulcer disease, gastric volvulus, and intussusception.
Physical examination
| Vitals | Afebrile, HR 88 bpm, BP 130/78mmHg, oxygen saturation 99% on RA. |
| GEN | No distress. |
| HEENT | No scleral icterus. |
| CVS | Normal S1, S2. No murmurs, rubs, or gallops. |
| RESP | Clear to auscultation. |
| ABD | Soft and non-tender. No rigidity, guarding, or rebound tenderness. Bowel sounds are normal. Rectal examination reveals an empty vault. |
| EXT | No edema. |
Does this narrow your differential diagnosis?
Yes. Volvulus and intussusception can be removed from the differential diagnosis, as bowel sounds are altered in these clinical settings.
What blood test(s) will you order?
| LFTs | AST | 267 units/L |
| ALT | 285 units/L |
| Alkaline phosphatase | 262 units/L |
| Total bilirubin | 3.6mg/dL |
What is the pattern of the elevated LFTs?
Elevated LFTs usually suggest either a hepatocellular process or an obstructive (or cholestatic) process. A cholestatic process presents with elevated alkaline phosphatase and elevated total bilirubin levels. With the passage of a gallstone through the common bile duct, ALT may be the first measure to appear abnormal.
What other blood tests will you order?
CBC, CHEM-7, and bHCG.
All are within normal limits.
What imaging test will you order?
Your differential diagnosis already includes gallbladder pathology. Therefore, an ultrasound is the most important imaging test. The probe is placed over the ninth rib costal margin in the right mid-clavicular line. You see the image shown in Figure 1.
Describe what you see and read on
The ultrasound shows a gallbladder in the sagittal view. Gallstones (white arrows) cast dark shadows (yellow arrows) on ultrasound. Changing the patient’s position demonstrates the stones are mobile. This image does not show a thickened gallbladder wall, or a black rim around the gallbladder wall suggesting fluid (pericholecystic fluid). The patient’s Murphy’s sign was negative on physical examination.
By now you have admitted the patient, kept her nil by mouth, started IV fluids, and called for a surgical consultation. Later you receive the radiology report and notice the patient’s common bile duct is 8mm.
What is your initial diagnosis, and how will you proceed?
The diameter of the common bile duct, measured in millimeters, should be less than or equal to the patient’s age in decades. So for this 44-year-old patient, who is in her fifth decade, it should be 5mm or less. An 8mm bile duct is suggestive, but not diagnostic, of at least some degree of biliary obstruction, and liver enzymes elevated in an obstructive pattern support this diagnosis. Given the numerous gallstones seen on ultrasound, a working diagnosis of choledocholithiasis – common duct stone(s) – is reasonable.
The next step is to obtain a GI consultation for a possible ERCP. This is arranged for the next day. The image shown in Figure 2 is obtained during the procedure.
Describe what you see and read on
A fluoroscopic scout view of the right upper quadrant is obtained prior to the endoscopic procedure. Numerous stones are present in the gallbladder (black arrow). In addition, a solitary stone is seen outside the expected location of the gallbladder (white arrow), suggesting a stone in the biliary tree. A fluoroscopic image is obtained during the ERCP (Figure 3).
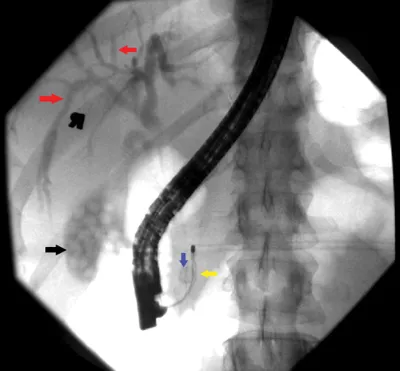
Describe what you see and read on
This fluoroscopic image shows that the gallbladder (black arrow) and intrahepatic biliary ducts (red arrows) have been opacified with contrast. There is air in the common bile duct after biliary sphincterotomy, and a Dormia basket (yellow arrow) has engaged the stone (blue arrow) and is being used for its extraction.
A stone that was not seen on ultrasound was obstructing the common bile duct. This also explains why the patient had elevated LFTs, as the stone was causing biliary obstruction.
Overnight, the patient’s laboratory results improved. She remained pain-free and was discharged with a plan to have a laparoscopic cholecystectomy at a later date.
Clinical pearl
| • | Only two-thirds of common duct stones are seen on ultrasound when the common bile duct is less than 10mm. In this case the ultrasound did not show the stone in the duct, but there was a high clinical suspicion based on clinical history, elevated LFTs, and the slightly dilated common bile duct at 8mm. |
Impress your attending
What are gallstones made from?
Most gallstones (approximately 85%) are composed of cholestero...