![]()
Part 1 Introduction
Management of ulcerative colitis
Ailsa L. Hart BMBCh MRCP PhD Senior Clinical Lecturer, Imperial College and Consultant Gastroenterologist, St Mark’s Hospital, London, UK
Ulcerative colitis is an inflammatory bowel disease of unknown cause (idiopathic) that affects up to 120,000 people in the UK with between 6,000 and 12,000 new cases being diagnosed each year.
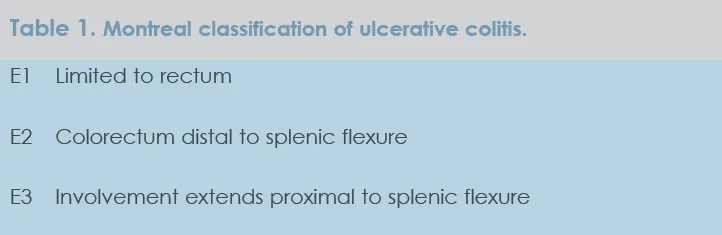
The principal symptoms of ulcerative colitis include diarrhoea with rectal bleeding, abdominal pain and cramps, usually relieved by defecation. Symptoms depend on the extent and severity of disease. When disease extends beyond the rectum, patients tend to complain of diarrhoea (often with blood and mucus), faecal urgency and faecal incontinence. Patients with disease limited to the rectum (proctitis) tend to present with rectal bleeding and mucus discharge and a proportion of these patients complain of constipation, as opposed to diarrhoea. Patients with a more severe colitis have associated systemic symptoms of fever, vomiting and anorexia. One way of classifying ulcerative colitis is using the Montreal classification (Table 1) which takes into account the part of the colon affected 1.
Ulcerative colitis tends to begin in the rectum and extends proximally affecting the bowel in a continuous fashion. Approximately one third of patients have disease confined to the rectum (proctitis) or the rectum and sigmoid (proctosigmoiditis) at the time of diagnosis. Approximately one third of patients will have a pancolitis at diagnosis. Disease can progress and extend, so that patients who have rectal or rectosigmoid involvement at presentation can progress to have disease affecting the proximal colon in 10-30% of patients at 10-year follow-up and in up to 50% at 25-year follow-up 2, 3.
The pattern of disease can follow different courses. Most patients have a chronic intermittent course with periods of remission and relapse 3; a cumulative relapse rate in the first year after diagnosis is about 50% irrespective of disease extent. Other patients have chronic continuous symptoms. Some patients have a single attack and subsequent remission. Some patients have a fulminant course leading to colectomy within the first disease episode. About 10% of patients have long-term remission after the initial disease episode. The extent of disease at diagnosis does not seem to affect the subsequent disease activity. When patients are followed up long term, disease activity in the previous year appears to be a good indicator of the subsequent course of disease 3. For example, a full year in remission is prognostically favourable and predicts an 80% probability of staying in remission for another year. The more years in remission, the higher the probability of experiencing yet another year in remission. On the other hand relapse in the previous year predicts a 70% probability of relapse in the subsequent year.
Both disease activity and extent determine treatment choice in the management of ulcerative colitis. For this reason this section is divided into chapters in which the extent of disease (e.g. proctitis, left-sided disease, extensive disease) and severity of disease (e.g. acute severe ulcerative colitis) are taken into account.
Each chapter has an algorithm of care, but in practice the care is individualised to the patient. Factors that contribute to the individual management of patients include patient preferences and beliefs; external factors such as schooling, work and family lives that may influence timing and choice of certain treatments; intolerance to medications; and other comorbidities. A clear agenda with a time-bound approach needs to be discussed with the patient, so that expectations of both the patient and health care professionals can be explored and met.
Treatment goals in ulcerative colitis include induction and maintenance of remission, mucosal healing, avoidance of admission to hospital, avoidance of surgery, minimising the risk of cancer, and optimised quality of life. Definition of remission and the contribution of clinical aspects, endoscopy, biomarkers and histopathology remain to be decided, but the bar should be raised with regards to what patients and physicians aim to achieve. An improvement in symptoms and wellbeing is unlikely to predict long-term outcome and is no longer optimal.
Treatment options for ulcerative colitis are increasing with development of new drug formulations and dosing strategies. There is a greater appreciation that assessment needs to occur in a timely fashion so that therapy can be escalated and optimised. There is also increased awareness of compliance problems that may need to be discussed and addressed.
References
| 1. | Silverberg MS, Satsangi J, Ahmad T, et al. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: Report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. Can J Gastroenterol 2005; 19 Suppl A: 5-36. |
| 2. | Ayres R... |