1
Fibro what?
Although we are learning more and more about the causes of fibromyalgia, it remains a difficult condition to diagnose. No one can see the pain, and it doesn’t show itself in X-rays or available blood tests and bone scans. You may have undergone a whole gamut of ‘investigations’, and while it is reassuring when major illnesses are ruled out, you have probably prayed, at the same time, for something to show up.
It may help to know that, prior to diagnosis, your doctor, likely as not, felt as mystified as you. Ironically, your doctor’s inability to determine the cause of your symptoms may have been hampered by his or her medical training. Medical students learn that specific conditions produce distinctive symptoms and that elimination of the cause ensures, in most cases, full recovery. This ‘classical medical model’ has been used successfully for many years, leading to numerous advances in modern medicine. Unfortunately, because the difficulties presented by fibromyalgia patients do not fit this model, delayed diagnosis is common.
On a more positive note, doctors are slowly but surely familiarizing themselves with the peculiar nature of fibromyalgia and referring their patients to a rheumatologist who is familiar with the condition. A diagnosis of fibromyalgia should only be made when all other diseases are ruled out. It can therefore be said that fibromyalgia is a diagnosis of exclusion.
What is fibromyalgia?
You may wonder how the name ‘fibromyalgia’ came into being. The word can be split into parts that are easier to understand. ‘Fibro’ means fibrous connective tissue – tendons and ligaments – ‘my’ means muscle, and ‘algia’ means pain. The word ‘syndrome’ means a collection of symptoms that, when they occur together, identify an illness. The symptoms commonly occurring with fibromyalgia include persistent, widespread pain, fatigue, sleep disturbance, anxiety, irritable bowel problems, irritable bladder problems, reactive depression, headaches, allergies, ‘foggy brain’ and morning stiffness (see Chapter 2).
First the good news … fibromyalgia is not a degenerative disease, it does not cause deformity and you are not going to die from it. Studies have shown that the majority of people with it either stay the same or improve – and, although progress is generally slow, the changes can be dramatic. However, notable advances appear only to be made in those who take steps to help themselves.
Fibromyalgia is, without doubt, a ‘challenging’ condition, for, as well as currently being incurable, its chief characteristic is pain. Those who have fibromyalgia often complain that they ‘hurt all over’, although the neck, shoulders – generally in the region between the shoulder blades – chest, lower back and buttocks seem to be the principal areas affected. The pain is mainly muscular for most people, but the tendons and ligaments are often a source of pain, too. Trapped nerves from bunched muscles can also cause pain – and this is usually a sharper, more intense pain than that coming directly from the muscles, tendons and ligaments.
Due to nearby tense and painful tissues, joint mobility is occasionally reduced in fibromyalgia – but the joints themselves don’t sustain damage. There is, however, an increased risk of developing premature osteoporosis – where the bones become brittle and more prone to fractures. Post-menopausal women whose activity levels are greatly limited are at greater risk of osteoporosis than anyone else.
Widespread pain
The pain of fibromyalgia is commonly described as ‘widespread’, and generally arises at neuromuscular junctions – that is, the places where the muscles receive electrical input from the nerve endings. Several areas may hurt at one time, but one particular region may be the cause of most concern. Also, the pain can migrate from area to area. One day your neck may hurt so badly you can barely turn your head; the next, although your neck pain has mysteriously eased, your legs ache so much that walking is difficult.
Such bizarre comings and goings of pain are difficult to rationalize, almost impossible for onlookers to comprehend and incredibly frustrating all round. Besides often being random, the pain may fluctuate during the course of each day. Factors particular to each person can be responsible for aggravating it.
Stress is one of the greatest enemies of someone with fibromyalgia, as is the lack of restorative sleep, cold and/or humid weather conditions and too much or the wrong type of activity. Any one of these elements may provoke a flare-up of symptoms lasting for days, weeks or even months. On the other hand, symptoms can improve for no apparent reason.
Just as no two people are exactly alike, no two people with fibromyalgia experience precisely the same pain. One person may complain of searing, burning pains, another of throbbing sensations, another of tingling and numbness, and another of constant, nagging aches. Whatever the sensation felt, it is far from pleasant, and when accompanied by a multitude of other symptoms and illnesses, it is no wonder people can feel overwhelmed.
Pain origins
Pain from the following sources contributes to the overall picture.
- Pain from muscle tension Muscle tension creates an increased demand for blood and oxygen, yet inhibits the drainage of waste materials. This creates more pain, therefore more muscle tension (see below).
- Pain from low muscle endurance Sustained activity creates many difficulties in fibromyalgia. For example, you may be able to lift, in turn, three 1 kg bags of sugar without immediate pain, but shortly afterwards your muscles may begin to hurt. Lifting no more than one or two bags of sugar would, in this instance, be recommended. If you need to lift three or more bags in total, allow your muscles to rest for a few minutes between each exertion.
- Myofascial (localized) pain This, often very acute pain is induced by ‘trigger points’ that are regularly ‘activated’ (see below).
- Pain from microtraumas Microtraumas are slow-healing microscopic tears in the muscle tissue. Experts believe they occur in most cases of fibromyalgia (for more details, see Chapter 2).
- Pain from abnormal stiffness Extreme stiffness sometimes occurs in fibromyalgia. It can arise when the individual sits or lies down for prolonged periods of time (for more details, see Chapter 2).
Pain from muscle tension
Certain muscle groups are, in all people with fibromyalgia, permanently tense and therefore painful. The tension may be due to over-activity, emotional stress or postural problems. Permanently tense muscles demand increased blood and oxygen supplies, but, at the same time, drainage of waste materials is inhibited by the tension. This leads to further tension and so further pain. The muscles eventually adapt to this cycle by becoming shorter and more fibrous, like the stringy bits in a piece of tough meat.
Gradually, these shorter, less elastic muscles begin to pull on their tendons – the structures that anchor them to the bones. The tendons then start the same process, becoming deprived of oxygen and clogged with waste materials. Like the affected muscles, they, in turn, grow fibrous and painful – and painful tissues burn energy at a terrific rate.
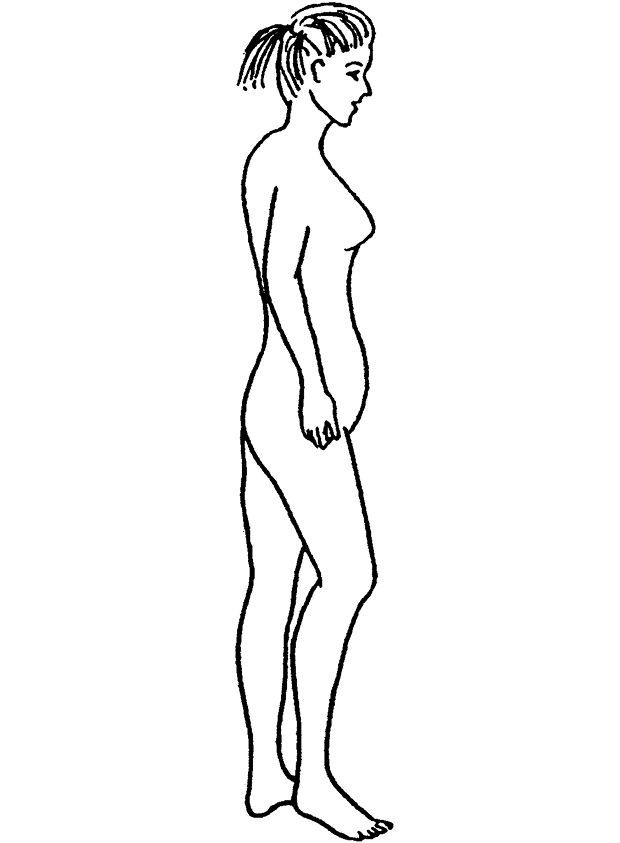
These tense and fibrous muscles go on to cause further problems, as, for every set of tense muscles, there is always an opposing set of weak muscles. For example, a person with weak abdominal muscles invariably has tight lower back muscles. Each set of permanently tense and fibrous muscles has an opposite set of muscles that is permanently weakened, and this eventually leads to the postural changes that typify fibromyalgia (see Figure 1).
Figure 1 Postural changes typical of fibromyalgia
Trigger points
Not to be confused with the ‘tender points’ used to diagnose fibromyalgia (see under ‘Diagnosis’ later in this chapter), trigger points are localized areas of pain and sensitivity occurring in permanently tense and fibrous tissues. Due to inadequate local circulation, these areas suffer from increased energy consumption and reduced oxygen supply.
When pressed, a trigger point will radiate pain and/or numbness into further areas. When ‘activated’ by cold, stress, over-exertion and so on, a trigger point will automatically transmit pain and numbness to further areas. If your doctor pressed a certain point on your upper back, say, and, as a result, you felt pain or numbness down one arm, the spot he had pressed would have been a trigger point.
Light-pressure, trigger-point massage generally reduces the pain and relaxes the muscle. Pain from active trigger points is a feature of almost all chronic (long-lasting) pain conditions.
Myofascial pain syndrome
You may be surprised to learn that many people with fibromyalgia also have a condition called myofascial pain syndrome (MPS for short) – I, for one, do. MPS arises from referred trigger-point pain, which occurs when one or more trigger points are regularly ‘activated’ (see ‘Trigger points’ above). It causes the localized, and often very severe, pain that is usually the worst part of our fibromyalgia. My myofascial pain is in my neck, shoulders and upper back. Other common areas are the chest, buttocks and lower back.
MPS is diagnosed in the same way as fibromyalgia (see under ‘Diagnosis’ later in this chapter). The following four points, taken together, can indicate the existence of MPS:
1 the presence of chronic, localized pain;
2 the fact that there is no obvious cause of the pain – that is, joint strain or arthritis;
3 the fact that the pain has neither responded to treatments prescribed for what was originally thought to be the problem, nor to further treatments, including rest;
4 the fact that the pain intensifies when you are under some kind of stress, such as after physical activity, emotional stress or exposure to cold.
There are some people, however, who have MPS and not fibromyalgia. These people experience less morning stiffness, less fatigue and less incidence of digestive disorders. The best treatment of MPS is trigger-point massage and manipulation, and fortunately more and more physiotherapists are being trained to do this. On a short-term basis, trigger points respond well to heat treatments and acupuncture.
What causes fibromyalgia?
Fibromyalgia is believed to arise from a variety of factors working together. Indeed, the following abnormalities have been found:
- The central nervous system (the brain and spinal cord) Advanced scanning technology has shown that people with fibromyalgia have reduced blood flow and energy production in the regions of the brain dealing with pain regulation, memory and concentration.
- The endocrine system (the hormones) Research into the endocrine system has shown that hormonal imbalances play a leading role in fibromyalgia. Research is now focusing on hormonal neurotransmitters.
- The immune system (antibody protection against infection) Immune system disturbances resulting from an overload of environmental toxins (pesticides, aerosols, car fumes and so on) and/or viral activity can arise when activated by specific triggers.
Chronic pain development
For many years, it was supposed that the same pain stimulus – such as a pinprick – produced the same degree of pain in every man, woman and child. However, we now know that if the pain stimulus is repeated many times there is an amplification of perceived pain, which causes the central nervous system (CNS, for short) to become sensitized. (The primary function of the CNS, located in the brain and spinal cord, is to analyse input from nerve cells.)
In 1992, researchers1 found that persistent severe pain will only arise in an individual who has suffered severe pain in the past (the CNS ‘remembers’ past pain intensity) and only after physical trauma, such as an injury or surgery, when the person concerned limits movement of the affected area. The individual expects to feel better after limiting movement, but many find that their pain levels have actually increased. We see, therefore, how persistent pain can arise.
Persistent pain can quite easily advance into a chronic pain situation – the second step towards central sensitization. In fact, modern scanning technology has demonstrated that prolonged pain can create a gradual build-up of electrical response throughout the CNS. The currents can build to such intensity that a state of chronic pain results – where the CNS is sensitized to pain. All chronic pain conditions involve a degree of central sensitization. Indeed, the central nervous...