Environmental Policy and Public Health
Emerging Health Hazards and Mitigation, Volume 2
- 322 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
Environmental Policy and Public Health
Emerging Health Hazards and Mitigation, Volume 2
About this book
Written by environmental health experts with long teaching and professional careers in policy and public health, the third edition of Environmental Policy and Public Health comprises two volumes, addressing key physical hazards in the environment that impact public health. The first volume on Principal Health Hazards and Mitigation is complemented by the second volume, Emerging Health Hazards and Mitigation.
Volume 2 discusses emerging health hazards and mitigation including environment-related infectious diseases, COVID-19 pandemic, social justice, and drugs and public health. New in this volume are a chapter on firearms violence as a public health hazard, a chapter on transportation and how built environments can affect human health and social well-being, and a chapter on noise and light pollution. As human populations increase and technology adds more devices to daily use that generate noise and light, adverse human and ecological health effects have become recognizable and require time-sensitive policy actions to mitigate and where possible prevent adverse health effects. Each chapter explains with great clarity how new environmental health issues are translated into public health policies. The volume concludes with case studies and practice questions to facilitate interactive learning for upper-level undergraduate and graduate students taking courses in public health and environmental sciences. The case studies and practice questions allow for a diverse portfolio of in-person and hybrid pedagogical strategies and tools at the fingertips of faculty who not only teach policy courses but whose course topics have policy relevance, such as climate and health.
Frequently asked questions
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Information
1 Environment-Related Infectious Diseases
1.1 Introduction
1.2 Infectious Diseases – A Global Perspective
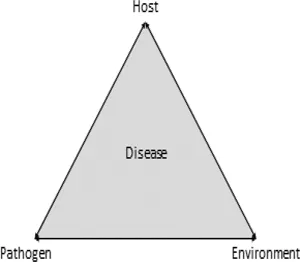
1.3 The Environment and Infectious Diseases
1.3.1 Cholera
1.3.2 Typhus
Table of contents
- Cover
- Half Title
- Title Page
- Copyright Page
- Table of Contents
- Preface
- Authors
- Chapter 1 Environment-Related Infectious Diseases
- Chapter 2 Solid and Hazardous Waste
- Chapter 3 Drugs and Alcohol
- Chapter 4 Firearms Violence
- Chapter 5 Noise and Light Pollution
- Chapter 6 The Built Environment
- Chapter 7 Transportation
- Lessons Learned and Authors’ Reflections
- Environmental Policy and Public Health: Emerging Health Hazards and Mitigation, Volume 2 Workbook
- Index