![]()
1
INTRODUCTION – WHY INTEGRATED CARE IS SO HARD TO ACHIEVE
In 2020, scholars published the results of a systematic review on integrated care. Their verdict was that integrated care is ‘an emergent set of practices’ rather than something that could be brought about by policy diktat (Hughes, Shaw, & Greenhalgh, 2020).
This finding should not have surprised anybody researching care integration in health systems. For decades, whilst repeatedly announced by policy documents, integration has remained elusive. Looking at the volumes of papers published on integrated care in health services and between health and social care, one is struck by the pluralism and diversity of implementing, investigating and evaluating integrated care (Oelke, Suter, da Silva Lima, & Van Vliet-Brown, 2015; Stokes et al., 2018; Suter, Oelke, Adair, & Armitage, 2009). This diversity might be a sign for how little we agree on what we are actually looking at. This lack of consensus extends not just to the phenomenon of integration itself. It stretches all the way from what integration may be (its ontology) to how we can examine it and produce reliable insights about it (its epistemology). In other words, integration in health and social care systems is a multifaceted issue, spurning simplistic attempts to resolve it.
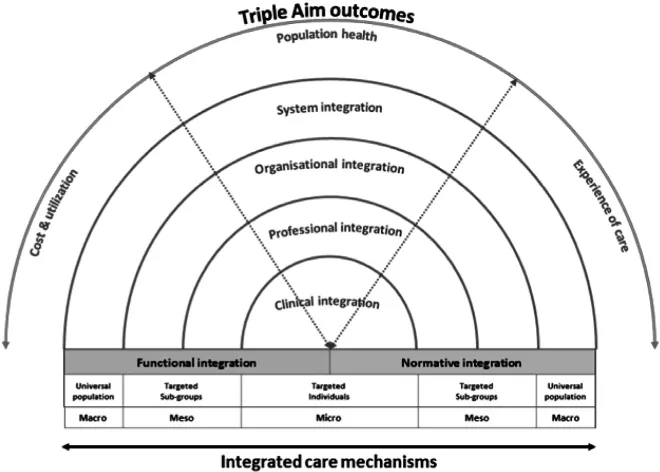
It seems sensible, however, to also acknowledge how far we have come. Policy makers have largely accepted that integration between health and social care, structural or otherwise, is of primary importance to improve the quality, efficiency and accessibility of health systems for patients. Pim Valentijn and colleagues have helpfully devised a conceptual model of integration that is now widely accepted in research and practice. The Rainbow Model (Valentijn, Schepman, Opheij, & Bruijnzeels, 2013; Valentijn et al., 2019) is invaluable in helping us think about the location, reach and scope of the various integration efforts undertaken in a specific context (see Graphic below).
Yet, there remains an elephant in the room. Whilst scholars of integrated care are designing ever more sophisticated studies to implement, support and evaluate collaborative practices between teams, organisations or care sectors, integration is pursued by and large without knowing what it would look like if it were achieved one day. In other words, measuring integrated care remains difficult (Bainbridge, Brazil, Ploeg, Krueger, & Taniguchi, 2016; Ridgely et al., 2020).
A brief search on conventional data bases reveals why that is the case. Integration is supposed to overcome fragmentation of systems, organisations or teams, yet there is no research on how to measure fragmentation itself. Whilst there is some research on care fragmentation and a considerable literature on continuity of care, there has been no systematic attempt to measure fragmentation in our health systems, between providers or between professionals.1 We all seem to know that fragmentation is bad for everyone involved but we are much less certain what the state of play is in our health systems. Since the old adage is still true that ‘what gets measured gets managed’, it seems to me that care integration remains the ‘unmanaged condition’ of our health systems.
Source: Valentijn et al. (2013) (CC by 3.0).
This is surprising given that it appears sensible to assume that health service outcomes for patients would benefit from improved collaboration between everyone working in health and social care. Care pathways routinely cross several professional and provider boundaries and patient organisations have long pointed to the fragmented and disrupted nature of care journeys for patients with multiple morbidities or chronic conditions. Our lack of ability to measure what we are trying to overcome, that is, service fragmentation, seems astonishing in this respect.
In this collection of papers, I will try to find an answer to the question why we are struggling to achieve integrated care. Throughout the book, I have employed what I would call a magpie approach. I will deliberately step out of the conventional boundaries of health science research and try to ‘think outside the box’. The result is an unashamedly multidisciplinary (if not interdisciplinary) take on what integrated care is and how we can investigate it. Borrowing from organisational sociology, social action theory and political theory, I will argue, helps us give a more a holistic picture of integration to do justice to what is, after all, a complex change phenomenon in public facing services. Using this eclectic approach, I am convinced, will reveal the blind spots in our research, including a striking absence of research about how integrated care as a policy ‘solution’ is formulated through the work of national, regional or local policy networks (for an exception see Martens et al., 2021).
In addition, using the concept of liminality and others, the chapters will throw a light on the profound transformation for staff, teams and departments which occurs whenever integrated care working is advocated and implemented, often leading to significant local resistance, rejection, if not sometimes failure of integrated care programmes. Finally, and crucially, the papers collected here may tell us more about the tacit assumptions that underpin care integration. One of these assumptions is that integration symbolises an unqualified value for everyone involved. This largely untested assumption, I will argue, is little more than a slogan and blinds us to seeking pragmatic patient focussed solutions manifesting real progress (Kaehne, 2019; Russell, Greenhalgh, Byrne, & McDonnell, 2008).
Some of the papers collected in this book have previously appeared in slightly different form in the Journal of Integrated Care. I am grateful to Emerald Publishing to permit their inclusion here. Last but not least, I want to say a big ‘thank you’ to my colleagues at the Department of Health and Social Management at the University of Eastern Finland, Kuopio, who have provided me with a visiting professorship in recent years which gave me the time and space to write some of the chapters and papers brought together in this volume. I am deeply indebted to them for the many discussions we had on integrated care and so much more.
NOTE
1. NHS England are currently undertaking some work to design an Integration Index measuring patient perceptions of integrated care. The work was not completed at time of writing (January 2022).
REFERENCES
Bainbridge, D., Brazil, K., Ploeg, J., Krueger, P., & Taniguchi, A. (2016). Measuring healthcare integration: Operationalization of a framework for a systems evaluation of palliative care structures, processes, and outcomes. Palliative Medicine, 30(6), 567–579. https://doi.org/10.1177/0269216315619862
Hughes, G., Shaw, S. E., & Greenhalgh, T. (2020). Rethinking integrated care: A systematic hermeneutic review of the literature on integrated care strategies and concepts. The Milbank Quarterly, 98(2), 446–492.
Kaehne, A. (2019). Response to ‘values of integrated care: A systematic review ’ by Nick Zonneveld et al. International Journal of Integrated Care, 19(3), 1–2.
Martens, M., Danhieux, K., Van Belle, S., Wouters, E., Van Damme, W., Remmen, R., & Van Olmen, J. (2021). Integration or fragmentation of health care? Examining policies and politics in a Belgian case study. International Journal of Health Policy and Management, 1–14. https://doi.org/10.34172/ijhpm.2021.581
Oelke, N. D., Suter, E., da Silva Lima, M. A. D., & Van Vliet-Brown, C. (2015). Indicators and measurement tools for health system integration: A knowledge synthesis protocol. Systematic Reviews, 4(1), 4. https://doi.org/10.1186/s13643-015-0090-7
Ridgely, M. S., Buttorff, C., Wolf, L. J., Duffy, E. L., Tom, A. K., Damberg, C. L., … Vaiana, M. E. (2020). The importance of understanding and measuring health system structural, functional, and clinical integration. Health Services Research, 55(S3), 1049–1061. https://doi.org/10.1111/1475-6773.13582
Russell, J., Greenhalgh, T., Byrne, E., & McDonnell, J. (2008). Recognizing rhetoric in health care policy analysis. Journal of Health Services Research and Policy, 13(1), 40–46. https://doi.org/10.1258/jhsrp.2007.006029
Stokes, J., Struckmann, V., Kristensen, S. R., Fuchs, S., van Ginneken, E., Tsiachristas, A., … Sutton, M. (2018). Towards incentivising integration: A typology of payments for integrated care. Health Policy, 122(9), 963–969. https://doi.org/10.1016/j.healthpol.2018.07.003
Suter, E., Oelke, N., Adair, C., & Armitage, G. (2009). Ten key principles for successful health systems integration. Healthcare Quarterly, 13, 16–23. https://doi.org/10.12927/hcq.2009.21092
Valentijn, P. P., Pereira, F., Sterner, C. W., Vrijhoef, H. J. M., Ruwaard, D., Hegbrant, J., & Strippoli, G. F. M. (2019). Validation of the rainbow model of integrated care measurement tools (RMIC-MTs) in renal care for patient and care providers. PLoS ONE, 14(9), 1–21. https://doi.org/10.1371/journal.pone.0222593
Valentijn, P. P., Schepman, S. M., Opheij, W., & Bruijnzeels, M. A. (2013). Understanding integrated care: A comprehensive conceptual framework based on the integrative functions of primary care. International Journal of Integrated Care, 13, e010.
![]()
2
THE FUTURE OF INTEGRATED CARE
As the corona virus spread around the world, one could have been forgiven to think that the pandemic would be a prima facie case for integrated care. Where health systems need to rapidly respond to epidemics their strengths and weaknesses are laid bare. In the case of COVID-19, it was intensive care unit (ICU) beds that were required in much larger numbers than normally. Some countries responded well to the crisis. In this early phase, Germany, with a larger than usual number of (admittedly expensive) hospital beds activated its containment plans early and, ultimately, suffered about 8,000 deaths from COVID-19, whilst the UK reached, as of mid-June 2020, the staggering number of 41,000 deaths. The disparities may be illustrative of a chasm in how well health systems were prepared. But there may be other factors at play as well.
In this brief first chapter, I want to set the scene for the subsequent sections of the book. In particular, I will try to sketch the main challenges that have emerged in our health systems in the last couple of years. Undoubtedly, pandemics and the threats to public health are some of the challenges but they are occurring simultaneously to the enormous transformation in health monitoring behaviour by patients is under way and I am not convinced we have yet grasped the magnitude of this fundamental change. First, I will try to define how COVID and health system responses to it has thrown into disarray the way we conceive of, plan and research integration in health and social care. In the second part of the chapter, I will link this with the developments in health seeking and health monitoring behaviour that is about to shake the foundations of conventional organisation centred change programmes such as care integration.
THE PANDEMIC AND INTEGRATED CARE
As the main emphasis of the public health system response was an increase in ICU capacity, in the UK, politicians and health directors took their eye off...