eBook - ePub
Clinical Lymphatic Mapping in Gynecologic Cancers
- 146 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Clinical Lymphatic Mapping in Gynecologic Cancers
About this book
Lymphatic mapping techniques have proven to be useful to the early detection and safe treatment of endometrial and cervical cancers; however, the techniques have much of value to offer for breast cancer also and particularly for vulvar cancer, where there has been an explosion of interest and research. In the new edition of Clinical Lymphatic Mapping of Gynecologic Cancers, the techniques are fully explained, with consideration of the latest developments and technologies.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Clinical Lymphatic Mapping in Gynecologic Cancers by Charles Levenback, Ate GJ van der Zee, Robert L. Coleman, Charles Levenback,Ate GJ van der Zee,Robert L. Coleman in PDF and/or ePUB format, as well as other popular books in Medicine & Anatomy. We have over one million books available in our catalogue for you to explore.
1 The history of lymphatic mapping: a gynecologic perspective
DOI: 10.1201/9781003255536-1
CONTENTS
Introduction
Cadaver studies of lymphatic anatomy
Halsted model for surgical management of solid tumors
In vivo injection of dyes
Early efforts at sentinel node identification
Progress toward the modern lymphatic mapping concept
Safety and surgical innovation
References
Introduction
In the new millennium, it is commonly believed that the answers to cancer questions will result from innovations in molecular biology that are brought from the bench to the bedside through the work of translational researchers. However, the story of the development of lymphatic mapping serves as a reminder to us that, even now, some advances in cancer care still come from the more traditional routes of careful study of anatomy, clinical observation, and literature research.
The history of the development of lymphatic mapping is also a humbling lesson in how important innovations in medicine can diffuse slowly. The term ‘sentinel node’ was first used in 1960,1 yet even today the full potential of this concept has not been realized. Initial reports of success with the sentinel node concept were largely ignored or misinterpreted. Old ideas can be difficult to abandon, and new ideas are not always what they appear.
The relative infrequency of gynecologic tumors is an additional impediment to the development of lymphatic mapping in our specialty. Fortunately, we can learn a lot from the experience of others in treating more common diseases. I saw the lymphatic mapping procedure for the first time when a patient presented to MD Anderson Cancer Center in 1992 with synchronous primary tumors: a 2-cm squamous cell cancer of the cervix and a thin cutaneous melanoma of the anterior thigh. Standard treatment at the time would have required inguinal, femoral, and pelvic lymphadenectomy that would have surely left the patient with significant lymphedema. After extensive consultation, the surgical oncologist performed lymphatic mapping and sentinel node biopsy. I was amazed to see lymphatic channels and the blue sentinel lymph node. Up to this time any type of preoperative or intraoperative direct imaging of lymphatic channels and lymph nodes was not possible. When I saw the blue node in the groin, it was clear that the same technique could be applied to carcinoma of the vulva.
Since the first edition of this book there has been an explosion in knowledge about patient safety and the risks associated with the introduction of new procedures and medical devices into surgical practice. In this chapter, we will explore lessons learned from the introduction of sentinel lymph node biopsy into gynecologic oncology surgical practice. Subsequent chapters will review the lymphatic anatomy of the female lower genital tract and breast and the current state of knowledge regarding lymphatic mapping for tumors at these sites.
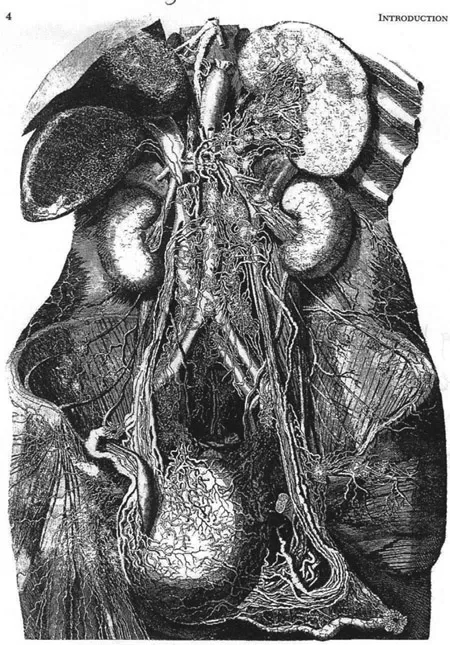
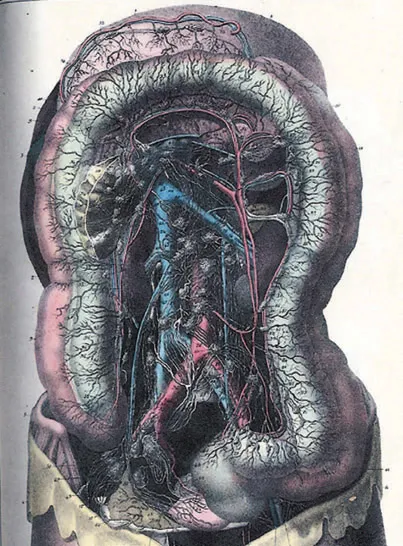
Cadaver studies of lymphatic anatomy
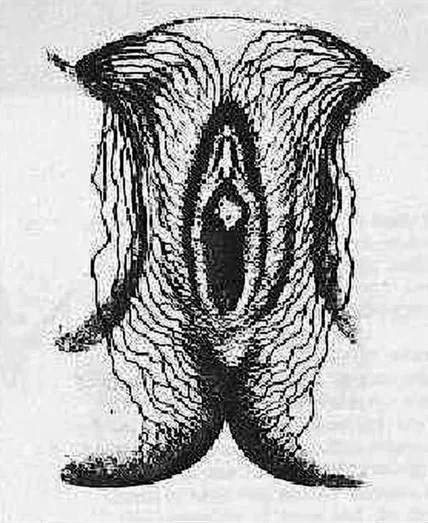
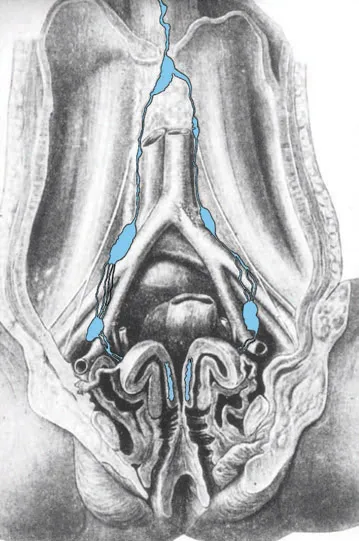
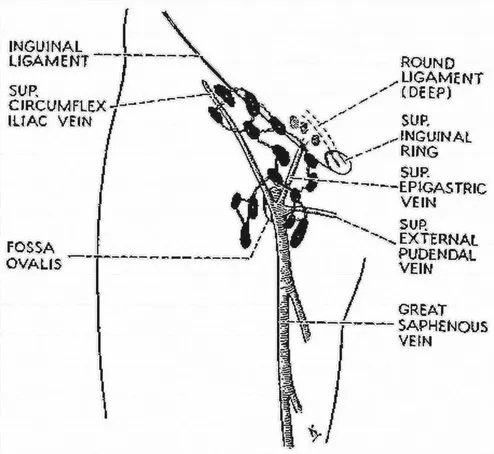
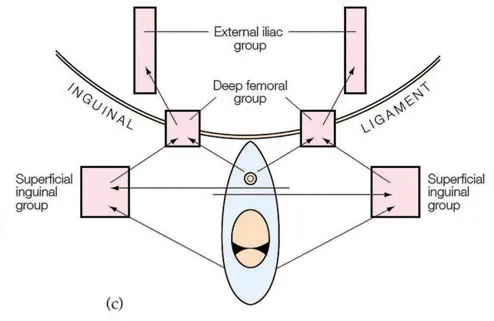
Early anatomists learned about lymphatic anatomy from cadavers. This work was complicated by the fact that lymphatic channels are difficult to see and very fragile and by the fact that tissue had to be extensively putrefied or fixed to be studied. Painstaking dissections led to the production of remarkable drawings of lymphatic anatomy. These illustrations were frequently reproduced by subsequent investigators with small improvements (Figures 1.1 and 1.2). Anatomists developed a variety of aids to help visualize the lymphatic channels, including a number of mercurial compounds that, when injected into various soft tissues, canalized the lymphatics. This technique most likely contributed to the depictions of lymphatic anatomy that erroneously show vulvar lymphatics crossing the labial-crural fold, best represented by Sappey’s illustration (Figure 1.3). In the early twentieth century, the French gynecologists Leveuf and Godard2 studied the lymphatic anatomy of the cervix using injection of Gerotti blue into the cervices of neonatal cadavers. They found that the dye drained in a highly reproducible way to a lymph node usually found in the obturator space or close to the iliac vessels. They named this the ‘principal’ lymph node (Figure 1.4).
Halsted model for surgical management of solid tumors
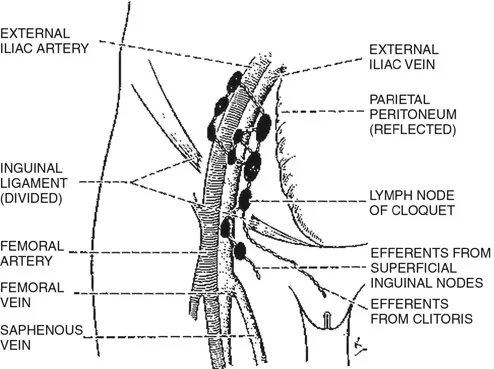
The great anatomist of the second century, Galen, believed that cancer was a local process resulting from a systemic disease of bodily fluids and humors. In the West, this concept was not challenged until the seventeenth century, when Valsalva proposed that cancer spread from primary tumors to lymph nodes.3 This understanding of cancer and the metastatic process ultimately led to the Halstedian model for surgical management of solid tumors. In this model, the primary tumor, the primary regional lymph nodes, and the second-echelon regional nodes, as well as all of the intervening lymphatic channels – including the fine cutaneous lymphatics – were resected en bloc. This approach was integrated into the treatment of gynecologic cancers by several gynecologic surgeons working in multiple sites on the European continent. Rupprecht, Basset, Stoeckel, and Bucura are credited with simultaneous descriptions in 1912 of what we now refer to as radical vulvectomy and bilateral inguinal femoral lymphadenectomy.4 The next generation of gynecologic cancer surgeons, including Twombly,5 Taussig,6 and Way,7 championed radical vulvectomy and bilateral inguinal femoral lymphadenectomy, with only minor revisions for patients with vulvar cancer, because of the dramatic improvement in survival compared with less radical or nonsurgical treatments. Stanley Way summarized the surgical philosophy of the day in 1951 when he stated, “The most important steps in the operation are undoubtedly the very wide removal of the vulva and the resection of the lymph nodes, certainly as far as the node of Cloquet”8 (Figure 1.5). Way added that the morbidity and mortality of the procedure were justified and that the operation “represents the final achievement of surgery in this disease.” Within a generation, however, the radicality of surgical treatment of the vulva would be diminishing, and today, no indications remain for radical vulvectomy and bilateral inguinal femoral lymphadenectomy for the primary treatment of vulvar cancer.
Although Way was incorrect in his assessment, he did make a prophetic plea for the establishment of special treatment centers for patients with vulvar cancer because of its rarity, the difficulty of radical surgery for vulvar cancer, and the need for experienced medical and nursing care. Way foreshadowed both the formation of the subspecialty of gynecologic oncology and the establishment of comprehensive cancer centers.
In vivo injection of dyes
The next advances in the study of lymphatic anatomy and the development of lymphatic mapping came from in vivo studies. Intraoperative observation of the lymphatics has always been hampered by two facts: The lymphatics are essentially invisible, and the lymph is colorless. Two of the first investigators to use living subjects for study were Stephen Hudack and Phillip McMaster.9 ...
Table of contents
- Cover
- Half Title
- Title
- Copyright
- Dedication
- Contents
- List of contributors
- Preface
- 1 The history of lymphatic mapping: a gynecologic perspective
- 2 Lymphatic anatomy: microanatomy and physiology
- 3 Lymphatic anatomy: lymphatics of the vulva
- 4 Lymphatic anatomy: lymphatics of the cervix
- 5 Lymphatic anatomy: lymphatics of the uterus
- 6 Lymphatic anatomy: lymphatics of the ovary
- 7 Lymphatic anatomy: lymphatics of the breast and axilla
- 8 Modalities of detection of sentinel nodes in lymphatic mapping
- 9 Ultrastaging of the sentinel node
- 10 Sentinel lymph node biopsy of the vulva
- 11 Sentinel lymph node mapping in cervical cancer
- 12 Sentinel lymph node mapping in breast cancer
- 13 Sentinel lymph node biopsy of the endometrium
- 14 Impact of sentinel lymph node mapping on quality of life
- 15 Radiation oncology considerations
- 16 Special considerations
- 17 Clinical trial design
- Index