- 220 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Spine Surgery Vivas for the FRCS (Tr & Orth)
About this book
Up to date and evidence-based answers to a wide range of spinal surgical questions that could be asked in the FRCS (Tr & Orth) Viva exam. Using a clear, case-based structure key points emphasise the core information that will improve the performance of every surgical in training.
Sections cover all the key areas of Trauma, Degenerative spinal pathology, Spinal cord injury, Spinal deformity, Primary bone tumours, Metastatic disease, Paediatric spinal surgery, Basic sciences, and other topics.
Suitable for use by trainees at all levels in orthopaedic surgery and neurosurgery, both in the UK and internationally, and those with aninterest in spinal surgery.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Spine Surgery Vivas for the FRCS (Tr & Orth) by Kelechi Eseonu,Nicolas Beresford-Cleary in PDF and/or ePUB format, as well as other popular books in Medicine & Medical Theory, Practice & Reference. We have over one million books available in our catalogue for you to explore.
Information
SECTION 1TRAUMA
1TRAUMATIC OCCIPITO-CERVICAL INSTABILITY
DOI: 10.1201/9781003201304-2
You are asked to see a 34-year-old female with Down’s syndrome. She presents with a 4-month history of progressive neck pain, bilateral impairment of fine motor dexterity of the hands and difficulty walking due to gait instability.
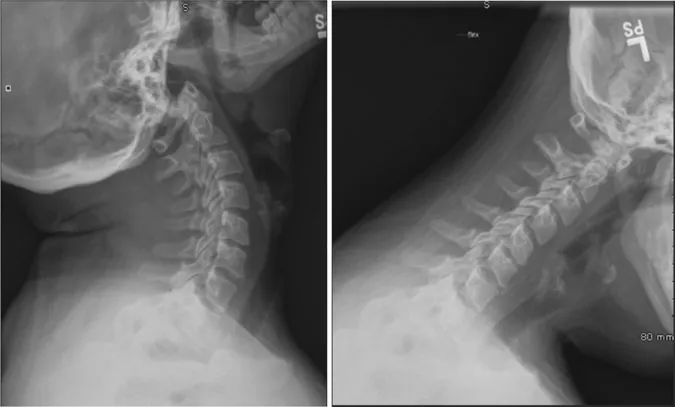
Lateral and anteroposterior (AP) plain radiographs and a computed tomography (CT) scan of the cervical spine were performed.
Q: What is the most likely diagnosis?
This patient has an acquired occipitoaxial dislocation. This is a rare diagnosis but is most seen in patients with Down’s syndrome. It is most commonly asymptomatic but can be associated with pain or neurological compromise. It is classically caused by bony dysplasia or ligament and soft tissue laxity.
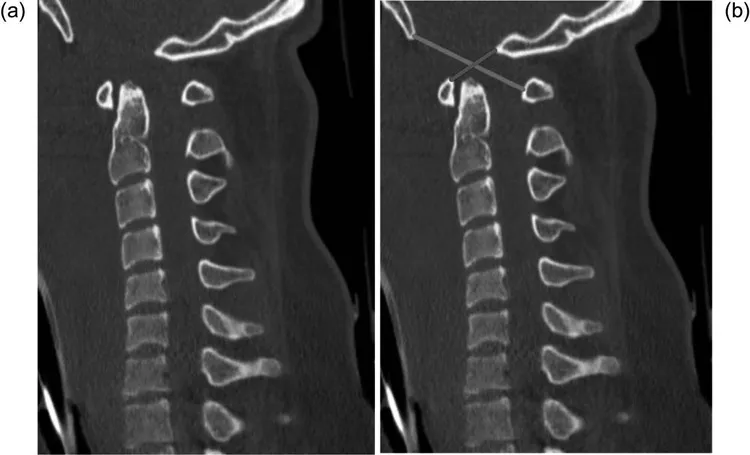
Plain radiographs have low sensitivity (57%) in detecting occipito-cervical (OC) injury and/or instability. The diagnosis can be most easily made using a sagittal CT scan of the cervical spine (Figure 1.2).
The power’s ratio is the ratio of the distance from the posterior arch of the C1 vertebra to the basion (yellow line) divided by the distance from the anterior arch of C1 to the opisthion (red line; Figure 1.2b). A ratio of around 1 is normal. Greater than 1 indicates a possible anterior dislocation and should be correlated with the clinical presentation. A ratio of significantly less than one is indicative of an atlas (C1) ring fracture, posterior atlanto-occipital dislocation or odontoid fracture.
It can be classified according to the Traynelis classification:
- Type I—Anterior occiput dislocation
- Type II—Longitudinal dislocation
- Type III—Posterior occiput dislocation
Acquired OC instability is distinct from traumatic OC dislocation—a rare injury associated with high-velocity trauma, a high incidence of associated neurological and vascular injury. It is identified in 19% of fatal cervical injuries but has become more commonly seen clinically due to improved techniques in resuscitation and imaging.
Q: How should this patient be managed?
The patient should have a detailed neurological examination and the cervical spine should be immobilised in a cervical collar if there is any history of trauma. In the presence of lowor high-energy trauma, other cervical fractures should be carefully excluded.
OC dissociation or dislocation requires urgent consult with a specialist spinal surgeon.
Q: Which other diagnostic imaging is required?
Cervical spinal magnetic resonance imaging (MRI) scan is indicated in the presence of neurological deficit. It can identify cervical disc herniation, spinal cord or nerve root compression. It can also be useful in the exclusion of ligamentous injury with preserved alignment or occult injury in the presence of possible trauma.
Q: What is the definitive management for this patient?
Surgical stabilisation is indicated for acquired OC dislocation with evidence of myelopathy or symptomatic neck pain.
This can be performed via posterior OC fusion via a midline posterior approach to the base of the skull (Figure 1.3). The patient should be positioned prone with the cervical spine securely immobilised. Fixation can be achieved via a rigid OC screw-rod or plate construct. Traction has been reported to worsen neurological compromise and so should not be attempted.

Major structures at risk include the dural venous sinuses, internal carotid artery and the vertebral artery (which runs cranially through the transverse foramen of the C2–6 vertebrae).
Exam Tips
- This is a rare condition and therefore infrequently tested. However, a working knowledge of the atlantoaxial ligamentous anatomy, as well as of the diagnosis of instability of the occipitoaxial and atlantoaxial joints is essential in clinical practice and may be covered. Note that other causes of instability in this area include tumour, trauma and inflammatory conditions, such as rheumatoid arthritis, and these should be included in differential diagnosis.
- Remember to mention the use of Advanced Trauma and Life Support (ATLS) guidelines with any history of even minor trauma and high cervical instability!
- You should be aware of the differences between acquired and traumatic OC instability/dislocation. A detailed discussion of the surgical management of either of these is beyond the level expected of the FRCS examination.
SUGGESTED READINGS
- Radcliff K, Kepler C, Reitman C, et al. CT and MRI-based diagnosis of craniocervical dislocations: the role of the occipitoatlantal ligament. Clin Orthop Relat Res. 2012;470(6):1602–13.
- Panjabi M, Dvorak J, Duranceau J, et al. Three-dimensional movements of the upper cervical spine. Spine (Phila Pa 1976). 1988;13(7):726–30.
2ATLAS FRACTURE
DOI: 10.1201/9781003201304-3
Q: A 45-year-old male presents to the emergency department having fallen and landed directly on his head from 2m. He suffers a concussion and complains of neck pain. Following initial assessment, he undergoes trauma CT. Please comment on this finding:
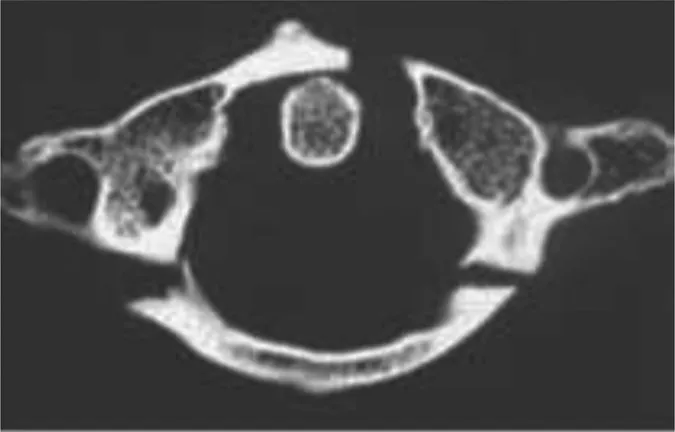
This is an axial image showing a fracture of the C1 ring. There are fractures to the anterior and posterior arches. This is a ‘burst’-type injury usually because of axial loading. The eponymous name for this fracture is a Jefferson fracture.
Q: Are there any other subtypes of this fracture of which you are aware?
Gehweiler classified these fractures into 5 subtypes. Type 1 and 2 are fractures to the anterior and posterior arches and tend to be caused by hyperflexion and hyperextension mechanisms, respectively. Type 3 injuries are injuries to the anterior and posterior arches as demonstrated in this case and are sub-classified into type 3a or 3b depending upon the integrity of the transverse atlantal ligament (TAL). Type 3a injuries (intact TAL) are considered stable and type 3b injuries unstable. In type 4 injuries, the fracture extends into the lateral mass, and type 5 injuries involve the transverse process and foramen. In type 5 injuries, careful assessment with CT angiogram (CTA) should be undertaken as the vertebral artery is at risk. Most of these fractures are stable and can be managed non-operatively in a cervical orthosis.
Q: How would you assess this injury?
The stability of this type 3 injury needs to be determined and depends on the integrity of the TAL, the primary stabiliser of the upper cervical spine at the atlantoaxial junction. Spence et al. suggested that instability is indicated if the lateral mass offset—the distance between the lateral masses of C1 and C2—on an open-mouth Antero-Posterior (AP) X-ray (XR) exceeded 6.9mm2, although this value has since been shown not to correlate well with TAL integrity and should be used only as a guide for assessment. Assessment on the lateral XR is by assessment of the atlanto-dens interval (ADI). This is the distance between the anterior arch of the atlas and the dens. Normally this should be <3mm and exceeding this may indicate TAL rupture.
To fully assess the integrity of the ligament, I would obtain an MRI scan. Type 3a injuries, according to the Geweiler classification, are those with an intact transverse ligament, are inherently stable, and can be managed with a cervical orthosis. However, if the ligament is ruptured this may confer instability and as such may require stabilisation.
Q: The MRI shows mid-substance disruption of the transverse ligament. How do you proceed?
This indicates that...
Table of contents
- Cover
- Half Title
- Title
- Copyright
- Contents
- Preface
- Section 1: Trauma
- Section 2: Degenerative Spinal Conditions
- Section 3: Spinal Cord Injury
- Section 4: Spinal Deformity
- Section 5: Primary Tumours
- Section 6: Metastatic Spinal Tumours
- Section 7: Paediatric Spinal Surgery
- Section 8: Infection
- Section 9: Other Useful Cases
- Things You Should Know!
- Index