![]()
V The Operating System of Patient Safety
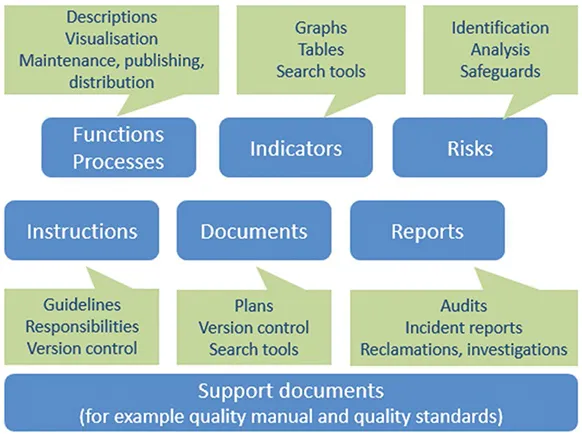
The Contents of the Operating System
The patient safety operating system is a description of an organisation’s – or one of its unit’s – procedures and of the requirements attached to them. It is intended for enabling and ensuring the implementation and monitoring of patient safety strategies. The operating system gives answers to the following questions:
- How to lead the operations; who leads them, and with what tools?
- How to set requirements and standards for operations?
- How to set goals for operations?
- How to organise operations?
- How to organise communications and relations to patients and their next of kin, partners, and interest groups?
- How to ensure accountability and continuity?
- How to measure and evaluate operations?
- How to improve operations?
- How to carry out management reviews?
- How to evaluate and improve the operating system?
A well-organised operating system offers a model for setting and achieving organisational targets and goals. It is a tool for managing and developing an organisation and its processes, personnel, partnerships, and resources. From a learning point of view, the operating system can offer means of sharing good practices, information, and experiences; it can also serve as an instrument for involving temporary workers and partners. It can be likened to an organisation’s collective memory describing the agreed ways of acting. The operating system makes it possible to maintain a situational picture of the implementation and impact of agreed measures.
The basic requirement for patient safety is that the operating system is a part of day-to-day management. As the next figure shows, the executive group must discusspatient safety regularly, not postpone it until later, or, worse still, swipe it under the carpet.
Figure 23. The operating system of patient safety
It is a dangerous misconception that development work, for example, automatically improves patient safety. Changes will probably create new risk scenarios with new threats, which requires a patient safety point of view to decision-making. Moreover, patient safety should not be someone’s part-time responsibility that takes second place to the primary responsibilities of that person.
Patient Safety Plan
Legal acts require that healthcare providers have a plan on quality management, and on implementing patient safety. Many organisations only speak about a patient safety plan. That plan is a strategy and policy document that, when completed, often gives a great feeling of satisfaction. However, consistent actions to implement that plan fall short, and people start micromanaging and coping with isolated cases.Furthermore, the plan is not always updated to form an annual plan describing the detailed measures to maintain and improve patient safety over a period of one year.
An operating system including a plan creates a procedure that best systematises practices and ensures continuity. It enables setting and achieving goals; it also enables and builds the foundations for effectiveness assessment, operations management, and continuous improvement. An operating system maintains the situational picture of patient safety. By acting in a planned and structured manner, it will be possible to keep the focus on proactive actions, not on after-care and statistics. The basic structure is as follows:
- Policy and management
- Planning
- Implementation, monitoring the situational picture, and support for activities
- Operation, control, and corrective actions
The next sentence may seem complicated, but it includes a simple idea of a plan. When we have planned and decided what we will do, we must do what we wrote we would do, the way we wrote we would do it. Next, we must check if we did what we wrote we would do. If not, what happened, why it happened, and what we must do to learn from it and to avoid repeating the same mistake. Lastly, we must check the whole cycle and decide if it needs changing.
Next, we will present two mission models that combined with a vision form the basis of a plan.
Example 1
We work proactively to recognise and control risks, instead of just being reactive and putting out occasional fires. We want to control risks proactively to achieve interruption-free operations without hazardous events and harms, as intended in our operative and economic plans, and we want to increase client satisfaction and strengthen relations to the surrounding society.
We want to continue learning from our own and from others’ experiences, so as not to repeat mistakes. We want to learn from the results of audits andmanagement reviews, so that we can efficiently control risks and make continuous improvements.
We are consistent in our actions. We want to have a consistent approach to risk management in different processes and operations. This prevents confusion, increases effectiveness, saves time, and reduces costs.
We are cyclical in our actions. Risk management is an ongoing process. We need a cyclical risk management process to reach our present aims. We continuously update our knowledge and approaches.
We are reviewable. By taking the previous steps, we can prove we have a predictable, coherent management system that keeps people safe and sound, protects the environment, and respects the community we work in.
Example 2
According to the mission of the Hope Hospital, the operative goals are:
- Ensuring safe and high-quality care experiences for the patients
- Working towards economic efficiency, high performance, and high quality
- Strengthening of service image
- Strengthening of professional skills and well-being at work among staff
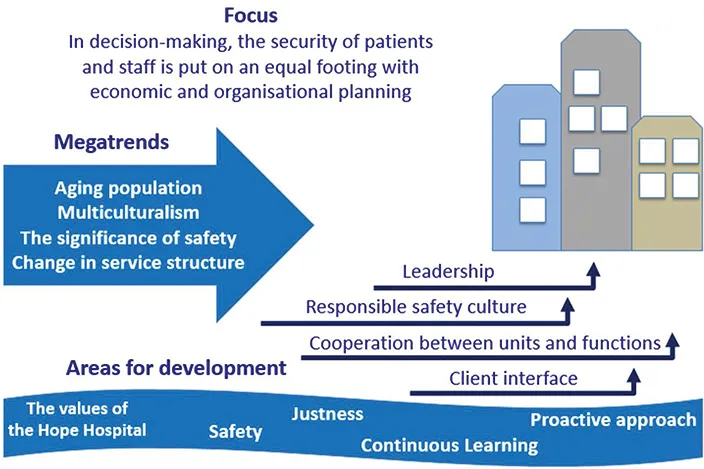
Patient safety is part of good care in the Hope Hospital; it covers the areas of research, care, and medical device safety. The personnel, the patients, and their next of kin have patient safety as a common goal. It means that the patients suffer no harm during their care and feel safe at all stages. Work on patient safety is part of the Hope Hospital’s quality management system. The objectives and ways of organising patient safety work are described in the patient safety plan.
A proactive patient safety culture in which operations are evaluated on a regular basis is at the heart of patient safety work; it is also based on shared values and operational principles. To maintain and promote a good patient safety culture, the Hope Hospital improves its work community’s ability to work for patient safety. That ability includes the elements of knowhow, organisation of work, equipment, teamwork skills, and feel for work.
Those working in the Hope Hospital commit themselves to following the values of patient safety:
- The objective of no harm: every mistake can be prevented.
- It is the attitude that matters: every task is carried out in a way that ensures safety and the correct identification of a patient.
- We shall value the culture of accountability: no compromises are made in safety matters. Instructions and agreed procedures are followed to a tee.
- We will not repeat the same mistakes: mistakes and close calls are always reported, and lessons are learned.
Figure 24. The Hope Hospital’s vision of patient safety
We who work at the Hope Hospital collect information on the patient safety situation in a continuous, proactive, and comprehensive manner. To facilitate management decisions, we use that information to form a situational picture of patient safety. Information gathering has been organised in a way that builds a proactive protection against risks and safety hazards. Actual deviations that have causedadverse events or harm are reported and analysed, and guidance is provided effectively, so that the incidents do not recur. Incident reports and investigations aim at serving organisational learning and protecting patients’ rights. The realisation of patient safety goals and principles is measured and assessed on a continuous basis.
Managing Functional Risks
Risk management is an activity that cuts across all cultural contents of an organisation. It does not pertain solely to safety, although these two things are closely interrelated. An organisation can face strategic, operational, or economic risks, or the risk of damage. Those risks can be internal or external in nature. Strategic risks prevent organisations from reaching their strategic goals. They often arise from external events and changes pertaining, for example, to demand, legislation, or reputation management. Economic risks are linked to internal or external economic or financial matters. Damage risks are caused by unexpected and sudden events that may result in an accident, equipment failure, or liability. These events are often insurable.
Operational risks stem from the daily functions of an organisation. They are caused by inadequate or failed internal processes, personnel, systems, or external factors. Operational risks can be divided into subcategories relating to management, patient care, personnel, and support services. In addition, an organisational and safety culture where there is resistance to change could also be categorised as an operative risk. It plays a role in operational risks but can materialise in other risk categories as well.
Risks are often interrelated. Materialised information management risks may lead to chains of events that result in accidents, or they may compromise patient safety. This may trigger economic or business image risks. An overly narrow safety perspective, for example, may pose challenges in terms of an organisation’s overall performance. Unsuccessful or non-existing risk management leads to poor quality costs, to say the least. Those costs eat up scarce economic resources and take their toll on well-being at work. Risk management is an important tool in reachingorganisational goals. When it comes to patient safety, risk management is a vital prerequisite for meeting client value propositions.
Proactiveness, situational awareness, and risk management concern everyone. An important practical observation is that to minimise care-related risks, steps should be taken to improve the involvement, awareness, and vigilance of patients and their next of kin as well.
When training people in different organisations, we have noticed that it is exceedingly difficult to motivate them to make risk assessments. It may be considered yet another bureaucratic way of reducing patient time. On the other hand, when having drills in real situations where it has been possible to assess the impact of risk assessments, the participants have often been pleasantly surprised.
Proactiveness and situational awareness are the basic principles in working towards zero harm. Proactiveness means continuous assessing of activities, analysing risks, and taking precautions against those risks. Situational awareness means that we recognise the incidence, quality, and significance of minor, often non-physical, adverse events.
Zero Harm: Is It Possible?
Anticipation is the most important step towards improved safety. Looking back through statistics, you may deem the zero-harm goal impossible. Errors, and subsequent adverse events, really do occur – in excess. The prevailing situation is also too often played down. When adverse events are presented statistically, the centre of attention is on how few and far between these events are, considering thesize and scope of the activities. In statistical analysis, percentages are often used, and results are presented in the form of Excel tables.
From a patient safety perspective, it would be useful to examine the same events in numbers. It is a completely different thing to read or hear that our actions have caused significant harm to ten people than to express the same thing as a percentage of visits. The way we use language also reinforces the way we think. An error is often hidden behind the word ‘complication’. There are many common phrases that support the thought ‘accidents will happen’: to err is hu...