- 944 pages
- English
- PDF
- Available on iOS & Android
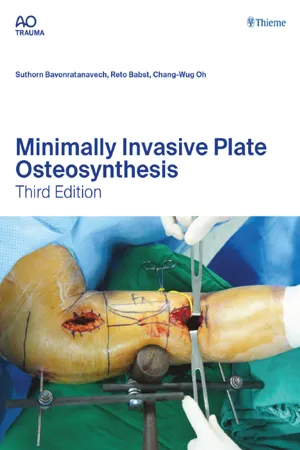
Minimally Invasive Plate Osteosynthesis
About this book
FOUR STARS from Doody's Star Ratings™
A practical hands-on manual for surgeons of all levels, the Minimally Invasive Plate Osteosynthesis, Third Edition is a crucial guide to managing fractures using the minimally invasive plate osteosynthesis technique. Expanding on the foundations set by the previous editions, this new issue will be of substantial value to any surgeon, boosting excellent fracture healing and functional outcomes, while minimizing complications.
The minimally invasive surgical techniques are presented in a systematic, case-based format covering fractures of the upper and lower extremity and pelvic/acetabular injuries. This new third edition provides step-by-step coverage on managing a broad spectrum of injuries from acute fractures to nonunion/malunion. While a single case can be approached through various methods, this new book seeks to impart fundamental guidelines and indications for applying minimally invasive procedures.
New third edition focuses on:
- General principles in minimally invasive plate osteosynthesis
- Clinical and radiographic evaluation
- Decision-making and options
- Preoperative planning
- Surgical approaches
- Tips and pitfalls to avoid complications
- Postoperative rehabilitation
Key features include:
- Contributions from 68 expert surgeons from 14 countries
- More than 50 cases on a comprehensive range of fractures
- More than 487 high-quality illustrations and 2647 images
Tools to learn more effectively

Saving Books

Keyword Search

Annotating Text

Listen to it instead
Information
Table of contents
- Minimally Invasive Plate Osteosynthesis
- Title page
- Copyright
- Table of contents
- Foreword
- Preface
- Acknowledgment
- Contributors
- 1 History and evolution of minimally invasive plate osteosynthesis
- 2.1 Basic mechanobiology of bone healing and biomechanics of fracture fixation
- 2.2 Cerclage wiring as a reduction technique
- 3 Instruments
- 4 Implants
- 5 Intraoperative imaging
- 6 Reduction techniques
- 7 Decision making and preoperative planning
- 8 Preoperative and postoperative management
- 9 Complications and solutions
- 10 Minimally invasive plate osteosynthesis and evidence-based medicine
- 11.1 Clavicle: introduction
- 11.2 Clavicle: bilateral comminuted diaphyseal fractures—15.2C
- 11.3 Clavicle, shaft: fragmentary spiral fracture—15.2C
- 11.4 Clavicular fracture—15.2C
- 11.5 Clavicle, shaft: long oblique fracture—15.2A
- 12.1 Scapula: introduction
- 12.2 Scapula: MIPO case
- 12.3 Scapula: minimal invasive scapula fixation
- 13.1 Humerus, proximal: introduction
- 13.2 Humerus, proximal: extraarticular fracture—11A3
- 13.3 Proximal humeral shaft fracture with extension into the humeral head—12B2.1
- 13.4 Humerus, proximal fracture 4-part, valgus malalignment—11C
- 14.1 Humerus, shaft: introduction
- 14.2 Humerus, shaft: wedge fracture, bending wedge—12B2
- 14.3 Distal one-third fracture of humerus: multifragmentatry fracture—12B3
- 14.4 Humerus, shaft: complex fracture, irregular—12B3
- 14.5 Humerus, shaft: lower third—12B
- 15.1 Forearm: introduction
- 15.2 Forearm—multifragmentary proximal one-third ulnar fracture (Monteggia fracture)—2U2B3.a
- 15.3 Forearm: diaphyseal fractures
- 15.4 Forearm: comminuted distal one-third radial fracture (Galeazzi fracture)—2R2B3 (g)
- 15.5 Forearm: distal radial fracture with dislocation—2R3B2.3
- 16.1A Pelvic ring fractures
- 16.1B Acetabular fractures
- 16.2 Unstable 61C pelvic ring injury in an elderly patient with complete and bilateral posterior and anterior fractures
- 16.3 Pelvis, acetabulum: a displaced high anterior column fracture of the left acetabulum—62A3
- 16.4 Pelvis, acetabulum: minimally displaced left anterior column posterior hemitransverse acetabular fracture—62B2, and associated right pelvic ring injury with right sacral fracture and bilateral superior and inferior rami fractures—61B2
- 16.5 Pelvis, acetabulum: both-column acetabular fracture—62C1
- 17.1 Femur, proximal: introduction
- 17.2 Femur, proximal: extraarticular fracture, intertrochanteric—31A3
- 17.3 Femur, proximal: extraarticular fracture, trochanteric area pertrochanteric simple—31A1
- 17.4 Femur, subtrochanteric, multifragmentary—32B3.1
- 17.5 Femur, proximal: extraarticular fracture, intertrochanteric—31A3 and wedge subtrochanteric fracture—32B2.1
- 18.1 Femur, shaft: introduction
- 18.2 Femur, shaft: wedge fracture, fragmented wedge—32B3
- 18.3 Femur, shaft: wedge fracture, comminuted wedge—32B3
- 18.4 Femur, shaft: segmental fracture—32C2
- 19.1 Femur, distal: introduction
- 19.2 Femur, distal: periprosthetic fracture—V.3-B1
- 19.3 Femur, distal: intraarticular fracture—33C2
- 19.4 Femur, distal: intraarticular simple fracture—33C1
- 19.5 Femur, distal: intraarticular fracture—33C3
- 19.6 Femur, distal—33C3
- 20.1 Tibia and fibula, proximal: introduction
- 20.2 Tibia and fibula, proximal: metaphyseal simple fracture—42A2
- 20.3 Tibia and fibula, proximal: intraarticular bicondylar fracture with a nonimpacted, metaphyseal component—41C3 with diaphyseal involvement
- 20.4 Tibia and fibula, proximal: intraarticular bicondylar fracture, no metadiaphyseal involvement—41C3
- 20.5 Tibia and fibula, proximal—42A
- 21.1 Tibia and fibula, shaft: introduction
- 21.2 Tibia, shaft: complex fracture—42C3
- 21.3 Tibia and fibula, shaft: simple fracture, transverse—42A2
- 21.4 Tibia and fibula, shaft: wedge fracture, spiral wedge—42B3
- 21.5 Tibia, shaft: complex fracture—42C2
- 22.1 Tibia and fibula, distal: introduction
- 22.2 Tibia and fibula, distal: torsional wedge fracture of the distal tibia with posterolateral articular extension—42B2 in combination with a multifragmentary fracture of the distal fibula—44C2
- 22.3 Tibia and fibula, distal: intraarticular simple fracture of the distal tibia—43C1 with simple fracture of the distal fibula
- 22.4 Tibia and fibula, distal: intraarticular complex fracture of the distal tibia—43C3 with simple fracture of the distal fibula
- 22.5 Tibia and fibula, distal: extraarticular multifragmentary distal tibial fracture—43A3 in combination with a multifragmentary distal fibular fracture
- 23.1 Calcaneus: introduction
- 23.2 Bilateral calcaneal fracture—82B1 (tongue type), Sanders type II
- 23.3 Displaced, intraarticular calcaneal fracture—82C2: surgical treatment with minimally invasive plate osteosynthesis via sinus tarsi approach in Sanders type III fracture
- 24.1 Pediatric fractures: introduction
- 24.2 Tibia and fibula, shaft: simple fracture, oblique—42A3
- 24.3 Tibia and fibula, shaft: simple fracture, transverse—42A3
- 24.4 Femur, shaft: simple fracture, transverse—32A3
- 24.5 Femur, shaft: unstable fracture—32D5.1
- 25.1 Minimally invasive plate osteosynthesis in periprosthetic fracture management
- 25.2 Periprosthetic fracture: total knee replacement case, femur—3[V]B1
- 25.3 Periprosthetic fracture: total hip replacement case—32A1(c)
- 25.4 Periprosthetic fracture: interprosthetic case—32B1(c)
- 26.1 Introduction
- 26.2 MIPO in open fractures
- 26.3 MIPO for deformity or malunion correction
- 26.4 MIPO in limb lengthening
- 26.5 Bone transport over a plate
- 26.6 Use of MIPO in the treatment of nonunion
- 27 Implant removal
Frequently asked questions
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app