![]()
Current Progresses in Methodology in Blood Purification in Critical Care
Suzuki H, Hirasawa H (eds): Acute Blood Purification.
Contrib Nephrol. Basel, Karger, 2010, vol 166, pp 100–111
______________________
Current Progress in Blood Purification Methods Used in Critical Care Medicine
Akira Saito
Division of Nephrology and Metabolism, Department of Medicine, Tokai University School of Medicine, Isehara, Japan
______________________
Abstract
The prognosis of patients with an acute accumulation of pathogenic or toxic substances in their body fluids - a condition that severely affects survival - can be significantly improved by blood purification. The most appropriate blood purification method and the duration for which it should be used must be selected on the basis of efficacy and cost. Several blood purification techniques - such as hemodialysis (HD), hemofiltration (HF), hemodiafiltration, continuous hemofiltration (CHF), hemadsorption and plasma exchange - have been developed. Each modality has different removal capacities and limitations; therefore, it is necessary to thoroughly evaluate the time and the duration of use in the case of different disease conditions. The survival rate of patients treated with HF with 35 ml/min of average filtrate is higher than that observed after conventional HD. In patients with systemic inflammatory response syndrome and multiple organ dysfunction syndrome, proinflammatory cytokines should be removed by HF or CHF, as should the toxins accumulated in the original disease. Thus far, no ideal filter has been developed for the removal of a considerable amount of proinflammatory cytokines with minimal albumin loss. In the case of acute liver failure, ammonia, amino acid metabolites and albumin-binding bilirubin should be removed by a combination of HF and plasma exchange. The use of fresh frozen plasma as a replacement fluid in plasma exchange is also important in order to replenish the deficient coagulation factors and essential metabolic factors. Activation of tissue/organ regeneration by the removal of pathogenic factors or by the substitution of factors essential for regeneration might be important in the case of multiple organ dysfunction syndrome. In critically ill patients with composite conditions, the use of more than two blood purification techniques at the same time or at different times during the course of the diseases can improve patient prognosis more than the use of single methods.
Copyright © 2010 S. Karger AG, Basel
During the Second World War, Kollf et al. [1] succeeded in saving an acute renal failure patient with Crush syndrome using hemodialysis (HD). This was the first time that a renal failure patient was kept alive by treatment using blood purification. However, after that, patients with acute kidney injury (AKI) were only treated with HD until 1960, when Quinton et al. [2] developed an external permanent shunt, by which a patient could be treated with HD repeatedly. Since 1944, blood purification has been used to treat acutely ill patients in whom pathogenic or toxic substances have acutely accumulated endogenously or exogenously, constituting risk factors for survival; blood purification helps in removing these substances and in maintaining homeostasis of body fluids. Therefore, several blood purification methods - such as HD, hemofiltration (HF), hemodiafiltration (HDF), continuous HF and HDF methods (CHF, CHDF), hemadsorption, plasma adsorption, and plasma exchange (PE) - have been developed and used for treating acutely ill patients. With the exception of the adsorption techniques, these have been developed with advances in membrane technology principally based on a dialysis membrane. Blood purification improves the prognosis of acutely ill patients if the progression of the disease cannot be sufficiently slowed by conventional treatments, such as medication, sufficient nutrition and surgery.
In this paper, I have mainly described blood purification methods used in critical care and mentioned the appropriate method for treating several disease conditions.
Application of Blood Purification in Critical Care
Blood purification treatments, in general, are used in emergency rooms and ICU because critically ill patients are treated using total life support, including extracorporeal circulation. The quick removal of toxic/pathogenic substances by blood purification can improve survival rate or at least ensure that the healing time is shortened compared to that required for conventional treatments. Because each method has a distinct technique for the removal of accumulated substances and improves homeostasis in critically ill patients to different extents, the method that is most appropriate for treatment has to be chosen and used in a timely manner, depending on the condition of the patient.
Continuous Blood Purification
High-volume HF has been used for patients with relatively stable hemodynamic status since HF was applied for the treatment of acutely ill patients [3, 4]. For the past 2 decades, on the other hand, CHF and CHDF - which maintain the hemodynamic status at a more stable level than that of intermittent ones - have also been used for the treatment of critically ill patients because of the risks involved with the use of extracorporeal circulation. Compared to intermittent treatment, continuous treatment is beneficial not only because of its effect on hemodynamic stability but also because of better survival rates and larger total capacity for the removal of the pathogenic and toxic substances and better maintenance of homeostasis in the patients [5, 6]. CHF or CHDF is well used to treat patients with septic shock because of their poor general condition and volume-refractory hemodynamic failure. Patients with severe pancreatitis are also treated mainly with CHF or CHDF because of the hemodynamic instability. CHDF should be selected in the case of patients under severe catabolic stress with remarkably high level of plasma urea nitrogen. HD and HF, on the other hand, are also used in critical-care medicine when there is insufficient manpower to keep patients under continuous observation.
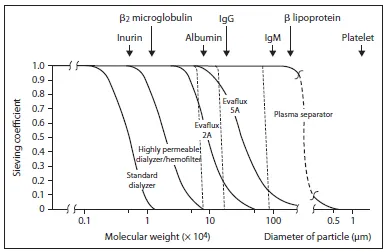
Fig. 1. Five curves for the sieving coefficients of substances with target-molecular-weight ranges filtered across 5 kinds of blood purification membranes: standard dialyzer membrane, highly permeable dialysis/hemofilter membrane, plasma fractionator membranes (such as Evaflux 2A and 5A) and plasma-separator membrane. The sieving coefficients of the target substances were not significantly different from the sieving coefficients of essential substances in the patients. These membranes removed not only toxic and pathogenic substances, but also essential substances to a considerable extent.
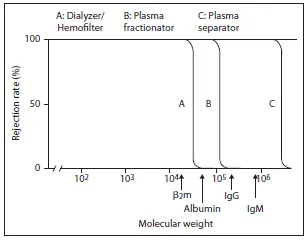
Fig. 2. Ideal blood purification membrane with sharp rejection curves for solutes in 3 molecular-weight ranges. A = β2-microglobulin to albumin; B = albumin to IgG; C = IgM to platelets (as the smallest blood cells). Improvements should be made in these 3 blood purification membranes to remove target molecules more selectively than conventional membranes. A = Dialysis or HF membrane; B = plasma-fractionation membrane; C = plasma-separation membrane.
Systemic anticoagulation is essential while using extracorporeal circulation; therefore, in Japan, nafamostat mesilate is used as an anticoagulant instead of heparin in case the patients develop disseminated intravascular coagulation, a bleeding tendency [7], or hypercoagulation due to continuous heparin loading in the continuous blood purification.
Membranes for Blood Purification
It is necessary to use an appropriate blood purification method that can remove the maximum possible amount of accumulated pathogenic substances and maintain maximum homeostasis. Therefore, the characteristics of the membrane - especially the pore size and biocompatibility - are important factors influencing the performance of the HD, HF, CHF and CHDF techniques [8]. The target molecule is different in each disease; therefore, knowledge of its molecular weight, distribution volume and albumin-binding rate is essential when selecting a blood purification device and modality. Sometimes, a patient with composite complications can have more than 2 pathogenic substances. In a blood purification treatment using a highly permeable membrane as a hemodialyzer or a hemofilter, the rejection rate of the target molecule as well as the protein-binding/total ratio of the molecule is important while selecting the most suitable membrane and treatment modality. Sufficiently sharp rejection curves for solutes have never been obtained while using a conventional dialysis membrane, a highly permeable membrane, a plasma-fractionation membrane and a plasma-separation membrane (fig. 1). Through advances in membrane technology, it is now possible to introduce a big difference between the values for the sieving coefficients (SC) of β2-microglobulin (molecular weight, 11,800 Da) and albumin (molecular weight, 66,800 Da). However, this has not been possible in the case of IL-6 and albumin, though a big difference in SCs between IL-6 and albumin is more important while using CHF and CHDF in critical care medicine. The big difference in the SCs between albumin and immunoglobulin (Ig) G is also important in while using plasma fractionators during PE. Figure 2 shows 3 ideal blood-purification membranes with apparently sharp rejection curves for solutes in 3 different molecular weight ranges. In the figure, A indicates a rejection c...