![]()
Prerenal Azotemia Syndromes
Kellum JA, Ronco C, Vincent J- L (eds): Controversies in Acute Kidney Injury.
Contrib Nephrol. Basel, Karger, 2011, vol 174, pp 33-45
______________________
Cardiorenal Syndrome: A Complex Series of Combined Heart/Kidney Disorders
Ching Yan Goha,c · Grazia Vizzib,c · Massimo De Calb,c · Claudio Roncob,c
aDepartment of Nephrology, Selayang Hospital, Selangor, Malaysia; bDepartment of Nephrology, Dialysis & Transplantation, Ospedale San Bortolo, San Bortolo, and cInternational Renal Research Institute Vicenza (IRRIV), Vicenza, Italy
______________________
Abstract
Over the last decade, it has become increasingly clear that the cardiovascular and renal systems are interdependent. Primary disorders of either system have been shown to disturb the other system. As a result, a class of cardiorenal syndrome (CRS) has been identified wherein a vicious cycle is established in which acute/chronic dysfunction of either the kidney or the heart exacerbates the loss of function in the other organ. The ADQI organization has proposed a classification derived from a consensus conference held in 2008. CRS is classified as a disorder of the heart and kidneys whereby acute or chronic dysfunction in one organ may induce acute or chronic dysfunction in the other. The general definition has been expanded into five subtypes: CRS type 1 = acute worsening of heart function (acute heart failure-acute coronary syndrome) leading to kidney injury and/or dysfunction; CRS type 2 = chronic abnormalities in heart function (chronic heart failure-chronic heart disease) leading to kidney injury or dysfunction; CRS type 3 = acute worsening of kidney function (acute kidney injury) leading to heart injury and/or dysfunction; CRS type 4 = chronic kidney disease (chronic kidney disease) leading to heart injury, disease and/or dysfunction; and CRS type 5 = systemic conditions leading to simultaneous injury and/or dysfunction of heart and kidney. A major problem with previous terminology was that it did not allow for identification of pathophysiological interactions occurring in the different types of combined heart/kidney disorders. The subdivision into different subtypes seems to provide a better approach to this syndrome.
Copyright © 2011 S. Karger AG, Basel
Cardiorenal syndromes (CRS) are broadly defined as conditions characterized by the initiation and/or progression of renal insufficiency secondary to heart failure [1], and it has also been used to describe the negative cardiac effects of declining renal function (renocardiac syndrome) [2]. A recent definition and classification system has been generated to include a vast array of acute or chronic conditions in these two important organs, where the primary failing organ can be either the heart or the kidneys [3]. Such classification has been endorsed and further developed by the ADQI (Acute Dialysis Quality Initiative) consensus group leading to a comprehensive characterization of the complex heart-kidney organ crosstalk [4]. This new classification represents a step forward to a better understanding of the pathophysiology and management strategies of the bidirectional heart-kidney interactions.
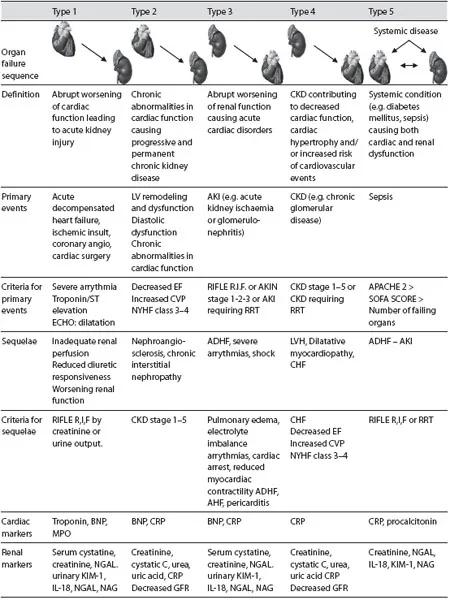
The Definition or Classification of Cardiorenal Syndromes
Any direct and indirect insult to either heart or kidneys can initiate and perpetuate the combined disorder of these two organs through several complex mechanisms. Therefore, ‘cardiorenal syndromes’, a large umbrella term, should be used to describe a series of heart and kidney disorders whereby acute or chronic dysfunction in one organ may induce acute or chronic dysfunction (structural or functional abnormalities) of the other. A more descriptive classification into five different subtypes would permit recognition of the primary organ dysfunction (cardiac vs. renal) as well as the acute versus chronic nature of the condition [4]. The five subtypes of the CRS can be identified (table 1) and defined as follows:
• Acute cardiorenal syndrome (CRS type 1): an acute worsening of heart function (acute heart failure-acute coronary syndrome) leading to kidney injury and/or dysfunction.
• Chronic cardiorenal syndrome (CRS type 2): chronic abnormalities in heart function (chronic heart failure-coronary heart disease) leading to kidney injury and/or dysfunction.
• Acute renocardiac syndrome (CRS type 3): acute worsening of kidney function (acute kidney injury) leading to heart injury and/or dysfunction.
• Chronic renocardiac syndrome (CRS type 4): chronic kidney disease leading to heart injury, disease and/or dysfunction.
• Secondary cardiorenal syndromes (CRS type 5): systemic conditions causing simultaneous injury and/or dysfunction of both the heart and kidneys.
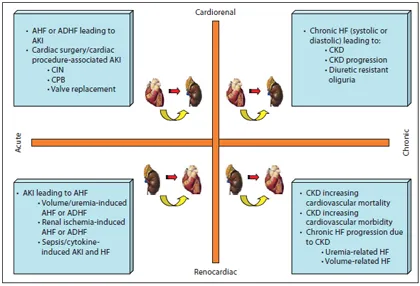
The relevant mechanisms are summarized in figure 1.
Pathophysiology of Cardiorenal Syndromes
Type 1 CRS - Acute Cardiorenal Syndrome
Premorbid renal dysfunction is common in heart failure patients [de novo acute heart failure (AHF) or acute decompensated heart failure (ADHF)] and predisposes them to acute kidney injury (AKI), which has been associated with higher risk of prolonged/re-hospitalization, cardiovascular (CV) and all-cause mortality, and faster progression to chronic kidney disease (CKD) stages 4-5 [5-9]. The incidence estimates for AKI or worsening renal function (WRF) associated with AHF and acute coronary syndrome range between 24-45 and 9-19%, respectively [4]. The broad range in reported incidence is largely attributable to variations in the definitions of WRF as well as retrospective and/or post-hoc analysis data collection [5-9].
Table 1. Modern definition of CRS
Fig. 1. CRS domain map. The timeframe and the bidirectionality of the different syndromes are described in the different subtypes (acute and chronic; cardiorenal and renocardiac). Every syndrome is then susceptible of transforming into another due to instauration of vicious circles. HF = Heart failure; CIN = contrast-induced nephropathy; CPB = cardiopulmonary bypass.
The mechanisms by which the onset of AHF or ADHF leads to AKI are multiple and complex [6]. They have been widely described in recent publications [3, 4]. The clinical importance of each of these mechanisms is likely to vary from patient to patient. The identified involved mechanisms are hemodynamic mechanisms in which a reduced cardiac output, together with an increased renal venous congestion may affect intrarenal circulation and glomerular filtration rate. Neurohormonal biofeedback mechanisms including reninangio-tensin-aldosterone system activation, a nonosmotic secretion of vasopressin and a parallel sympathetic nervous system-mediated vasoconstriction may lead to perpetuation and extension of the primary insult. We may also suggest an immune-mediated damage where the activation of monocytes and the direct effect of proinflammatory mediators may play an important role in renal tissue apoptosis and damage [10]. Finally, exogenous nephrotoxic agents such as contrast media, aminoglycosides, diuretics or angiotensin-converting enzyme inhibitors may represent another important source of kidney insult in patients with AHF or ADHF.
Humoral Signaling in CRS Type 1
The multiple factors involved in the development of AKI during heart failure describe a pathogenesis of AKI accounting for multiple pathways. Nevertheless, the occurrence of AKI even in patients with preserved or intact ejection fraction, the worsening of renal function even in the absence of fall in cardiac output, and the concept that AKI does not necessarily mean acute tubular necrosis have recently spurred new interest in humoral signaling and the inflammatory pathways to explain distant organ damage and, in particular, kidney injury in heart failure. It is known that ADHF implies an increase in circulating cytokines, but the level of this inflammatory response has not been quantified and it has not been determined in single patients.
We performed a study on 16 patients with ADHF analyzing renal function throughout hospital admission. Eight of the patients developed AKI according to the RIFLE criteria. In all patients we collected serum samples to analyze the possibility of different inflammatory patterns in patients with or without AKI development. Urea creatinine and brain natriuretic peptides (BNP) were not significantly different at admission in the two groups (A = AKI; B = non-AKI) and the amount of diuretics administered was similar. Serum samples collected at admission in all patients were incubated with human monocytic cultured cells (U-937) and the level of apoptosis was evaluated up to 96 h. Our hypothesis was that patients who develop AKI might have an inflammatory pattern due to various mediators that induce an early pathological apoptosis in normal monocytes. In this case, the humoral signal for a distant organ effect could be proved demonstrating an important contribution of the inflammatory pathway to the development of CRS type 1. In figure 2, cell apoptosis is reported in the two groups, demonstrating a significant difference at various incubation time points.
This is the first piece of evidence that CRS type 1 is an inflammatory disorder or at least the contribution of the inflammatory pathways in its pathogenesis is fundamental for the occurrence of distant organ damage.
Type 2 CRS - Chronic Cardiorenal Syndrome
Chronic heart failure patients with secondary WRF are associated with significantly increased adverse CV mortality and prolonged hospitalization. However, chronic heart disease and CKD frequently coexist in the same patient, and often the clinical scenario does not permit the ability to distinguish which disease came first. Notably, there are about 45-63.6% of chronic heart failure patients who have evidence of CKD with an estimated glomerular filtration rate <60 ml/min/1.73 m2 [11, 12]. The mechanisms causing secondary WRF in these patients likely differ from CRS type 1. Concomitant hemodynamic alterations with poor cardiac contractility and neurohormonal abnormalities with excessive production of vasoconstrictive mediators (epinephrine, angiotensin, endothelin), as well as altered sensitivity and/or release of endogenous vasodilatory factors (natriuretic peptides, nitric ...