
eBook - ePub
Monogenic Hyperinsulinemic Hypoglycemia Disorders
- 204 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Monogenic Hyperinsulinemic Hypoglycemia Disorders
About this book
In this volume of 'Frontiers in Diabetes' dealing with the molecular basis of monogenic disease of beta-cell insulin regulation, world-renowned experts provide in-depth descriptions of the many recent advances in genetic defects that cause hyperinsulinemic hypoglycemia. These disorders comprise the most important form of hypoglycemia in infants and children and are associated with a high risk of morbidity, including seizures and severe brain injury. The discovery of eight different genetic loci involved in congenital hyperinsulinism has led to greatly improved methods of diagnosis and treatment. New approaches to diagnosis are highlighted, such as 18F-DOPA PET scans for preoperative localization of focal hyperinsulinism, as well as potential new treatments, such as green tea polyphenols for GDH-HI and GLP-receptor antagonists for SUR1 and Kir6.2 hyperinsulinism. Practitioners, including pediatricians and specialists in endocrinology, surgery, genetics, pathology, and radiology, will find important up-to-date information for clinical diagnosis, management, and new treatments for infants and children with congenital hyperinsulinism. Researchers will discover how genetic hyperinsulinism disorders provide novel insights into the basic mechanisms regulating insulin secretion not only in diabetics, but also in healthy humans.
Tools to learn more effectively

Saving Books

Keyword Search

Annotating Text

Listen to it instead
Information
Stanley CA, De León DD (eds): Monogenic Hyperinsulinemic Hypoglycemia Disorders.
Front Diabetes. Basel, Karger, 2012, vol 21, pp 172-181
Front Diabetes. Basel, Karger, 2012, vol 21, pp 172-181
______________________
Exercise-Induced Hyperinsulinism: A Failure of Monocarboxylate Transporter 1 Expression Silencing
Timo Otonkoskia,b · Thomas Meissnerc
aChildren's Hospital, University of Helsinki and Helsinki University Central Hospital, and bResearch Programs Unit, Molecular Neurology, Biomedicum Stem Cell Centre, University of Helsinki, Helsinki, Finland;cDepartment of General Pediatrics, University Children's Hospital Düsseldorf, Düsseldorf, Germany
______________________
Abstract
Exercise-induced hyperinsulinism (EIHI) is a rare disorder, which has so far only been described in two families as a dominantly inherited trait and in one isolated individual. It is characterized by hypoglycemia which is triggered most prominently by anaerobic exercise. Blood glucose levels fall as blood pyruvate and lactate levels increase and, typically, hypoglycemia develops immediately following exhaustive exercise. The insulin secretion of these individuals is responsive to intravenous pyruvate unlike in healthy controls. In all patients, mutations have been found in the regulatory regions of the SLC16A1 gene, which encodes the monocarboxylate transporter 1 (MCT-1) protein. MCT-1 transports lactate and pyruvate into the cell and is expressed in practically all cell types, except the pancreatic beta-cell where it is transcriptionally silenced. The pathogenesis of EIHI is based on the failure of MCT-1 silencing, leading to inappropriate insulin secretion triggered by anaerobic exercise. Although the patients are responsive to diazoxide in terms of a general increase of blood glucose, diazoxide does not completely prevent exercise-induced hypoglycemia. Most patients do not need specific treatment because they do not have significant symptoms if they avoid strenuous exercise.
Copyright © 2012 S. Karger AG, Basel
Insulin Secretion during Exercise
In healthy humans, moderate as well as excessive exercise is not associated with severe hypoglycemia. Several factors contribute to a tight control of glucose levels. Increased hepatic glucose production, which occurs in response to moderate-intensity exercise, compensates for increased glucose demand of the muscles. An exercise-induced fall in insulin and the increase in glucagon are thought to be the primary stimuli for the increment in hepatic glucose production. During exercise, insulin secretion is in part inhibited by beta-cell alpha-adrenergic receptor activation [1-3].
During intense exercise, there is a rapid increase in the need for glucose. In this situation, glucose mobilized from muscle and liver glycogen is the exclusive muscle fuel. Intense exercise is characterized by marked increments of glucose production rising seven- to eightfold. After intense exercise, rising glycemia requires a substantial increase in insulin secretion for 40-60 min to restore pre-exercise levels [4-6], but without decreasing glucose levels into the range of hypoglycemia.
Although mild hypoglycemic symptoms during prolonged moderate exercise are common, the acute development of severe hypoglycemia during intense exercise is a rare feature. We describe otherwise healthy individuals in whom heavy exercise is associated with massive insulin secretion resulting in symptomatic hypoglycemia.
Clinical Picture and Treatment
The main clinical characteristics of the patients are listed in table 1. The index patient for this disorder was a 16-year-old German boy of Caucasian origin who presented with a 2-year history of recurrent syncope. These episodes usually occurred a few minutes after vigorous exercise. Hypoglycemia was found during one of these episodes (blood glucose <1.6 mmol/l; normal range: 3.0-5.5), which responded rapidly to intravenous glucose with relief of symptoms. During a fasting test, he developed symptomatic hypoglycemia after 12 h (blood glucose 2.2 mmol/l; insulin 20 mU/l). Ketone bodies and free fatty acids were very low during hypoglycemia, and hyperinsulinism was confirmed. First an insulinoma was suspected, but diagnostic laparotomy with manual exploration of the pancreas, intraoperative ultrasonography, and pancreatic biopsies failed to show any abnormalities. Family history was unremarkable in this patient. When the patient reported that he always suffered from hypoglycemia (home measurements of glucose and symptoms of hypoglycemia) after exercising with dumbbells at home, we tested his blood glucose and insulin levels after 5 min of intense dumbbell exercise and found a dramatic rise of insulin (49 mU/l) resulting in hypoglycemia in the recovery phase (glucose 1.9 mmol/l) [7].
The second indentified individual was a Finnish girl who presented at the age of 11 months, when she was admitted with convulsions. She had suffered from a concussion on the previous day and had been eating poorly. Blood glucose was low at 0.9 mmol/l. Subsequently, she had several hospital admissions for hypoglycemic episodes and syncope. Spontaneous blood glucose values in the range of 0.9-2.0 mmol/l were measured several times during early childhood. Extended fasting did not provoke hypoglycemia, but prolonged exercise, particularly swimming, seemed to cause hypoglycemic symptoms that were different from exhaustion and fatigue, although biochemical hypoglycemia was never documented. At the age of 15 years, a bicycle exercise test was performed with monitoring of plasma glucose and insulin. The test was stopped after 10 min and blood glucose concentration measurements 20 min later revealed hyperinsulinemic hypoglycemia (insulin 50 mU/l, glucose 1.8 mmol/l) [7]. Since these 2 cases appeared to represent a new form of hypoglycemia in which exercise was associated with inappropriate insulin secretion, we named the condition exercise-induced hyperinsulinism (EIHI).
Table 1. EIHI individuals and their main symptoms
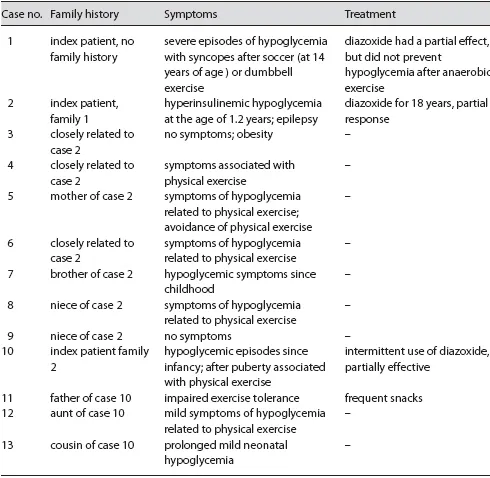
Subsequently, another Finnish patient was identified and exercise testing of family members revealed 10 additional EIHI patients for the 2 Finnish cases [8]. The age at diagnosis of these individuals varied widely between 1.5 and 60 years (median: 27). The clinical symptoms varied remarkably. Two of 9 adult patients had never recognized episodes of hypoglycemia; however, one of them was at the time of evaluation severely overweight (BMI: 36). Most of the 9 adult patients reported recurrent hypoglycemic symptoms associated with strenuous exercise. For many, swimming had often been linked with hypoglycemia-like symptoms since childhood. Aerobic mild exercise was usually well tolerated, and most subjects learned to adjust their activities so that they did not develop episodes of serious hypoglycemia. Only the 2 Finnish index cases suffered from recurrent severe episodes of hypoglycemia starting in early childhood. Prolonged neonatal hypoglycemia was reported for the patient who was 1.5-years-old at the time of diagnosis. One index patient suffered from epilepsy.
The 3 index cases had benefited from medical treatment with diazoxide, a potassium channel opener which acts by inhibiting insulin release. Diazoxide relieved their symptoms only to some extent. It was helpful to enable a longer fasting period; however, it did not totally prevent hypoglycemic episodes after exercise. Therefore, none of the patients have found it necessary to continue with the medication. Avoidance of anaerobic exercise is the most effective way to prevent severe post-exercise hypoglycemia. In addition, carbohydrates after physical exercise might be helpful, but have to be tested individually.
Clinical Physiological Studies
Different studies with changing intensity of exercise were performed. Reactions of blood glucose with and without treatment with diazoxide were investigated. After identification of the first 2 cases of EIHI, a protocol to diagnose this condition was established. Exercise testing was found necessary to clearly identify affected individuals.
Physical Exercise Testing
Most EIHI-individuals were diagnosed based on a 10-min bicycle exercise. The aim was to increase the pulse rate to an age-adjusted target of 220 minus age in years. Blood tests for glucose, insulin, pyruvate, and lactate were taken at - 10, 0, 5, 10, 15, 20, 25, 30, 35, 40, 50, and 60 min.
All individuals were normoglycemic after the overnight fast and before the test (blood glucose: 3.5-5.2 mmol/l). During exercise, and particularly immediately after it, blood glucose levels decreased in the patients, whereas a slight increase was observed in the control subjects (fig. 1). A clearly hypoglycemic level (<3.0 mmol/l) still remained in 5 of 11 patients at 60 min after the onset of exercise. The patients reported mild hypoglycemic symptoms during and after the test [8]. The increases in blood pyruvate (fourfold from basal level) and lactate (tenfold) were similar in patients and control subjects up to the 15-min sample. Serum insulin levels increased during and immediately after exercise in the patients and were significantly higher at 20 min after exercise in patients compared to control subjects (39 vs. 11 mU/l, p <0.05; fig. 1).
Anaerobic exercise testing to exhaustion seems to be even more diagnostic for EIHI. Exercise with an intensity corresponding to 130% VO2 max, which means that exercise leads to exhaustion, within 2-3 min elicited comparable maximal lactate levels in an EIHI patient and controls (10-11 mmol/l). The German index patient for EIHI was further tested at an institute of sports medicine. He, but not the controls, experienced a massive increase in insulin from 34 to 649 mU/l after the intense anaerobic test (fig. 2) [9]. The increase in insulin was much more pronounced with this protocol compared to milder exercise tests done earlier (insulin increase to 50-90 mU/l) in the same individual.
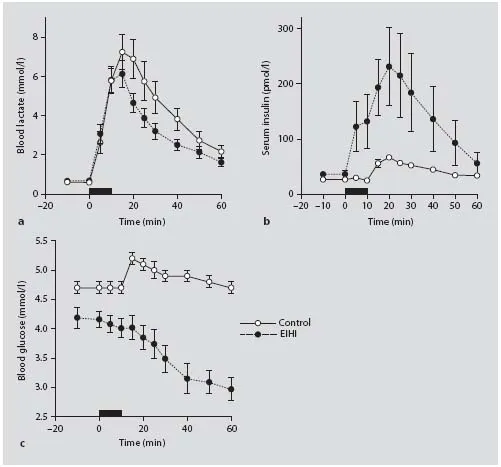
Fig. 1. Physical exercise test. Blood lactate (a), serum insulin (b), and blood glucose (c) concentrations before, during, and after a 10-min bicycle exercise (black bar) in healthy controls (white circles, n = 7) and EIHI patients (black circles, n = 11). Modified from Otonkoski et al. [8].
Suggested Exercise Protocol
Since the data for affected individuals are still sparse, we recommend the following extended protocol for exercise testing in adults after exclusion of cardiac risk factors. The increase in lactate is a particularly important aspect for the diagnosis. The protocol has to be individually adapted for children.
The bicycle exercise test should start after an 8- to 12-hour overnight fast without any significant exercise in the preceding 24 h. If this is not possible, a 4-hour fast will also be suitable. An intravenous cannula is inserted into a large (e.g. antecubital) vein for blood sampling. Blood is sampled at two 10-min intervals before the beginning of exercise to ensure a steady state. Blood samples are drawn on a total of about 10 occasions (including at -20, -10, and 0 min before the test; 2-min intervals during the exercise period and early recovery; and 5, 15, 30, 45, and 60 min during later recovery). Glucose, insulin, and lactate are measured. After a 5-min warm-up phase with low intensity, the workload is increased every minute until the patient is exhausted within 5-7 min (to make the total exercise test 8-12 min). Exhaustion is defined by the subject at the time at which he or she is unable to continue cycling due to leg muscle fatigue. The increase of the workload has to be fast to ensure that the total duration of the test is not more than 8-12 min, including the warm-up phase. Typical for EIHI is a marked increase of insulin in parallel with the change in lactate. This results in a drop of glucose during the recovery phase 20-45 min after exercise. It is essential that during and after testing there is awareness for symptoms of hypoglycemia and necessary preparations (availability of i.v. glucose) have been taken to treat severe h...
Table of contents
- Cover Page
- Front Matter
- Historical Perspective on the Genetic Forms of Congenital Hyperinsulinism
- Biochemistry and Physiology of the ATP-Sensitive Potassium Channel
- Pathophysiology of Diffuse ATP-Sensitive Potassium Channel Hyperinsulinism
- Molecular Defects of ATP-Sensitive Potassium Channels in Congenital Hyperinsulinism
- Molecular Mechanisms and Clinical Pathophysiologies of Focal ATP-Sensitive Potassium Channel Hyperinsulinism and Beckwith-Wiedemann Syndrome
- Pancreatic Histopathology of Hyperinsulinism
- Localization of a Focal Lesion of Congenital Hyperinsulinism: Imaging and Surgery
- Role of Incretin Hormones in Hyperinsulinemic Hypoglycemia
- Glutamate Dehydrogenase: Structure, Regulation, and Its Role in Insulin Homeostasis
- Congenital Hyperinsulinism Due to Activating Mutations of Glutamate Dehydrogenase: The Hyperinsulinism/Hyperammonemia Syndrome
- Amino Acid-Stimulated Insulin Secretion: The Role of the Glutamine-Glutamate-Alpha-Ketoglutarate Axis
- Tissue Specificity of Glutamate Dehydrogenase as Illustrated in Pancreatic Beta-Cells and the Central Nervous System
- The Molecular Genetics and Pathophysiology of Congenital Hyperinsulinism Caused by Short-Chain 3-Hydroxyacyl-CoA Dehydrogenase Deficiency
- Hyperinsulinism Due to Activating Mutations of Glucokinase
- Hyperinsulinism Due to Mutations of Uncoupling Protein 2
- Exercise-Induced Hyperinsulinism: A Failure of Monocarboxylate Transporter 1 Expression Silencing
- HNF4A and Hyperinsulinemic Hypoglycemia
- Author Index
- Subject Index
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn how to download books offline
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 990+ topics, we’ve got you covered! Learn about our mission
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more about Read Aloud
Yes! You can use the Perlego app on both iOS and Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app
Yes, you can access Monogenic Hyperinsulinemic Hypoglycemia Disorders by C. A. Stanley,D. D. De León,C.A., Stanley,D.D., De León, Massimo Porta,Massimo, Porta in PDF and/or ePUB format, as well as other popular books in Medicine & Endocrinology & Metabolism. We have over one million books available in our catalogue for you to explore.