eBook - ePub
Polycystic Ovary Syndrome
Novel Insights into Causes and Therapy
- 188 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Polycystic Ovary Syndrome
Novel Insights into Causes and Therapy
About this book
Polycystic ovary syndrome (PCOS) is the most frequent disorder affecting women of reproductive age. Recent years have shown substantial advances in our understanding of the complex genetic, biochemical, metabolic, cardiovascular, and reproductive issues associated with PCOS. This book presents a comprehensive overview of recent clinical developments in identifying the phenotypic expression of women with PCOS resulting in a completely new recognition of its phenotypic variability. Metabolic and cardiovascular consequences of the syndrome are discussed in detail. Advances made in dealing with secondary forms of PCOS-like syndromes are presented as well as specific therapies of clinical manifestations and their outcomes. Additionally, a number of hot topics are included presenting genetic developments, endothelial causes leading to unfavorable outcomes, and novelties in therapeutic approaches dealing with metabolic and reproductive consequences. Covering phenotypic characteristics, diagnostic criteria, central pathophysiological mechanisms, metabolic, cardiovascular and reproductive aspects, and modern therapeutic approaches, this book is a useful tool for general practitioners, gynecologists, pediatricians, internists, endocrinologists, as well as cardiologists.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Polycystic Ovary Syndrome by D. Macut,M. Pfeifer,B. O. Yildiz,E. Diamanti-Kandarakis,D., Macut,M., Pfeifer,B.O., Yildiz,E., Diamanti-Kandarakis, Federica Guaraldi,Giovanni Corona,Federica, Guaraldi,Giovanni, Corona in PDF and/or ePUB format, as well as other popular books in Medicine & Cardiology. We have over one million books available in our catalogue for you to explore.
Information
Macut D, Pfeifer M, Yildiz BO, Diamanti-Kandarakis E (eds): Polycystic Ovary Syndrome. Novel Insights into Causes and Therapy. Front Horm Res. Basel, Karger, 2013, vol 40, pp 142–157 (DOI: 10.1159/000341846)
______________________
Endocrinopathies and Other Disorders Inducing a Polycystic Ovary Syndrome Phenotype
Krystallenia I. Alexandraki · Gregory A. Kaltsas
Department of Pathophysiology, National University of Athens, Athens, Greece
______________________
Abstract
Amongst the commonest endocrine symptoms encountered in premenopausal women are those related to excessive androgen secretion or action, along with menstrual irregularity. The vast majority of women presenting with such symptoms will be found to have the polycystic ovary syndrome (PCOS), a disorder characterized by specific clinical, endocrine and ultrasonographic features. PCOS is regarded as a state of ‘functional hyperandrogenism’, as no distinct source of autonomous androgen secretion is identified and is commonly associated with insulin resistance. This later feature may also be related to some long-term sequelae of the syndrome that are associated with metabolic abnormalities and excessive cardiovascular morbidity. Although PCOS in the short-term is regarded as a ‘benign’ disease, a proportion of patients may harbor other underlying disorders that can be life-threatening, requiring prompt diagnosis and treatment. Adrenal and ovarian androgen-secreting tumors, adrenal and ovarian steroidogenic deficiencies along with other medical or endocrine conditions, particularly in the presence of insulin resistance, can exhibit similar clinical, endocrine and/or ultrasonographic features to PCOS.Their early identification is based on the presence of distinct features and a high index of suspicion.
Copyright © 2013 S. Karger AG, Basel
Symptoms and signs of hyperandrogenism, namely hirsutism and acne, and menstrual irregularity in the form of chronic anovulation are amongst the most common endocrine abnormalities found in premenopausal women [1, 2]. The vast majority of such women will be found to have the polycystic ovary syndrome (PCOS), a chronic disorder usually manifested from adolescence, characterized by distinct endocrine abnormalities and the presence of polycystic ovaries (PCO) on ovarian ultrasonography [1, 2]. Although PCO can be found in 21-23% of premenopausal women, approximately 7% will develop the full clinical and endocrinological manifestations of PCOS [3]. This implies that additional factors may also operate for the development of the syndrome, the most probable being hyperinsulinemia and insulin resistance (IR) [4]. Recently an International Consensus Group proposed that PCOS can be diagnosed when at least two of the following criteria are present: oligo-ovulation or anovulation (usually manifested as oligomenorrhea or amenorrhea), elevated circulating androgen levels (hyperandrogenism), and PCO as defined by ultrasonography [5]. It was also suggested by the same group that the diagnosis of PCOS can be made with certainty when other medical conditions exhibiting similar clinical endocrine and ultrasonographic manifestations have been excluded [2, 4, 5].
Current understanding of the pathogenesis of PCOS suggests that it is a complex, multigenic disorder [4]. Genes that regulate the hypothalamo-pituitary-ovarian axis and those responsible for the development of IR appear to be related to the development of PCOS. Although alterations of gonadotropin secretion, particularly luteinizing hormone (LH), are implicated in the development of PCOS, disorders associated with hypersecretion of these hormones are extremely rare. In contrast, alterations of insulin secretion and/or action are found in many common disorders that are related to PCOS (table 1). Insulin, either alone or in association with LH, enhances androgen production from the ovaries while inhibiting hepatic synthesis of sex hormone-binding globulin (SHBG) from the liver; the net result of this effect is an increase in the biologically active androgens [2, 4]. This notion is further reinforced by the findings that hyperinsulinemia and IR are more prominent in women with PCOS and menstrual irregularity irrespective of the presence of obesity [4]. Excessive insulin levels correlate with the clinical severity of the syndrome and exert a stimulatory effect on the ovaries that remain sensitive to its action [6]. In addition, when obesity is present, IR is exacerbated further contributing to the worsening of the clinical phenotype [6]. It is therefore possible that hyperinsulinemia and IR may be implicated as an underlying pathogenic mechanism in several disorders associated with a PCOS-like phenotype [2] (table 1). In addition, a number of disorders associated with excessive androgen production from the adrenals and/ or ovaries, or that affect steroid biosynthesis, secretion, metabolism and/or action, may exhibit similar to the PCOS clinical, endocrine and/or ultrasonographic features [2] (table 1).
Although PCOS remains the underlying diagnosis when such alternate diseases are excluded, the extent to which patients presenting with a PCOS phenotype should be investigated for other diseases has not yet been defined [2, 7]. It is estimated that the prevalence of disorders other than PCOS in women presenting with such symptoms is less than 7%; however, a number of them can cause considerable morbidity and/or even can be life-threatening [2, 8]. It is therefore important to be aware of the distinct features that these diseases may harbor to be able to identify them promptly.
Table 1. Disorders associated with the PCOS phenotype
| Adrenal hyperandrogenism Congenital adrenal hyperplasia Adrenal androgen-producing tumors (adenomas, carcinomas) Abnormal cortisol action and/or metabolism |
| Ovarian hyperandrogenism Ovarian steroidogenic defects Ovarian androgen-producing tumors Hyperthecosis, luteoma Ectopic LH secretion |
| Other endocrinopathies Cushing's syndrome Acromegaly Hyperprolactinemia Insulinoma Ectopic LH secretion Precocious puberty Thyroid disorders |
| Syndromes of hyperinsulinemia and IR states Lipoatrophic diabetes Leprechaunism Rabson-Mendenhall Kahn types A and B IR Diabetes mellitus type 2 Gestational diabetes mellitus Obesity Lipodystrophy |
| Other non-endocrine disorders Epilepsy (?) Intracranial hypertension |
| Drugs Valproic acid Growth hormone Oxcarbazepine |
Disorders Associated with a PCOS Phenotype
Disorders Associated with Abnormalities of Steroid Secretion, Metabolism and/or Action
Adrenal and Ovarian Androgen-Producing Tumors
Androgen-producing tumors, mostly adrenal carcinomas, and a wide variety of ovarian tumors can present with symptoms/signs of virilization (clitoromegaly, deepening of the voice, frontal balding, and muscle hypertrophy), hyperandrogenism and chronic anovulation [7, 8] (fig. 1). Virilization seems to represent a distinctive feature for the presence of such tumors as it is extremely rare in women with PCOS, and when present it is usually mild. Adrenal carcinomas are large tumors that can hypersecrete testosterone or its precursors with or without concomitant cortisol hypersecretion. Ovarian neoplasms can be of variable size secreting mainly testosterone, although rarely can also co-secrete various androgen precursors [9]. Occasionally, ovarian neoplasms of epithelial origin may produce factors stimulating steroidogenesis in a paracrine fashion. Sertoli-Leydig cell tumor is the commonest virilizing ovarian tumor that occurs during the second to fourth decade of life and may be gonadotropin responsive [9]. A number of other tumors that also simulate the PCOS, such as hilus cell tumors, benign cystic teratomas and adrenal rest tumors have also been described; these tumors occur more frequently in postmenopausal women [8]. Ovarian hyperthecosis (nests of luteinizing cells distributed throughout the ovarian stroma) can present with a similar picture and be associated with severe IR [8]. The ovaries are enlarged and of an extremely firm texture as a result of extensive and dense fibroblast growth; the absence of follicle formation provides a clear morphologic distinction from the PCOS ovary [8]. The majority of virilizing tumors present during the middle age with symptoms such as rapidly progressive androgenic alopecia, deepening of the voice, increased libido and a male body habitus. However, particular attention should be paid to the rare cases of slowly evolving tumors, which can be clinically indistinguishable from PCOS [2, 7]. Although the majority of patients with tumors invariably have elevated androgen levels, only testosterone values >7 nmol/l (200 ng/dl) are highly suggestive of an androgen-secreting tumor [2, 7]. Occasionally, the documentation of an ovarian androgen-secreting tumor may be difficult as these tumors can be relatively small, eluding the detection with conventional imaging modalities [9]. Although in such cases bilateral adrenal and ovarian catheterization and sampling to document a gradient of an androgenic steroid has been employed, the detection rate remains relatively low [9]. Prompt diagnosis and management of these tumors are important, particularly in cases of adrenal carcinoma (fig. 2), as patients with localized disease exhibit a much more favorable prognosis compared to patients with more extensive disease [2].

Fig. 1. Excessive hirsutism in a young woman who was found to have Cushing's syndrome secondary to ectopic adrenocorticotrophin secretion.
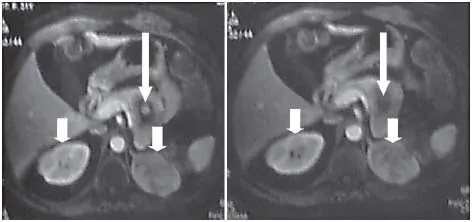
Fig. 2. T1-weighted MRI of the abdomen demonstrating bilateral adrenocortical carcinomas (short white arrows) and a pancreatic neuroendocrine tumor (long white arrow) in a 34-year-old woman with multiple endocrine neoplasia syndrome type who was initially diagnosed to suffer from PCOS.
Adrenal-Ovarian Steroi...
Table of contents
- Cover Page
- Front Matter
- Polycystic Ovary Syndrome: Definitions, Phenotypes and Diagnostic Approach
- Pathophysiology of Polycystic Ovary Syndrome: The Role of Hyperandrogenism
- Genetics of Polycystic Ovary Syndrome
- Obesity, Adipokines and Metabolic Syndrome in Polycystic Ovary Syndrome
- Dyslipidemia and Oxidative Stress in PCOS
- Cardiovascular Risk and Subclinical Cardiovascular Disease in Polycystic Ovary Syndrome
- Insulin Sensitizers in Polycystic Ovary Syndrome
- Hirsutism – From Diagnosis to Use of Antiandrogens
- Combined Oral Contraceptives in Polycystic Ovary Syndrome – Indications and Cautions
- Infertility Treatment in Polycystic Ovary Syndrome: Lifestyle Interventions, Medications and Surgery
- Endocrinopathies and Other Disorders Inducing a Polycystic Ovary Syndrome Phenotype
- Non-Classic Adrenal Hyperplasia due to the Deficiency of 21-Hydroxylase and Its Relation to Polycystic Ovarian Syndrome
- Author Index
- Subject Index