![]()
Clinical Aspects of High-Risk HPV Infections
Pfister H (ed): Prophylaxis and Early Detection of HPV-Related Neoplasia.
Monogr Virol. Basel, Karger, 2012, vol 28, pp 58-71
______________________
Penile Cancer and Penile Intraepithelial Neoplasia
G. Gross
Department of Dermatology and Venereology, University of Rostock, Rostock, Germany
______________________
Abstract
There is evidence that high-risk human papillomaviruses (HPVs), particularly HPV16, have a pathogenic role in about 45-50% of penile carcinoma. Very similar to the pathogenesis of vulvar cancer, there may be two etiologies for penile cancer, one HPV-related and the other due to non-HPV-related factors, such as lichen sclerosus and other chronic inflammatory diseases. Most likely, the pathogenesis reflects several steps of events over some decades from precursor lesions to squamous cell cancer. Increased attention has to be paid to the recognition of early stages of penile cancer and premalignant lesions, especially the flat and very flat lesions. Preventive measures include topical treatment of warts, destruction or surgical excision of intraepithelial lesions. Prevention is also in line with a careful treatment of inflammatory conditions such as lichen sclerosus and surgical correction of phimosis. Furthermore, neonatal circumcision, prevention of phimosis, smoking cessation and avoiding UV and dermatologic psoralen and UVA exposition of external genitals should be promoted. The prevalence of HPV16 and HPV18 in penile cancer and precursor lesions suggests that available HPV vaccines are possibly effective to substantially reduce the burden of the disease. This, however, depends on the dissemination of the HPV vaccines to a large part of the young males in the different populations.
Copyright © 2012 S. Karger AG, Basel
The prevalence of genital human papillomavirus (HPV) infection in men is variable depending on the population studied with a peak incidence between 16 and 35 years of age [1, 2]. The prevalence of genital HPV DNA in men is between 1.3 and 72.9% with most studies reporting more than 20% [3]. A large proportion of HPV infections spontaneously regress. In a number of patients, HPV infection persists with a risk of developing intraepithelial neoplasia and invasive cancer.
In analogy to the pathology of the female lower genital tract, HPV-associated lesions in the male genital area have been divided into low-risk (LR) and high-risk (HR) HPV types based on the association of each genotype with benign genital warts (see chapter by Gross, p.19), penile cancer and precursor lesions [penile intraepithelial neoplasia (PIN)]. HR HPV types (HPV16, 18, 31, 33, 35, 39, 45, 52, 54, 56, 58, 59, 65, 67, 68), which tend to persist, have been identified in PIN of different grades, in situ carcinomas and invasive carcinomas of the penis [4].
Infections with HR HPV genotypes may be latent, subclinical or result in very flat lesions [5]. Histologically the latter lesions exhibit features of low, moderate or severe dysplasia (PIN grade 1, 2 or 3). In 19-44% of genital warts, coinfections with HR HPV types may be present [6].
Penile Intraepithelial Neoplasia
PIN is a heterogeneous condition. Standard clinical protocols for diagnosis do not exist.
The very first manifestation of HR HPV-associated PIN is an inconspicuous flat lesion, which is best diagnosed using the acetic acid test and histology. Atypical cells are initially visible in basal layers of the infected epithelia. These lesions are in line with squamous hyperplasia and features of low-grade PIN (PIN1). Flat penile lesions are strongly associated with cervical intraepithelial neoplasia in female sexual partners [7, 8]. Fifty to seventy percent of affected men have cervical intraepithelial neoplasia-positive female partners compared with 10-20% of men whose sexual partners are cervical intraepithelial neoplasia negative. Most of these flat lesions regress during 1-2 years. A certain percentage, however, may persist [9]. Higher-grade PIN lesions are thought to be precursors of penile squamous cell carcinoma. However, only a small proportion (5-15%) of PIN converts into invasive penile cancer.
PIN3 lesions are completely devoid of fully differentiated keratinocytes. Only very small numbers of koilocytes are seen and thus low amounts of virus, if ever, are produced within the epithelia of PIN3. Thus infectivity of PIN3 is thought to be extremely low or absent. This is in contrast to low-grade and moderate PIN (PIN1 and PIN2, respectively) and to LR HPV-associated genital warts (see chapter by Gross, p. 19).
Malek et al. [10] as well as Aynaud et al. [11] showed that the mean age of patients affected by PIN1 or PIN2 is 35.8 years. The age of patients with PIN3 and invasive squamous cell carcinoma of the penis is 56.1 and 65.3 years, respectively. Apparently, it takes at least 20 years for penile infection with HR HPV to develop into squamous cell carcinoma. In contrast to PIN grade 2 and PIN grade 3, where preferentially HPV16 and other HR HPV types are discovered, in PIN1 lesions, both LR HPV types and to a lesser degree HR HPV types have been detected. Different studies revealed that high-grade PIN lesions present differently in men of younger age (25-40 years) and in men older than 40 years [7, 12-14]. Differentiation of PIN3 from patients of the two different age groups can only be done on clinical grounds, since histology is likely to be identical [15].
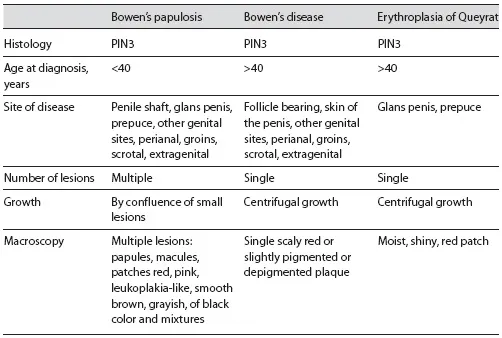
Clinically there are three different conditions that have the histological features of PIN3: erythroplasia of Queyrat occurring on the glans, Bowen's disease involving the follicle-bearing skin of the penile shaft and bowenoid papulosis. The latter has been detected almost always in younger men [11] (table 1). Bowen's disease and erythroplasia of Queyrat were described 100 years ago [16, 17], whereas bowenoid papulosis [syn.: multicentric (pigmented) Bowen's disease] was first described in 1970 [18].
Table 1. Characteristic features of PIN
Human Papillomavirus and Penile Intraepithelial Neoplasia
In the early 1980s, HPV16 DNA was repeatedly identified in biopsies from penile Bowen's disease and bowenoid papulosis (multiple papular penile lesions with histologic features of high-grade dysplasia) [19, 20]. HPVs have been identified in all types of PIN. According to Aynaud et al. [11], Barrasso et al. [12] and Horenblas et al. [2], the rate of HPV infection in PIN varies from 60 to 100%. A history of anogenital warts was notified as a significant risk factor for PIN and penile cancer [21]. In a more recent study, Wikström et al. [22] detected HPV DNA in 93% of PIN lesions. Interestingly, 21% of analyzed PIN3 lesions were positive only for LR HPV types compared to 68% of LR HPV positivity in PIN1 lesions. In contrast, HR HPV types were found in only 10% of PIN1 lesions, while 64% of PIN3 lesions were positive for HR HPV DNA. The simultaneous detection of the cutaneous HPV8 and the mucosotropic HPV16, 39 or 51 in cases of erythroplasia of Queyrat by Wieland et al. [23] was surprising and remains still not understood. HPV8 DNA was identified in 8/8 lesions. Coinfections with HPV16 were observed in 88% of the lesions.
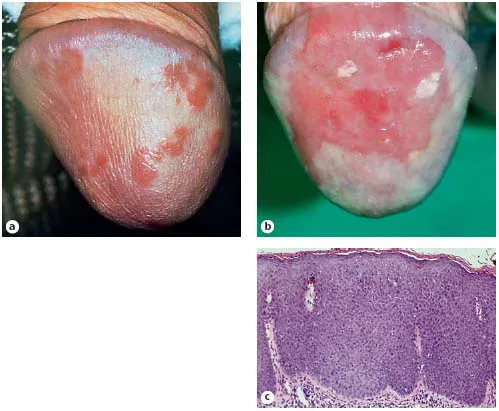
Fig. 1. Penile intraepithelial neoplasias.a Multiple maculopapular erythematous lesions of the glans penis (bowenoid papulosis). b Flat partially slightly elevated solitary plaque of the glans penis (erythroplasia of Queyrat). c Histology: PIN3.
Studies evaluating the relationship between HPV-related genital lesions in sexual partners are further hints to link HPV and PIN [8, 12, 24-28].
Penile Intraepithelial Neoplasia in Young Men
HR HPV-associated PIN grade 1-3 lesions in young men may manifest macroscopically as multiple, flat, brownish or red macules or slightly elevated papules, leukoplakialike lesions or red, papular lesions as well as mixtures of different types of papules [14]. PIN lesions in young men tend to be multiple, grow multifocally at the entire genitoanal skin and have a tendency to confluence (fig. 1). By definition, papular PIN3 lesions in young men have been known as bowenoid papulosis [18, 29]. Such lesions may spontaneously regress as do flat PIN3 lesions and PIN3 lesions of mixed features. However, recurrence of bowenoid papulosis lesions and malignant conversion may also occur [30], particularly in severely i...