Radiosurgery
8th International Stereotactic Radiosurgery Society Meeting, San Francisco, June 2007
- 436 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
Radiosurgery
8th International Stereotactic Radiosurgery Society Meeting, San Francisco, June 2007
About this book
The aim of the International Stereotactic Radiosurgery Society (ISRS) is to promote technical developments in stereotactic radiosurgery on the highest level of clinical experience based on clinical investigations. In this volume, high-quality peer-reviewed papers from the 8th International Stereotactic Radiosurgery Society meeting held in San Francisco 2007 are presented. The reports include new studies on physics, imaging and radiobiology in radiosurgery as well as the latest research in the field of cranial radiosurgery on benign tumors, malignant tumors and vascular malformations. Further articles cover new investigations in the practice on spinal and body radiosurgery.This publication is of special interest to neurosurgeons, radiation oncologists and medical physicists who require precise information to keep up to date with the important developments on the use of stereotactic radiosurgery.
Frequently asked questions
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Information
Raising Questions and Answering Them: A Personal Approach to Radiosurgery. The 2007 Jacob I. Fabrikant Award Lecture
If we are to be biologic surgeons..
What are the effects of a single radiation dose to the brain?
What are the effects of different doses, over time, and in different brain locations?
What about tumor or AVM doses, in models closer to humans, over longer periods of time?
Clinical indication | Procedures n |
Arteriovenous malformation | 1,132 |
Cavernous malformation | 126 |
Arteriovenous fistula | 31 |
Vestibular schwannoma | 1,252 |
Trigeminal schwannoma | 36 |
Other schwannoma | 43 |
Meningioma | 1,126 |
Pituitary tumor | 255 |
Craniopharyngioma | 63 |
Hemangioblastoma | 41 |
Hemangiopericytoma | 32 |
Glomus tumor | 19 |
Pineocytoma | 16 |
Malignant pineal tumor | 13 |
Chordoma | 27 |
Chondrosarcoma | 19 |
Choroid plexus papilloma | 10 |
Hemangioma | 8 |
Glioblastoma multiforme | 305 |
Anaplastic astrocytoma | 122 |
Astrocytoma | 39 |
Oligodendroglioma | 19 |
Pilocytic astrocytoma | 71 |
Ependymoma | 62 |
Medulloblastoma | 21 |
CNS lymphoma | 11 |
Hypothalamic hamartoma | 4 |
Brain metastasis | 2,382 |
Malignant skull base tumor | 44 |
Other tumor | 20 |
Trigeminal neuralgia | 721 |
Sphenopalatine neuralgia | 7 |
Cluster headache | 5 |
Thalamotomy for tremor | 78 |
Mesial temporal lobe epilepsy | 3 |
Obsessive compulsive disorder | 3 |
Cancer pain | 2 |

Skull Base Tumors
How do we maintain cranial nerve function inpatients with acoustic neuromas?
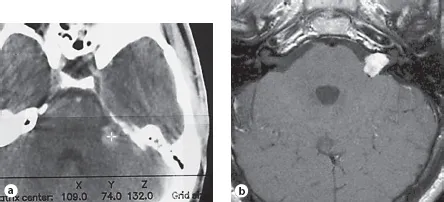
Table of contents
- Cover Page
- Front Matter
- Raising Questions and Answering Them: A Personal Approach to Radiosurgery. The 2007 Jacob I. Fabrikant Award Lecture
- Stereotactic Orthogonal Films Can Be Used as an Indication of Linear Accelerator Ageing
- Routine Dosimetric Verification of Stereotactic Treatments Using Monte Carlo Methods in a Distributed Computing Environment
- Three-Dimensional Gel Dosimetry for Dose Volume Histogram Verification in Stereotactic Radiosurgery
- Dose Distribution Comparison for the Treatment of Spinal Metastases Using CyberKnife® versus IMRT Stereotactic Body Radiotherapy Using Linac/CT-on-Rails Unit
- Miniature Ion Chamber for Output Calibration of Stereotactic Radiosurgery Units
- Functional Relationship between the Volume of a Near-Target Peripheral Isodose Line and Its Isodose Value for Gamma Knife® Radiosurgery
- Monte Carlo Simulation Dose Calculation for Intensity Modulated Radiosurgery
- Relationship between Radiosurgery Conformity Indices and Acoustic Neuroma Tumor Volume
- Failure of Arteriovenous Malformation Radiosurgery and Its Prevention Using True Image Fusion of Rotation CINE Angiograms in Integrated Multiplanar Imaging
- Observation of Shift Phenomena when Using 3T MRI Scanners in Stereotactic Radiosurgery
- Diffusion-Tensor Imaging Tractography of the Corticospinal Tract for Evaluation of Motor Fiber Tract Radiation Exposure in Gamma Knife® Radiosurgery Treatment Planning
- Acoustic Neuroma Radiosurgery: Lessons Learned
- Radiosurgery of Intracranial Schwannomas: Comparative Study of Follow-Up Evaluation
- Treatment of a Large Acoustic Tumor with Fractionated Stereotactic Radiotherapy
- Current Treatment Strategy of Gamma Knife® Surgery for Vestibular Schwannoma: Image-Guided and Robotized Microradiosurgery
- Non-Surgical Management of Meningiomas Involving the Cavernous Sinus
- Long-Term Follow-Up of 32 Meningiomas of the Clivus and Foramen Magnum Subjected to Stereotactic Radiosurgery
- Safety and Efficacy of Fractionated Stereotactic Radiotherapy in the Treatment of Skull Base Tumors: An Evidence-Based Approach
- Image-Guided Micro Gamma Knife® Surgery for Skull-Base Tumors to Avoid Underlying Dysfunction of the Surrounding Vital Structures Using CISS with Gadolinium Enhancement
- Endocrine Issues Related to Stereotactic Radiosurgery in the Vicinity of the Pituitary Gland
- Simultaneously Integrated Boost to Multiple Brain Metastases during Whole Brain Radiation Therapy-Hippocampal Avoidance
- Gamma Knife® Radiosurgery Alone for One to Four Brain Metastases. Is Prophylactic Whole-Brain Radiation Therapy Really Necessary?
- Linac Stereotactic Radiosurgery of the Resection Cavity following Surgical Removal of Brain Metastasis: A Brief Report
- Radiosurgery as Salvage Therapy for Primary Central Nervous System Lymphoma
- Survival following Stereotactic Radiosurgery for Newly Diagnosed and Recurrent Glioblastoma Multiforme: A Multicenter Experience
- Arteriovenous Malformation Radiosurgery: Realities from a Twenty-Year Perspective
- Dynamic Definition of Critical Zones for Radiosurgery in AVMs
- Gamma Knife® Radiosurgical Strategy for Pediatric High-Grade Arteriovenous Malformations: Advantages of Staged Radiosurgery Prior to Targeting Nidus Proximal to the Drainer
- Hyperbaric Oxygen in the Management of Brain Edema Associated with Stereotactic Radiosurgery
- Gamma Knife® Radiosurgery of the Trigeminal Nerve and Sphenopalatine Ganglion for Cluster Headache
- Impact of Dose Rate on Outcomes of Gamma Knife® Radiosurgery in Patients with Face Pain
- Comparisons of Novalis and CyberKnife® Spinal Stereotactic Body Radiotherapy Treatment Planning Based on Physical and Biological Modeling Parameters
- Preliminary Results of Stereotactic Radiotherapy for Spinal Lesions using the Novalis System
- Imaging Resolver Localization for Whole-Body Stereotaxy Using TomoTherapy
- Utilization of Image-Guided Radiation Therapy Equipment to Enhance Stereotactic Body Radiation Therapy Commissioning
- Use of Platinum Embolization Coils for Targeting Liver Lesions in Stereotactic Body Radiotherapy/Radiosurgery
- Author Index
- Subject Index