eBook - ePub
Transplantation Dermatology
- 210 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Transplantation Dermatology
About this book
Patients undergoing solid organ and hematopoietic stem cell transplantation frequently develop skin diseases that can be challenging to themselves and their doctors. In the first part of this volume, prevalent epidemiological, clinical and histological skin problems of solid organ recipients are discussed. Pre- and posttransplant management as well as follow-up programs are presented focusing on European and Swiss guidelines. A special chapter is dedicated to immunosuppressive drugs considering current standards, and new and upcoming medication. The second part starts with a summary of historical aspects of hematopoietic stem cell transplantation, and proceeds with a description of skin manifestations of graft-versus-host disease and their therapy. Covered are early, late and very late periods after transplantation with a focus on recent consensus classification and treatment aspects of chronic graft-versus-host disease. The publication ends with a comprehensive review and practical guidance on photoprotection in transplant recipients. This book covers all the important dermatological aspects that should be considered in diagnosis and treatment of recipients of solid organ and hematopoietic stem cell transplants. It is intended as a guide for dermatologists, nephrologists, hemato-oncologists and all specialists involved in the field of transplantation.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
At the moment all of our mobile-responsive ePub books are available to download via the app. Most of our PDFs are also available to download and we're working on making the final remaining ones downloadable now. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Transplantation Dermatology by P. Häusermann,J. Steiger,J. Passweg,P., Häusermann,J., Steiger,J., Passweg, P. Itin,G. B. E. Jemec,P., Itin,G.B.E., Jemec in PDF and/or ePUB format, as well as other popular books in Medicine & Cardiology. We have over one million books available in our catalogue for you to explore.
Information
Photoprotection
Häusermann P, Steiger J, Passweg J (eds): Transplantation Dermatology.
Curr Probl Dermatol. Basel, Karger, 2012, vol 43, pp 171-196
Curr Probl Dermatol. Basel, Karger, 2012, vol 43, pp 171-196
______________________
Photoprotection in Transplant Recipients
Christian Surbera · Mark Pittelkowc · Stephan Lautenschlagerb
aDepartment of Dermatology, University Hospital of Basel, Basel,bOutpatient Clinic of Dermatology, Triemli Hospital, Zurich, Switzerland;cDepartments of Dermatology and Biochemistry and Molecular Biology, Mayo Clinic, Rochester, Minn., USA
______________________
Abstract
Skin cancers remain the most commonly diagnosed neoplasms among organ transplant recipients (OTRs), comprising nearly 40% of all posttransplant malignancies. The occurrence of skin tumors has a considerable impact on the quality of life and the overall survival of OTRs. Ultraviolet radiation (UVR) is the major environmental cause of nonmelanoma skin cancers, and it is therefore pivotal to protect the skin from UVR in order to prevent de novo and progression of preinvasive and invasive malignancies. The present chapter delivers background information on UVR, photoprotection and accompanying concerns regarding vitamin D, as well as educational and behavioral aspects of photoprotection in OTRs; some common misconceptions and mistakes regarding photoprotection are addressed as well.
Copyright © 2012 S. Karger AG, Basel
Skin cancers remain the most commonly diagnosed neoplasms among organ transplant recipients (OTRs), comprising nearly 40% of all posttransplant malignancies [1]. The occurrence of skin tumors has a considerable impact on the quality of life and the overall survival of OTRs [2]. In addition to the increased incidence of these tumors in the OTR population, the tumors tend to behave more aggressively than those in nontransplants. Most of the cutaneous malignancies diagnosed in OTRs are nonmelanoma skin cancers (NMSC), with squamous cell carcinomas (SCC) and basal cell carcinomas (BCC) accounting for more than 90% of the total (table 1) [3].
The reported average time to develop NMSC is estimated to range from 3 to 10 years after organ transplantation [2, 8-12]. Male gender, older age at transplantation, and longer follow-up after transplantation are independently associated with the onset of NMSC [10]. Other predictors of NMSC after organ transplantation are skin phototypes I—III according to the Fitzpatrick scale, an excessive sun exposure history, ‘aggressive’ immunosuppressive medication and genetic factors [8, 13, 14].
Cumulative ultraviolet radiation (UVR) is the primary responsible carcinogen for the induction and promotion of NMSC, as suggested by the fact that the lesions almost exclusively appear on UV-exposed skin [15]. Hence, patients working in typical outdoor occupations or spending most of their leisure time outdoors and patients living in countries with high UV indices are at higher risk. The determinants of skin cancer development in OTRs are well defined (table 2).
Table 1. Population-based standardized incidence ratios of skin cancers in OTRs [4-7].
| Skin cancer | Increase in incidence (x) |
| SCC | >65-220 |
| BCC | >10-16 |
| Melanoma | >2.2-8 |
| Kaposi sarcoma | >84 |
Table 2. Risk factors for the development of skin cancer after organ transplantation
| Skin cancer | |
| Exposure to UVR | |
| Fitzpatrickskin types I-III | |
| Increased age at transplantation | |
| Duration, degree, and type of immunosuppression | |
| Type of organ transplant | |
| Previous organ transplant | |
| Personal history of actinic keratosis | |
| HPV infection | |
UVR is presumably the only factor that is to a certain degree ‘avoidable’. Sun avoidance and sun protection measures, including sunscreen application, are usually the cornerstones of dermatological education programs designed for OTRs (see the section ‘Educational and Behavioral Aspects in Skin Cancer Prevention’). | |
The significance of UVR is further emphasized by the observation that after the first SCC, the rate of subsequent NMSC can be decreased if patients change their behavior and protect themselves from the sun [16]. Unfortunately, several studies highlighted the poor compliance among OTRs with advice of sun protection measures [17, 18]. In addition, a high number of OTRs are no longer integrated into a daily occupational routine after transplantation. Recreational sun exposure - either in their home environment or during prolonged vacations - gains predominant importance for OTRs. This is supported by previous findings that OTRs who participated in outdoor recreation were more likely to subsequently develop NMSC [17, 19]. UVR is presumably the only factor that is to a certain degree ‘avoidable’. Sun avoidance and sun protection measures, including sunscreen application, are usually the cornerstones of dermatological education programs designed for OTRs.
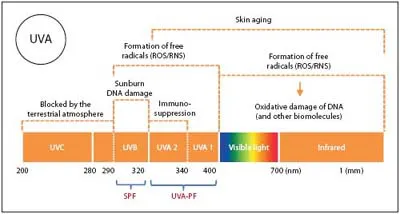
Fig. 1. UVR refers to solar radiation with wavelengths in the 200 to 400 nm range. Radiation in the 400 to 700 nm range is referred to as visible light. UVR is subdivided into UVC, UVB and UVA radiation. Penetration of UVR into skin is wavelength dependent and hence leads to different biological effects (e.g. sunburn, DNA damage, immune suppression, formation of free radicals, oxidative damage of DNA and other biomolecules). SPF is largely a measure of UVB protection. In Europe, a sufficient UVA protection of a sunscreen product is labeled with a dedicated UVA label as depicted above.
In this chapter, background information on (A) UVR, (B) photoprotection and accompanying concerns regarding vitamin D, as well as educational and behavioral aspects of photoprotection in OTRs will be delivered - some common misconceptions and mistakes regarding photoprotection are addressed as well.
Ultraviolet Radiation
Physics of Ultraviolet Radiation
The electromagnetic spectrum covers a wavelength band of radiation ranging from 10-14 m (gamma radiation) to 104 m (radio waves). UVR refers to solar radiation with wavelengths in the 200 to 400 nm range. Radiation in the 400 to 700 nm range is referred to as visible light. UVR is subdivided into UVC, UVB and UVA radiation (fig. 1). Penetration of UVR into skin is wavelength dependent and hence leads to different biological effects [20-22]. The UVC band (200-290 nm) is known as the germicidal band and is primarily absorbed by the ozone layer (NB: industrial workers may experience UVC exposure, e.g. welding, UV drying of paint or finish). The UVB band (290-320 nm) - reaching the epidermis - is known as the erythemal band and is significantly attenuated by the atmosphere. UVA (320-400 nm) - reaching the basal layer of the epidermis and the upper dermis - is known as black light. It is further subdivided into UVA-1 (340-400 nm) and UVA-2 (320-340 nm). The shorter wavelengths of UVA-2 are more erythemogenic than UVA-1. Although UVA is more prevalent at the earth’s surface, it is less effective than UVB in eliciting erythema in human skin [23].
Biological Effects of Ultraviolet Radiation
UVR exerts a number of important biological effects on the skin, influencing the immune system and vitamin D metabolism, as well as causing DNA damage, photoaging, skin cancer, and pigmentary changes through biologically complex mechanisms [24]. In addition, there are psychological effects, with many people reporting enhanced well-being after sun exposure, and social influences, with 20th and 21st century fashion dictating that in some cultures a suntan is attractive and a sign of increased socioeconomic status [25].
Since the 1890s, even before the discovery of DNA and the concept of genetic mutations, sunlight exposure was implicated in the etiology of skin cancer [26, 27]. Over time, significant scientific evidence has been collected and has linked UVR with skin cancer formation [28].
The exact mechanism of UVR-induced cutaneous carcinogenesis is multifactorial and has not been totally elucidated. It is a complex interplay between gene mutation, inflammation, and immunosuppression. Erythema is the clinically visible immediate effect on the skin from UVR. Evidence suggests that clinical erythema correlates with DNA damage. Wavelengths of UVR that are most efficient at producing erythema are also the most efficient at producing pyrimidine dimers [29, 30]. However, some of the deleterious effects of UVR occur before the erythema threshold is reached. Such suberythemal effects of UVR include inflammation, photoaging, diminished antigen responsiveness and depletion of epidermal Langerhans cells [31]. The tumor suppressor, p53 protein, is also induced, which is a strong indication that DNA damage is occurring during suberythematous ultraviolet (UV) exposures [32]. Although much of the literature documents the effects of UVB on skin, many studies in recent years have highlighted the role UVA radiatio...
Table of contents
- Cover Page
- Front Material
- Organ Transplantation and Skin – Principles and Concepts
- Skin Problems in Immunodeficient Patients
- Critical Skin Cancer in Organ Transplant Recipients – A Dermatopathological View
- Immunosuppressive Drugs in Organ Transplant Recipients – Rationale for Critical Selection
- Human Papillomavirus and Squamous Cell Cancer of the Skin – Epidermodysplasia Verruciformis-Associated Human Papillomavirus Revisited
- Pre- and Posttransplant Management of Solid Organ Transplant Recipients: Risk-Adjusted Follow-Up
- Future Trends in Organ Transplant Recipients – Important Issues for Dermatologists
- History of Hematopoietic Stem Cell Transplantation: Evolution and Perspectives
- Acute and Chronic Skin Graft-versus-Host Disease - Pathophysiological Aspects
- Cutaneous Graft-versus-Host Disease - Clinical Considerations and Management
- UV Treatment of Chronic Skin Graft- versus-Host Disease - Focus on UVA1 and Extracorporeal Photopheresis
- Late Effects after Hematopoietic Stem Cell Transplantation - Critical Issues
- Drug Hypersensitivity Reactions during Hematopoietic Stem Cell Transplantation
- Future Trends in Hematopoietic Stem Cell Transplantation
- Photoprotection in Transplant Recipients
- Author Index
- Subject Index