
eBook - ePub
Diabetes and Physical Activity
- 166 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Diabetes and Physical Activity
About this book
Presenting current knowledge regarding the relationship between exercise and diabetes, this publication discusses in detail the physiologic, molecular and genetic mechanisms involved in this interaction. Further, the book presents valuable information on the role of exercise in the treatment and management of diabetes through the life course, including gestational diabetes, diabetes in children, and in the elderly. Notably, the role of diet in modulating the relationship between exercise and diabetes is explored, and for the first time, the importance of sedentary behavior, rather than exercise, is highlighted. The current public health guidelines for type 2 diabetes are presented, as well as practical recommendations for the management of type 1 diabetes. Finally, in each chapter areas of further investigations are emphasized. The book provides a valuable and up-to-date overview and is highly recommended to researchers, students, clinicians, including physicians, dieticians, biokineticists, physiotherapists, nurses and diabetes educators.
Tools to learn more effectively

Saving Books

Keyword Search

Annotating Text

Listen to it instead
Information
Goedecke JH, Ojuka EO (eds): Diabetes and Physical Activity.
Med Sport Sci. Basel, Karger, 2014, vol 60, pp 141-153 (DOI: 10.1159/000357344)
Med Sport Sci. Basel, Karger, 2014, vol 60, pp 141-153 (DOI: 10.1159/000357344)
______________________
Exercise for People with Type 1 Diabetes
Ian W. Gallen
Royal Berkshire NHS Foundation Trust Centre for Diabetes and Endocrinology, Royal Berkshire Hospital, Reading, UK
______________________
Abstract
Exercise in people with type 1 diabetes (T1DM) can produce large changes in blood glucose, with hypo-and hyperglycaemia before and following exercise. Different exercise types, intensity and duration have significantly different effects on blood glucose control, and on the endocrine response to exercise. Exercise performance can also be impaired in T1DM. There have been significant recent improvements in the knowledge of what underlies these changes and in the appropriate management to support the maintenance of euglycaemia. Further advances in insulin infusion pump therapy and continuous subcutaneous glucose monitoring are likely to be useful in the management of people with T1DM who want to exercise.
© 2014 S. Karger AG, Basel
People with type 1 diabetes mellitus (T1DM) are tasked with a complex self-management regime to optimize glycaemic control, to reduce the onset of disabling complications whilst minimizing the risk of hypoglycaemia. They must inject insulin or use an insulin infusion pump (continuous subcutaneous insulin infusion, CSII), pay careful attention to their food intake and in particular carbohydrate consumption. They are guided by the results of capillary blood glucose testing augmented for some with continuous subcutaneous glucose monitoring systems (CGMS). Each of these stages is prone to variation. Insulin absorption in an individual is variable from site to site, but also with exercise [1-3]. It may be difficult to accurately assess the quantity of carbohydrate intake and action [4], although this can be mitigated with skills training which teach insulin dose adjustment and carbohydrate counting [5, 6]. Finally, the information to guide treatment decisions gained from capillary blood glucose testing and from CGMS calibrated from these tests may not always be reliable [7, 8]. These variations and others can and do cause marked disparity in blood glucose control on otherwise apparently similar days (table 1).
When a person with T1DM attempts physical activity, they are faced with further difficulties in maintaining glycaemic control. Different types and duration of exercise produce varying changes in blood glucose, with either hypoglycaemia or hyperglycaemia occurring during or following exercise. These seemingly inexplicable variations in glycaemic control may make managing diabetes in the context of exercise and sporting activities challenging. Concern about hypoglycaemia and previous poor experience may restrict the desire of people with T1DM to take part in exercise and discourage involvement or progression in any chosen sporting activity [9].
Table 1. Some non-exercise factors which contribute to variability in glycaemic control in type 1 diabetes
Factor | Effect |
Subcutaneous insulin injection | Difference in injection site and depth may alter insulin absorption characteristics; rapidly acting insulin may take longer to act or basal insulin may not last as long as expected |
Carbohydrate intake | Variation in carbohydrate quantity and type will alter postprandial glycaemia excursions, with hypo- or hyperglycaemia |
Self-monitored capillary glucose measurements | Errors in sampling or measurement may result in inappropriate insulin dose estimations |
Medication and alcohol | May result in altered glucose response to insulin administration |
Physiological cycles | Diurnal endocrine variation, menstrual cycle and pregnancy |
Changes in work pattern | Will require changes in timing of insulin basal dose administration |
Intercurrent illness | Will require changes in both basal and bolus insulin dose |
Given this unstable basis, and the well-recognised and strong tendency to dysglycaemia with exercise, it might seem ambitious to advise people with T1DM on how to adjust therapy and food ingestion so that they can perform physical exercise or sport safely. Over the last decade, we have developed a specialist diabetes and sports clinic for people with T1DM. In this clinic, we have found that people complain of three main groups of symptoms: (1) rapid changes in blood glucose during and immediately following exercise; (2) severe hypoglycaemia, particularly at night; (3) excessive fatigue and impaired physical performance.
The skills and practice gained from this clinic, combined with excellent clinical research, offer us the opportunity of suggesting a clinic model to healthcare professionals, to help people manage T1DM and exercise more effectively.
Effect of Exercise on Glycaemic Control in T1DM
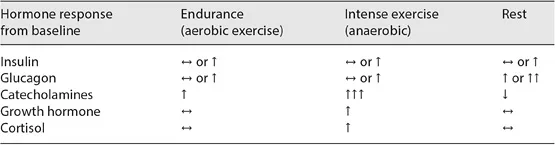
It is predictable that the endocrine and metabolic response to exercise will be altered in T1DM, affecting glycaemic control (table 2). Injected insulin sits in subcutaneous depots, from where absorption continues or may actually increase during exercise [3]. There may be either relatively excessive (with endurance exercise) or deficient (with intense exercise) levels relative to the counter-regulatory hormone response and glucose concentration [10, 11]. Glucagon levels may not change, with the result that the insulin to glucagon ratio presented to the liver is inappropriately high, and thus hepatic glucose production may not be increased adequately during exercise to cope with the increased fuel requirement [10]. This inappropriately high plasma insulin level will promote glucose uptake by non-exercising muscles and other tissues [12]. The catechol-amine and growth hormone responses to exercise are also deficient in T1DM [13, 14]. During prolonged sub-maximal exercise, the relatively high ambient plasma insulin levels combined with a deficient counter-regulatory hormonal response will provoke a marked fall in blood glucose.
Table 2. Endocrine response to exercise in T1DM
To some extent, the endurance athlete has almost a similar endocrine state as the person with untreated T1DM, but does not accumulate glucose and ketone bodies because these are all oxidized. It is important to restate that exercise-induced translocation of GLUT-4 receptors to the cell surface enables non-insulin mediated increased muscle glucose uptake [15]. This suggests that the optimum management of people with T1DM during exercise to maximise performance and reduce the risk of hypoglycaemia may be to replicate this physiological hypo-insulinaemic state during exercise. However, insulin levels must be restored quickly to deal with post-exercise hyperglycaemia.
Intense exercise produces a greater counter-regulatory hormone response than sub-maximal endurance exercise [16, 17]. This effect is preserved but diminished in T1DM, and has important implications for glycaemic control [16, 18-20]. Intermittent high-intensity exercise is associated with a lesser fall in glucose than moderate exercise of a similar workload. When people with T1DM were exercised for 30 min by continuous sub-maximal exercise or with 4-second sprints performed every 2 min, the decline in blood glucose was less with the intense exercise. Glucose levels remained stable during recovery, but continued to fall after sub-maximal exercise alone. The mechanism for this stabilisation of blood glucose levels appears to be mediated through increased secretion of catecholamines and growth hormone during early recovery after exercise [21].
Short periods of intense exercise performed before, or following, endurance exercise can also attenuate the decline in blood glucose that occurs following exercise. When a maximal 10-second cycling sprint was performed immediately following exercise of moderate intensity, the fall in blood glucose was less in the 2 h following exercise when compared to that observed following moderate intensity exercise without the brief sprint. A similar protective effect is observed if the 10-second sprint is performed before continuous exercise [18, 19].
This protective effect of high-intensity exercise seems to be lost in the late post-exercise period. Nocturnal hypoglycaemia is more frequent following intermittent high intensity exercise than after moderate exercise. When glucose profiles were examined using CGM during, and in the 20 h after, a 30-min session of either intermittent high-intensity exercise or moderate-intensity exercise, glucose levels declined during both types of exercise. However, between midnight and 6.00 a.m. the glucose levels were significantly lower after the period of intermittent exercise, and the number of hypoglycaemic epi-sodes was greater than after lower-intensity exercise [22].
While differences exist between glycaemic responses in people with T1DM during, and following different forms of exercise, there are also differences in responses when aerobic and resistance exercise are performed in the same session, but in different exercise order [23]. When aerobic exercise occurs before resistance exercise, blood glucose falls during aerobic exercise but stabilizes during later resistance exercise. Post-exercise blood glucose was lower than before exercise. In contrast, when these exercises take place in reverse order, with resistance exercise first, blood glucose increases, but then falls during subsequent aerobic exercise, with blood glucose being similar to baseline values. CGMS demonstrated a trend to less nocturnal hypoglycaemia when resistance training had taken place first. These data suggest that performing resistance exercise before aerobic exercise improves glycaemic stability throughout exercise and reduces t...
Table of contents
- Cover Page
- Front Matter
- The Relationship between Exercise, Nutrition and Type 2 Diabetes
- Sedentary Behavior as a Mediator of Type 2 Diabetes
- Increasing Prevalence of Type 2 Diabetes in Sub-Saharan Africa: Not Only a Case of Inadequate Physical Activity
- Exercise Interventions to Prevent and Manage Type 2 Diabetes: Physiological Mechanisms
- Relationships between Exercise, Mitochondrial Biogenesis and Type 2 Diabetes
- Interaction between Lipid Availability, Endurance Exercise and Insulin Sensitivity
- Mechanisms in Exercise-Induced Increase in Glucose Disposal in Skeletal Muscle
- The Effect of Exercise on Obesity, Body Fat Distribution and Risk for Type 2 Diabetes
- Gene-Physical Activity Interactions and Their Impact on Diabetes
- Physical Activity and Gestational Diabetes Mellitus
- Physical Activity in Children: Prevention of Obesity and Type 2 Diabetes
- Diabetes and Exercise in the Elderly
- Public Health Recommendations for Physical Activity in the Prevention of Type 2 Diabetes Mellitus
- Exercise for People with Type 1 Diabetes
- Author Index
- Subject Index
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn how to download books offline
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 990+ topics, we’ve got you covered! Learn about our mission
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more about Read Aloud
Yes! You can use the Perlego app on both iOS and Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app
Yes, you can access Diabetes and Physical Activity by J. H. Goedecke,E. O. Ojuka,J.H., Goedecke,E.O., Ojuka, D. J. Caine,A. P. Hills,T. Noakes,D.J., Caine,A.P., Hills,T., Noakes in PDF and/or ePUB format, as well as other popular books in Medicine & Nutrition, Dietics & Bariatrics. We have over one million books available in our catalogue for you to explore.