eBook - ePub
Comorbidity of Mental and Physical Disorders
- 200 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Comorbidity of Mental and Physical Disorders
About this book
This publication presents evidence about the magnitude and severe consequences of comorbidity of mental and physical illnesses from a personal and societal perspective. Leading experts address the huge burden of co-morbidity to the affected individual as well as the public health aspects, the costs to society and interaction with factors stemming from the context of socioeconomic developments. The authors discuss the clinical challenge of managing cardiovascular illnesses, cancer, infectious diseases and other physical illness when they occur with a range of mental and behavioral disorders, including substance abuse, eating disorders and anxiety. Also covered are the organization of health services, the training of different categories of health personnel and the multidisciplinary engagement necessary to prevent and manage comorbidity effectively. The book is essential reading for general practitioners, internists, public health specialists, psychiatrists, cardiologists, oncologists, medical educationalists and other health care professionals.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Comorbidity of Mental and Physical Disorders by N. Sartorius,R. I. G. Holt,M. Maj,N., Sartorius,R.I.G., Holt,M., Maj, A. Riecher-Rössler,N. Sartorius,A., Riecher-Rössler,N., Sartorius in PDF and/or ePUB format, as well as other popular books in Medicina & Cardiologia. We have over one million books available in our catalogue for you to explore.
Information
Comorbidity of Mental and Physical Illness: A Selective Review
Sartorius N, Holt RIG, Maj M (eds): Comorbidity of Mental and Physical Disorders.
Key Issues Ment Health. Basel, Karger, 2015, vol 179, pp 42-53 (DOI: 10.1159/000365529)
Key Issues Ment Health. Basel, Karger, 2015, vol 179, pp 42-53 (DOI: 10.1159/000365529)
______________________
Depression, Diabetes and Dementia
Joshua D. Rosenblata, d · Rodrigo B. Mansura, f, g · Danielle S. Chaa, b · Anusha Baskarana, e · Roger S. McIntyrea-c
aMood Disorders Psychopharmacology Unit (MDPU), University Health Network, bInstitute of Medical Science, and cDepartment of Psychiatry and Pharmacology, University of Toronto, Toronto, Ont., dSchulich School of Medicine and Dentistry, Western University, London, Ont., and eCentre for Neuroscience Studies, Queen's University, Kingston, Ont., Canada; fInterdisciplinary Laboratory of Clinical Neuroscience (LINC) and gProgram for Recognition and Intervention in Individuals in At-Risk Mental States (PRISMA), Department of Psychiatry, Federal University of Sao Paulo, Sao Paulo, Brazil
______________________
Abstract
Depression, diabetes and dementia are three disorders associated with staggering morbidity and mortality worldwide. The association between depression and diabetes has been well established. Furthermore, both depression and diabetes have been shown to increase the incidence of dementia individually and synergistically. The metabolic-brain axis appears to be a key mediator connecting depression, diabetes and dementia. Brain regions important for cognition and emotional regulation may be damaged by the effects of hyperglycemia and insulin resistance. Indeed, insulin resistance and decreased insulin in the central nervous system (CNS) results in decreased intracellular glucose levels in frontal and subcortical regions, neurotoxicity, decreased neuro-plasticity, decreased signaling, decreased synaptic connectivity and disturbances in neural circuitry. The aforementioned changes may be attributable to brain bioenergetics wherein there is a bias toward energy conservation. The insulin pathway also has a bidirectional interaction with amyloid-β oligomer formation, one of the hallmarks of Alzheimer's disease. As well, depression may further facilitate neural circuit damage through the inflammatory pathway, hypothalamic-pituitary-adrenal axis dysregulation, monoamine changes and lowering of neurotrophic support to the CNS. Stress and psychosocial determinants of health may also be key mediators in how these systems interact. The involvement of several pathways may present new potential drug targets for the treatment and prevention of dementia using a lifetime approach. Systemic and intranasal insulin, oral diabetic medications, exercise, dietary changes, bariatric surgery and improved screening practices with early treatment of depression and diabetes all show promise in the treatment and prevention of comorbid depression, diabetes and dementia.
© 2015 S. Karger AG, Basel
Depression has been recognized by the World Health Organization (WHO) as one of the leading causes of disability worldwide, affecting an estimated 350 million people globally [1]. Depression has also been identified as a risk factor and poor prognostic indicator for several medical comorbidities including, but not limited to, metabolic disorders such as diabetes, metabolic syndrome and obesity [2]. According to WHO estimates, diabetes, which now affects more than 350 million people globally, will be the seventh leading cause of death by 2030 [3]. Moreover, depression and diabetes have a well-established link as numerous investigators have shown a bidirectional association between these disorders [4]. Both depression and diabetes have been independently associated as risk factors for the development of cognitive impairment and dementia [5, 6]. Furthermore, depression and diabetes have been recognized as having a synergistic effect in increasing the risk for dementia above and beyond the effects that depression or diabetes would have on the risk of developing dementia independently. More specifically, comorbid type 2 diabetes mellitus and major depressive disorder have been documented to increase the incidence of Alzheimer's disease greatly later in life [7].
Alzheimer's disease is the leading cause of dementia, the sixth leading cause of mortality and the third most costly disease in the USA [8-10]. It is progressive in nature and is ultimately fatal [10]. Currently, available treatments are only palliative as there are no agents that have been shown to have disease-modifying properties [11]. Therefore, primary prevention represents a priority research vista for identifying and targeting modifiable risk factors of Alzheimer's disease. Modifiable risk factors that are addressed in this review are type 2 diabetes and major depressive disorder.
The overarching aim of this review is to review the potential pathophysiologic mechanisms which may account for this observed association between Alzheimer's disease, type 2 diabetes and major depressive disorder. There is also a brief discussion about preventative and therapeutic options with particular emphasis on a lifetime approach to dementia. Evidence for the association between diabetes, depression and dementia has been extensively reviewed and can be found elsewhere [7, 12-14].
Mechanisms Linking Depression, Diabetes and Dementia
Evidence from preclinical and clinical studies has suggested several potential mechanisms connecting diabetes, depression and dementia. Essential to this discussion is the recognition that the neural networks implicated in cognitive and emotional function and dysfunction have significant overlap, as shown in figure 1 [15], which is central to the observed interactions between cognition and mood. It has been amply documented that cognitive dysfunction and changes in mood are key symptoms that have been observed to appear together in individuals diagnosed with major depressive disorder [6, 16]. Therefore, the observed symptoms of Alzheimer's disease and major depressive disorder may be associated with a spectrum of structural and functional changes of shared neural circuits of the frontal and subcortical regions [6, 16]. Likewise, the epidemiological observation and proposal of major depressive disorder as a prodrome of Alzheimer's disease may be indicative of progressive damage to these neural circuits with repeated major depressive episodes [6, 13, 16].
In addition, central to the discussion of mechanisms involved in diabetes, depression and dementia is the bidirectional relationship of the body's metabolic milieu and neural circuitry [17]. Pathologic metabolic processes may damage these foregoing neural circuits. Evidence for such damage to neural circuits is shown through impaired cognition and altered brain connectivity in people with diabetes, independent of vascular pathology, as demonstrated through functional imaging techniques, such as electroencephalography, magnetoencephalography and functional magnetic resonance imaging [18, 19]. The damage to frontosubcortical circuits by metabolic pathology, namely diabetes, insulin resistance, and obesity, may thus impair cognition and affect mood [18, 20].
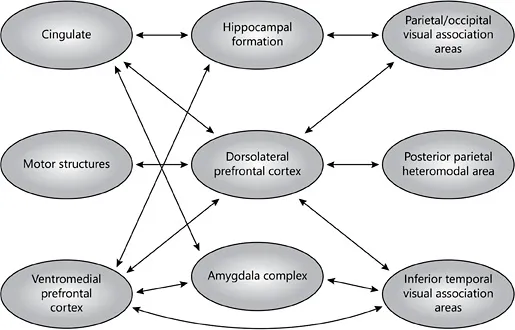
Fig. 1. The neural basis of cognitive and emotional processes. Reprinted with permission from Wood and Grafman [15].
Impaired Central Insulin and Glucose Supply
Insulin, produced by the pancreas, enters the blood stream allowing for its systemic circulation and systemic effects [21]. To enter the central nervous system (CNS), blood-borne insulin is transported across the blood-brain barrier via a saturable, receptor-mediated process [15]. Once in the CNS, insulin may exert a plethora of important effects, including, but not limited to, promoting glucose uptake in specific regions, neurogenesis, neuroplasticity, synaptic strengthening and preventing neurodegeneration [22, 23]. CNS insulin and glucose have also been proposed to be an important modulator of the reward system and appetite [24].
The previous understanding that insulin had no effect on the brain has now been abolished with the discovery of insulin receptors in numerous brain regions [25]. Notably, insulin receptors have been identified in regions involved with cognition and emotion including the hypothalamus, olfactory bulb, cerebral cortex, substantia nigra, basal ganglia, hippocampus and amygdala [25]. As such, altered insulin levels and signaling, as seen in type 2 diabetes, may have important CNS consequences.
Type 2 diabetes is characterized by hyperglycemia, insulin resistance with compensatory hyperinsulinemia, and subsequent pancreatic decompensation, resulting in hypoinsulinemia at later stages, unless treated [21]. Preliminary evidence indicates that the blood-brain barrier insulin transporters may be downregulated in chronic hyperinsulinemia [15] and that, consequentially, CNS insulin levels may be decreased [26-28]. As previously discussed, CNS insulin is an important signaling molecule in nume...
Table of contents
- Cover Page
- Front Matter
- Background
- Comorbidity of Mental and Physical Illness: A Selective Review
- Management of Comorbidity of Mental and Physical Illness
- Concluding Remarks
- Author Index
- Subject Index