eBook - ePub
Surgery for Pediatric Velopharyngeal Insufficiency
- 92 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Surgery for Pediatric Velopharyngeal Insufficiency
About this book
This surgical atlas describes the multidisciplinary approach to treating pediatric velopharyngeal insufficiency (VPI) and reviews the diagnostic and therapeutic modalities involved. The publication begins with a review of the key anatomic features of children with VPI and focuses on a clinically relevant approach to surgical anatomy. How to perform nasal endoscopy and how to decide between different surgical treatments are key diagnostic questions when treating VPI, which are discussed in detail in this volume. Included with the published text are 5- to 7-minute-long narrated audio/video recordings of each surgery. The videos show the key surgical steps as well as the pearls and pitfalls of each surgical intervention. This publication gives an excellent overview of the various types of procedures, and it should prove to be essential reading for VPI surgeons, both the novice and experienced, who need to understand the relevant anatomy and the pearls and pitfalls of each of the various surgical procedures.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Surgery for Pediatric Velopharyngeal Insufficiency by N. Raol,C. J. Hartnick,N., Raol,C.J., Hartnick, Patrick J. Bradley,Patrick J., Bradley in PDF and/or ePUB format, as well as other popular books in Medicine & Ear, Nose & Throat Medicine. We have over one million books available in our catalogue for you to explore.
Information
Raol N, Hartnick CJ (eds): Surgery for Pediatric Velopharyngeal Insufficiency.
Adv Otorhinolaryngol. Basel, Karger, 2015, vol 76, pp 7-17 (DOI: 10.1159/000368004)
Adv Otorhinolaryngol. Basel, Karger, 2015, vol 76, pp 7-17 (DOI: 10.1159/000368004)
______________________
Nasometry, Videofluoroscopy, and the Speech Pathologist's Evaluation and Treatment
Marie de Stadler · Cheryl Hersh
Department of Speech Language and Swallowing Disorders, Massachusetts General Hospital, Boston, Mass., USA
______________________
Abstract
The speech-language pathologist (SLP) plays an important role in the assessment and management of children with velopharyngeal insufficiency (VPI). The SLP assesses speech sound production and oral nasal resonance and identifies the characteristics of nasal air emission to guide the clinical and surgical management of VPI. Clinical resonance evaluations typically include an oral motor exam, identification of nasal air emission, and analysis of the speech sound repertoire. Additional elements include perceptual assessment of intra-oral air pressure, the degree of hypernasality, and vocal loudness/quality. Clinical speech and resonance evaluations are typically the gold-standard evaluation method until a child reaches 3-4 years of age, when sufficient compliance levels and speech-language abilities allow for participation in instrumental testing. At that time, objective assessment measures are introduced, including nasometry, videofluoroscopy, and/or nasopharyngoscopy. Nasometry is a computer-based tool that quantifies nasal air escape and allows comparison of the score against normative data. Videofluoroscopy is a radiographic tool used to assess the shaping of the velum and closure of the velopharyngeal mechanism during speech production. Evaluation findings guide decision making regarding surgical candidacy and/or the therapeutic management of VPI. Surgery should always be pursued first when an anatomic deficit prevents velopharyngeal closure. Therapy should always be pursued in children who present with velopharyngeal mislearning and/or motor planning issues resulting in VPI. It is not uncommon for children to receive a combination of surgical intervention and speech resonance therapy during their VPI management course. Collaborative decision making between the otorhinolaryngologist and the SLP provides optimal patient care.
© 2015 S. Karger AG, Basel
Introduction
The role of the speech-language pathologist (SLP) in the management of pediatric ve-lopharyngeal insufficiency (VPI) is a continuously changing role and one that is based on the evolution of a child's clinical presentation and therapeutic needs. One of the earliest functions of SLP involvement with children with cleft palate and/or craniofacial anomalies is initiation of speech-language therapy as early as at 9 months of age to promote the development of early speech and language skills. It is well documented in the literature that children with a history of cleft palate are at risk for delayed expressive language development [1]. The risk of language delay stems from a variety of potential factors, including frequent ear infections, psychosocial challenges, lengthy or repeated hospitalizations, cognitive deficits, and/or impaired speech production abilities in the setting of the cleft [1, 2]. Children with a syndromic diagnosis are at a higher risk of language delay than children with an isolated cleft lip and/or palate [2,3]. The focus of speech-language therapy for children under the age of three is typically centered around language stimulation and the quantity of early speech and language skills acquired [4]. Clinical speech and resonance evaluations are utilized during this time to track a child's speech sound repertoire and monitor oral nasal resonance.
Figure 1a is a visual representation of the components of VPI assessment and management when a child reaches 3-4 years of age. At this time, sufficient compliance levels and speech-language skills allow for participation in more structured testing. Instrumental assessment methods are then introduced, including nasometry, video-fluoroscopy, and nasopharyngoscopy, to objectively assess velopharyngeal closure and nasal airflow rates. These methods, in conjunction with clinical speech and resonance evaluation findings, are used to determine whether the next step in treatment planning includes surgical intervention and/or speech resonance therapy intervention. Whether surgery or therapy is pursued, the components of the model depicted apply to several different scenarios, including the determination of baseline speech and resonance performance, the evaluation of treatment versus surgical candidacy, and the assessment of post-operative progress. The child may cycle through this model at different phases throughout the course of his or her VPI management. The oto-rhinolaryngologist (ORL) and SLP collaborate at many points in order to best inform clinical decision making. The best patient care is provided when patients are matched with appropriate clinical treatment courses. Surgery is the gold-standard intervention for children whose speech and resonance profile is the result of physiological limitations of the velopharyngeal mechanism. Speech resonance therapy intervention is the primary avenue of management when the etiology of VPI is related to oral motor planning issues and/or phoneme-specific nasal air emission (PSNAE). Speech resonance therapy should also be pursued as a component of care when the child is stimulable for modifications in speech and resonance using therapeutic techniques. The videos available throughout the chapter allow the reader to explore different assessment and therapy techniques, including the use of instrumental and clinical methods.
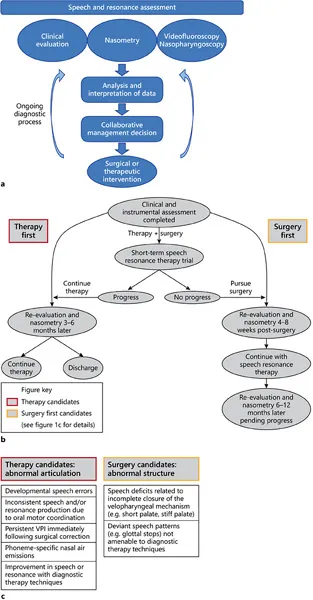
Fig. 1. Speech and resonance assessment when a child exhibits sufficient compliance levels and speech-language abilities allow for participation in instrumental testing.
Assessment
Clinical speech and resonance evaluations typically include an oral motor exam; identification of nasal air emissions and/or turbulence; and perceptual assessment of vocal loudness, vocal quality, intra-oral air pressure, and the degree of hypernasality perceived [5, 6]. A speech sound inventory is also collected during clinical evaluation to assess speech development and identify whether speech errors are developmental in nature or structurally based in the setting of the cleft or velopharyngeal anomaly. Developmentally appropriate speech errors should not be viewed as concerning when within the normal expected age range for a child. Obligatory errors are the result of anatomical or dental limitations, whereas compensatory speech errors are the result of velopharyngeal mislearning and/or oral motor planning difficulties. Atypical speech errors and compensatory mis-articulations are eligible for remediation. Clinical speech and resonance evaluations typically serve as the primary means of assessment for the child under 3-4 years of age due to limitations in compliance and developmental speech-language expectations.
Clinical Speech and Resonance Evaluation
An oral motor exam generally includes assessment of the oral and facial anatomy (including the hard/soft palate and dental occlusion) as well as evaluation of the strength/coordination of the oral articulators for speech production.
Nasal air emissions and/or turbulence are evaluated through analysis of spontaneous speech samples and identification of nasal air escape with production of non-nasal speech sounds via a nasal mirror exam [6-8]. Online supplementary video 1 (for all online supplementary material, see http://www.karger.com/Article/FullText/368004) is an example of a nasal mirror exam. By placing the nasal mirror under the nares during production of sentences containing exclusively oral consonants, the clinician is able to assess the presence, quantity, and symmetry of nasal air emission. In a patient with normal velopharyngeal functioning, there should be no visible nasal air emission with production of these sentences.

Additional characteristics of the perceptual examination include assessment of vocal quality, vocal volume, the degree of hypernasality, and intra-oral air pressure during structured and spontaneous speech tasks. Children with a history of VPI may present with reduced vocal loudness or a shorter length of utterance due to incompetent valving of the velopharyngeal mechanism. Hoarseness and/or breathiness may also be present in this population secondary to compensatory valving mechanisms, which may result in pathologies such as vocal nodules [5, 9]. Intra-oral air pressure is evaluated via the use of standard phrases weighted with sibilant speech sounds (e.g. Suzy sees a horse) and plosive consonants (e.g. Pick up the puppy). All standardized phrases contain exclusively orally produced phonemes. Perceptual evaluation scales often assist with quantifying the degree of VPI. It should be noted that nasal turbulence is generally reflective of a small velopharyngeal gap, whereas overt nasal air emission is indicative of a larger anatomical deficit [10, 11]. One of the most commonly used perceptual evaluation scales is that of McWilliams and Phillips [12], which is sometimes referred to as the Pittsburgh Weighted Speech Scale.
Nasometry
Nasometry is a non-invasive computer-based measurement tool that quantifies nasal acoustic energy in speech [7, 13]. The nasometer, as seen in online supplementary video 2 (for all online supplementary material, see http://www.karger.com/Article/FullText/368004), comprises a headset with an oral and nasal microphone that connects to the computer through a converter. The patient wears the headset with the aforementioned microphones and repeats standardized speech samples. As the patient produces the utterances, the clinician visually determines the pattern of nasal air emission and whether specific speech sounds and/or changes in rate or volume affect the overall nasalance markings in real time. At the conclusion of the standardized utterance, a nasalance score is generated, and the score is then compared with normative data using the Ma...
Table of contents
- Cover Page
- Front Matter
- Anatomy and Physiology of Velopharyngeal Closure and Insufficiency
- Nasometry, Videofluoroscopy, and the Speech Pathologist's Evaluation and Treatment
- Nasal Endoscopy: New Tools and Technology for Accurate Assessment
- New Technology: Use of Cine MRI for Velopharyngeal Insufficiency
- Validated Patient-Reported Outcome Instruments for Velopharyngeal Insufficiency
- Prosthodontics Rehabilitation in Velopharyngeal Insufficiency
- Superiorly Based Pharyngeal Flap
- Sphincter Pharyngoplasty
- Furlow Double-Opposing Z-Plasty
- Posterior Pharyngeal Wall Augmentation
- Persistent Velopharyngeal Insufficiency
- Obstructive Sleep Apnea
- Author Index
- Subject Index