eBook - ePub
Food Allergy: Molecular Basis and Clinical Practice
- 278 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Food Allergy: Molecular Basis and Clinical Practice
About this book
While first accounts of food allergy date back to antiquity, only in recent years has food allergy become recognized as one of the major allergic diseases. During the last decade the output of research papers on food allergy increased tremendously, and today, issues related to food allergies still attract a lot of attention among academics and the general public. Featuring contributions by world-renowned experts, this book presents the current concept, practice and recent advances in the field of food allergy. A comprehensive background section provides a historical retrospective and information on the immunological basis and epidemiology of food allergies. Main topics discussed include clinical aspects, diagnosis and management, allergen-based food allergies, and disease-based food allergies. Furthermore, nutritional aspects and diets, public policy and educational programs are covered as well as recent hot topics such as molecular-based allergen diagnosis, eosinophilic gastrointestinal food allergies and oral immunotherapy. Allergists, pediatricians, internists, dermatologists and general practitioners will find this publication an essential source of information as it provides in-depth insights into food allergies from childhood to adulthood.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Food Allergy: Molecular Basis and Clinical Practice by M. Ebisawa,B. K. Ballmer-Weber,S. Vieths,R. A. Wood,M., Ebisawa,B.K., Ballmer-Weber,S., Vieths,R.A., Wood, T. A. E. Platts-Mills,T.A.E., Platts-Mills in PDF and/or ePUB format, as well as other popular books in Medicine & Dermatology. We have over one million books available in our catalogue for you to explore.
Information
Allergen-Based Food Allergies
Ebisawa M, Ballmer-Weber BK, Vieths S, Wood RA (eds): Food Allergy: Molecular Basis and Clinical Practice.
Chem Immunol Allergy. Basel, Karger, 2015, vol 101, pp 114-123 (DOI: 10.1159/000375415)
Chem Immunol Allergy. Basel, Karger, 2015, vol 101, pp 114-123 (DOI: 10.1159/000375415)
______________________
Cow's Milk Allergy in Children and Adults
Alessandro Fioochia · Lamia Dahdaha · Marco Albarinib · Alberto Martellic
aDivision of Allergy, Department of Pediatrics, Pediatric Hospital Bambino Gesù, Rome; bMelloni Paediatria, Melloni University Hospital, Milan; cThe Garbagnate, Bollate Santa Corona Hospital, Milan, Italy
______________________
Abstract
Cow's milk allergy is among the more frequent food allergies in infants and children. Because its suspicion stems from a plethora of symptoms, it is frequently reported. However, the development of a rigorous diagnostic pathway will reduce the diagnosed children to less than 50% of those reported. Cow's milk allergy is the only specific food allergy for which an EBM guideline exists. According to the guidelines (Diagnosis and Rationale for Action against Cow's Milk Allergy), a diagnostic process based on the pre-test probability of this condition is available. Treatments include avoidance, the substitution of cow's milk with an appropriate formula, and in some cases, oral immunotherapy. Treatment choice is also guided by these guidelines.
© 2015 S. Karger AG, Basel
Introduction
According to the general definition of food allergy, cow's milk allergy (CMA) is an adverse health effect arising from a specific immune response that occurs reproducibly on exposure to a given food’ [1]. This definition includes both IgE-mediated and non-IgE-mediated immune responses as well as a combination of both, and it is in agreement with international guidelines [2-4] and statements [5]. Thus, CMA is not a single clinical condition but includes a spectrum of IgE, non-IgE and mixed conditions affecting different organs and systems (table 1).
Epidemiology
The estimated prevalence of confirmed CMA varies from 0.25 to 4.9% and is higher in children than in adults. Adult CMA is not an unknown phenomenon, and cow's milk is the second most reported food offender in adults on food allergy surveys [6].
CMA can develop in exclusively or partially breast-fed infants when cow's milk protein is introduced into the feeding regime. The incidence of CMA is lower in exclusively breast-fed infants compared to formula-fed or mixed-fed infants, and clinical reactions in the breast-fed group are mostly mild to moderate. These findings might be related to the lower levels of CMP in breast milk compared to cow's milk. Immunomodulators in breast milk and differences in gut flora between breast-fed and formula-fed infants may also play roles.
Table 1. The spectrum of conditions associated with IgE-mediated reactions to cow's milk [1]
I Systemic IgE-mediated reactions (anaphylaxis) |
A Immediate-onset reactions |
B Late-onset reactions |
II IgE-mediated gastrointestinal reactions |
A Oral allergy syndrome |
B Immediate gastrointestinal allergy |
III IgE-mediated respiratory reactions |
A Asthma and rhinitis secondary to ingestion of milk |
B Asthma and rhinitis secondary to inhalation of milk (e.g. occupational asthma) |
IV IgE-mediated cutaneous reactions |
A Immediate-onset reactions |
1. Acute urticaria or angioedema |
2. Contact urticaria |
B Late-onset reactions |
Atopic dermatitis |
Pathogenesis
Milk can give rise to several food hypersensitivities, which are usually classified as milk allergy or milk intolerance [7]. The immunological basis of CMA distinguishes it from other adverse reactions to cow's milk protein, such as lactose intolerance, which is attributable to a beta-galactosidase (lactase) deficiency [8]. This chapter does not address lactase deficiency or other cow's milk-induced hypersensitivities that are not mediated by immune mechanisms. Other classes of immunoglobulins, immune complexes, or cell-mediated reactions are involved in allergies that are not mediated by IgE. IgE and non-IgE-mediated mechanisms may play roles in the pathogeneses of atopic dermatitis (AD) and eosinophilic gastrointestinal disorders (EGIDs). In IgE-mediated allergy, circulating antibodies recognize specific molecular regions on the antigen surface (epitopes), which are classified according to their specific amino acid sequences (linear epitopes) or the folding and conformation of their protein chains (conformational epitopes).
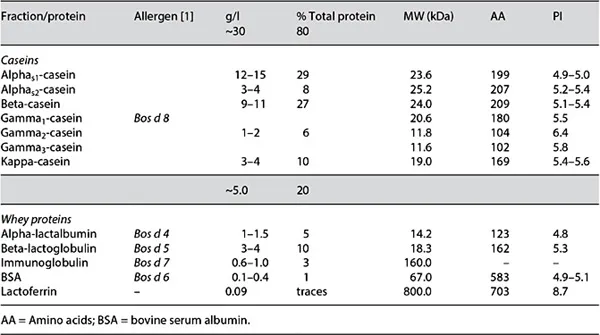
Allergens
Cow's milk contains several proteins, some of which are considered to be major allergens (i.e. IgE prevalence ≥50%), while some are minor allergens, and other milk proteins have hardly or never been associated with clinical reactions. The proteins in the casein and whey fractions of cow's milk are listed in table 2. Each of these two fractions contains five major components [9-11]. The casein fraction contains 80% of the total proteins in cow's milk, while alphas1 and beta-casein comprise 70% of this fraction. Whey proteins are less abundant, and beta-lactoglobulin accounts for 50% of this fraction. Because beta-lactoglobulin is not present in human milk, this protein has been previously considered to be the most important cow's milk allergen, but it has since been shown that other proteins, such as casein, are also dominantly involved in the etiology of the disease.
By convention in the international nomenclature, allergens are designated by an abbreviation formed by the genus (capitalized, with the first three letters abbreviated) and species (reduced to one letter) names of the Linnaean taxonomical system in italics, followed by an Arabic numeral reflecting the chronological order in which the allergen was identified and characterized (e.g. Bos d [omesticus] 4) [11] (see: http://www.allergen.org/). In CMA, the determination of an IgE-mediated response to sequenced and characterized allergens may be more useful in predicting the presence and severity of clinical allergy than the currently used skin test or serological tests performed with whole allergen extracts [12].
Clinical Manifestations
The clinical manifestations of CMA depend to a great extent on the type of immunological reaction involved.
Table 2. The proteins in cow's milk
Immediate Reactions
These reactions occur at <2 hours after ingestion. The most frequent manifestations are IgE-mediated cutaneous (urticaria, angioedema, or an acute flare-up of atopic eczema) and gastrointestinal (GI) (vomiting, diarrhea, or colic) reactions. Cow's milk protein-induced enterocolitis syndrome is an immediate-onset, non-IgE-mediated condition. It is characterized by initial symptoms presenting during the first months of life as repeated vomiting episodes, sometimes leading to dehydration. Symptoms might be very severe and mimic sepsis. A characteristic feature of this syndrome is a symptom-free interval of up to several hours between the ingestion of milk, most often a cow's milk protein-based formula, and the first symptoms [13]. Milk-induced proctocolitis is mostly observed in young infants that are exclusively breast-fed [14]. Respiratory manifestations (asthma or allergic rhinitis) are infrequent, especially as isolated symptoms. There is a belief among some members of the lay public that the consumption of milk and dairy products increases the production of mucus in the respiratory tract; however, this view has not been confirmed by scientific evidence [15]. Anaphylaxis is the most severe manifestation of immediate-type CMA.
Delayed Reactions
These immunological, non-IgE-mediated reactions occur at several hours or days after milk consumption. AD is observed in approximately 10-15% of young children. It is primarily associated with dry skin and is linked to hereditary factors; however, approximately one third of patients with moderate to severe AD present with flares of eczema linked to a food allergy [16]. Cow's milk, hen's egg, and peanuts are the most frequently involved foods. GI disorders include food protein-induced enteropathy and proctocolitis [17]. CMA-enteropathy usually presents with diarrhea, mild to moderate steatorrhea (80% of cases) and poor weight gain. Rectal bleeding is the usual presenting feature of CMA-colitis, and the infant ...
Table of contents
- Cover Page
- Front Matter
- Background
- Clinical Aspects
- Diagnosis and Management
- Allergen-Based Food Allergies
- Disease-Based Food Allergies
- Special Topics
- Acknowledgments
- Author Index
- Subject Index