eBook - ePub
New Insights in Intracerebral Hemorrhage
- 198 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
New Insights in Intracerebral Hemorrhage
About this book
The age-standardized mortality rate for hemorrhagic stroke has decreased worldwide over the past two decades, but incidence, number of deaths, and lost disability-adjusted life-years (DALY) continue to increase. Moreover, hemorrhagic stroke occurs half as frequently globally as ischemic stroke, but causes significantly more deaths and lost DALY. Milestone studies of the past decade - STICH, FAST, and INTERACT2 - indicate the importance of hyperacute care for intracerebral hemorrhage; despite this, there is to date no established strategy for patients analogous to reperfusion therapy for ischemic stroke. This book, written by world-renowned experts, covers all current topics related to the diagnosis and management of intracerebral hemorrhage. It will contribute to an improved understanding of current and future aspects concerning optimal management of patients. This is a comprehensive, up-to-date resource for neurologists, neurosurgeons and trainees.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access New Insights in Intracerebral Hemorrhage by Kazunori Toyoda,C. S. Anderson,S. A. Mayer,Kazunori, Toyoda,C.S., Anderson,S.A., Mayer, Julien Bogousslavsky in PDF and/or ePUB format, as well as other popular books in Medicine & Internal Medicine & Diagnosis. We have over one million books available in our catalogue for you to explore.
Information
Toyoda K, Anderson CS, Mayer SA (eds): New Insights in Intracerebral Hemorrhage.
Front Neurol Neurosci. Basel, Karger, 2016, vol 37, pp 107-129 (DOI: 10.1159/000437117)
Front Neurol Neurosci. Basel, Karger, 2016, vol 37, pp 107-129 (DOI: 10.1159/000437117)
______________________
Ultra-Early Hemostatic Therapy for Intracerebral Hemorrhage: Future Directions
Katja E. Wartenberga · Stephan A. Mayerb
aNeurocritical Care Unit, Department of Neurology, Martin-Luther-University Halle-Wittenberg, Halle, Germany; bInstitute for Critical Care Medicine, The Mount Sinai Hospital, New York, N.Y., USA
______________________
Abstract
Hematoma expansion after initial bleeding is associated with many risk factors, such as anticoagulation, diagnosis by computed tomography (CT) shortly after symptom onset, liver disease, and a high initial blood pressure, among others, and with increased mortality and poor long-term functional outcomes. Contrast extravasation on CT angiogram, termed ‘the spot sign’, and on delayed-contrast CT scans (13-59%) may help to identify impending intracerebral hemorrhage growth and may open a window of opportunity for therapeutic interventions. The spot sign score, the prediction score for hematoma expansion, and the BRAIN score were developed to assess the probability of hematoma expansion at 24 h. Therapeutic interventions to promote hemostasis are currently limited to intensive blood pressure control and antagonization of the effect of antiplatelets and anticoagulation. Ultra-early hemostasis for ICH not associated with coagulopathy may include administration of recombinant factor VIIa and tranexamic acid to selected patients based on the presence of a spot sign on the CT angiogram is currently under investigation.
© 2016 S. Karger AG, Basel
Scope of the Problem: Hematoma Growth
Hematoma volume was identified as the single most powerful predictor of poor functional outcomes and mortality after intracerebral hemorrhage (ICH), followed by the presence of intraventricular hemorrhage (IVH), a depressed level of consciousness, age, and an infratentorial location [1-8].
Moreover, retrospective observational studies revealed that ICHs undergo progressive growth within the first 24 h [9] (fig. 1). In the first prospective study of this phenomenon, at least 38% of 103 patients experienced >33% growth in the ICH volume during the first 24 h after symptom onset. In 26% of patients, ICH growth had already occurred within the first hour, and in 12%, growth had occurred between 1 and 20 h. ICH growth was accompanied by neurological deterioration, as detected based on concurrent National Institutes of Health Stroke Scale and Glasgow Coma Scale scores, in one third of patients within 1 h of the first computed tomography (CT) image and in an additional 25% of patients within the next 20 h [10]. Although all studies examining early ICH growth have found the highest rates within 6 h of onset [10-25], the finding of neurological deterioration with hematoma growth between 6 and 48 h has been substantiated by other studies [11, 13, 17, 18]. Several multivariate analyses have identified factors associated with hematoma enlargement and early neurological deterioration after ICH (table 1).
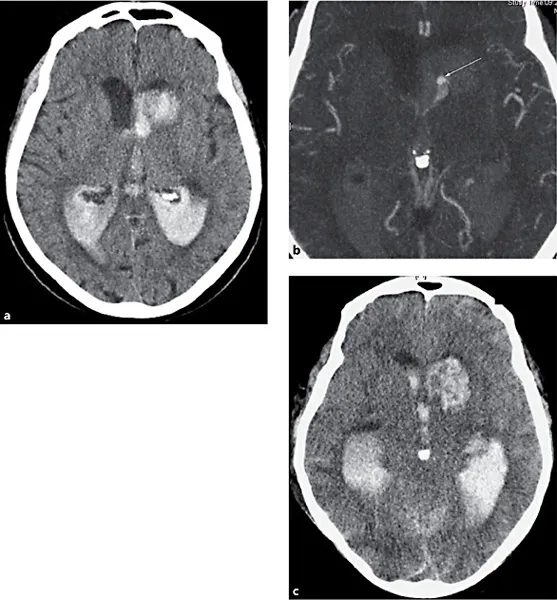
Fig. 1. A computed tomography scan demonstrates a left caudate hemorrhage with extension into the ventricles (a) and the spot sign (see arrow) on the source images of the angiogram (b). On follow-up imaging after 24 h, the caudate hemorrhage had doubled in size, and the amount of ventricular hemorrhage had increased as well (c).
Patients with hematoma expansion were found to have an increased frequency of neurological deterioration (66 vs. 14%) and higher ICH-related mortality rates (29% vs. 3%) compared with those without expansion [13, 15, 26]. For every 1 ml increase in the baseline ICH volume, the hazard ratio of dying increased by 1% [18]. For every 10% increase in the ICH volume at 24 h, the patients were 16% more likely to exhibit a one-point increase on the modified Rankin scale (mRS) for outcomes and 18% more likely to worsen from independence to assisted independence or from assisted independence to a poor outcome [18]. Ultra-early hematoma growth, defined as the relationship between the baseline ICH volume and an ICH onset-to-imaging-time >10.2 ml/h, represents the most powerful predictor of hematoma growth, neurological deterioration, a poor long-term outcome, and mortality [27]. Therefore, it seems reasonable that therapy directed at stopping bleeding as early as possible could potentially decrease mortality and improve functional neurological outcomes. The most interesting questions that remain are as follows: Which type of hemorrhage will expand further after first presentation? Which therapeutic agent is most effective in stopping the bleeding, outweighing all risks associated with its administration?
Table 1. Risk factors for hematoma growth
1. | Shorter time from symptom onset to first CT [12, 15, 21, 26, 38, 51, 62, 133] |
2. | Large hematoma size [30, 51, 62, 133]; hematoma volume on first CT<25 mm3 [26] |
3. | Irregular hematoma shape and heterogeneous lesions [12, 134] |
4. | MAP >120 mm Hg [30]; SBP ≥200 mm Hg [26]; highest SBP [135, 136]; history of hypertension [38] |
5. | GCS score ≤8 [30]; presence of consciousness disturbance [12]; higher NIHSS score [21] |
6. | History of cerebral infarction [26] |
7. | Liver disease [26] |
8. | Fasting plasma glucose ≥141 mg/dl and hemoglobin A1c ≥5.1% [26]; hyperglycemia [62, 133, 137] |
9. | Hypocholesterolemia [137] or hypercholesteremia [133] |
10. | Alcohol consumption (46.3 g/day) [12] |
11. | Reduced fibrinogen level (<87 mg/dl) [12]; elevated serum fibrinogen level (>523 mg/dl) [135] |
12. | Body temperature >37.5°C [135] |
13. | Neutrophil count (by 1,000-unit increase) [135] |
14. | IVH [135] |
15. | Admission cellular fibronectin level >6 μg/ml and admission interleukin-6 level >24 pg/ml [138] |
16. | Oral anticoagulation [15, 21, 23, 38, 51]; increased INR 2 h after presentation [22]; INR >2 before treatment or ≥24 h after PCC administration [24] |
17. | Use of antithrombotic agents prior to hemorrhage [21, 133] |
18. | Baseline weight [133] |
19. | Increased serum creatinine [133] |
20. | White-matter hyperintensities on MRI [139] |
CT = Computed tomography; MAP = mean arterial blood pressure; SBP = systolic blood pressure; GCS = Glasgow Coma Scale; NIHSS = National Institutes of Health Stroke Scale; IVH = intraventricular hemorrhage; INR = international normalized ratio; PCC = prothrombin complex concentrate; MRI = magnetic resonance imaging. | |
Prediction of Intracerebral Hemorrhage Growth: The Spot Sign
Contrast-enhanced imaging studies may indicate an active bleeding process during the acute phase of ICH. Leakage of contrast dye during cerebral angiography was reported in 12.5-42% of patients whose initial CT scan was taken within 5 h of ICH onset [28, 29]. CT angiography (CTA) performed within 12 h of onset showed contrast extravasation in 46% of 113 patients [30]. The patients with contrast leakage were more likely to have been imaged earlier and were significantly more likely to die (64 vs. 16%) [30]. A gadolinium-enhanced ma...
Table of contents
- Cover Page
- Front Matter
- Epidemiology of Intracerebral Haemorrhage
- Emergency Imaging of Intracerebral Haemorrhage
- Evidence-Based Critical Care of Intracerebral Hemorrhage: An Overview
- New Insights into Blood Pressure Control for Intracerebral Haemorrhage
- Emergency Reversal Strategies for Anticoagulation and Platelet Disorders
- Reperfusion-Related Intracerebral Hemorrhage
- Cerebral Microbleeds: Detection, Associations and Clinical Implications
- New Insights into Nonvitamin K Antagonist Oral Anticoagulants’ Reversal of Intracerebral Hemorrhage
- Ultra-Early Hemostatic Therapy for Intracerebral Hemorrhage: Future Directions
- Ventriculostomy and Lytic Therapy for Intracerebral Hemorrhage
- Surgical Craniotomy for Intracerebral Haemorrhage
- New Insights in Minimally Invasive Surgery for Intracerebral Hemorrhage
- Surgical Strategies for Acutely Ruptured Arteriovenous Malformations
- Prognosis and Outcome of Intracerebral Haemorrhage
- Author Index
- Subject Index