eBook - ePub
Intracranial Atherosclerosis: Pathophysiology, Diagnosis and Treatment
- 226 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Intracranial Atherosclerosis: Pathophysiology, Diagnosis and Treatment
About this book
Intracranial atherosclerosis is a leading cause of stroke in Asians and Africans. As these ethnic groups account for more than 70% of the world's population, it is in fact the major cause of ischemic stroke worldwide. This timely book provides readers with up-to-date knowledge of intracranial atherosclerosis, covering vascular anatomy, pathology, epidemiology, stroke mechanisms and syndromes, diagnostic methods as well as treatment strategies such as antithrombotics, angioplasty/stenting and surgery. Furthermore, nonatherosclerotic intracranial arterial diseases like Moyamoya disease, dissection, vasculitis and other miscellaneous disorders are extensively discussed. Experts from both East and West present the latest findings from cutting-edge research and discuss controversial topics from different yet balanced points of view, allowing readers to form their own unbiased opinion on these issues. With this approach, the book serves as a useful and stimulating guide on the diagnosis and management of intracranial atherosclerosis for neurologists, neurosurgeons, neuroradiologists and vascular interventionists.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Intracranial Atherosclerosis: Pathophysiology, Diagnosis and Treatment by J. S. Kim,L. R. Caplan,K. S. Wong,J.S., Kim,L.R., Caplan,K.S., Wong, Julien Bogousslavsky in PDF and/or ePUB format, as well as other popular books in Medicine & Cardiology. We have over one million books available in our catalogue for you to explore.
Information
Kim JS, Caplan LR, Wong KS (eds): Intracranial Atherosclerosis: Pathophysiology, Diagnosis and Treatment.
Front Neurol Neurosci. Basel, Karger, 2016, vol 40, pp 179-203 (DOI: 10.1159/000448313)
Front Neurol Neurosci. Basel, Karger, 2016, vol 40, pp 179-203 (DOI: 10.1159/000448313)
______________________
Non-Atherosclerotic Intracranial Arterial Diseases
Jong S. Kima · Louis R. Caplanb
aDepartment of Neurology, Asan Medical Center, University of Ulsan, Seoul, Republic of Korea; bDepartment of Neurology, Beth Israel Deaconess Medical Center, Boston, Mass., USA
______________________
Abstract
Atherosclerosis is not the only cause of intracranial arterial disease. Arterial dissection, moyamoya disease, vascular inflammatory disease, vasospasm and immunologic disorders are important non-atherosclerotic intracranial arterial diseases. Identification of the correct etiology is important in establishing treatment strategies and assessing prognosis. Careful history taking and appropriate laboratory testing are essential. Although catheter angiography is the most important diagnostic tool to examine various intracranial arterial diseases, other diagnostic modalities such as CT angiography and MR angiography are nowadays widely used. High resolution vessel wall MRI also can assist in making the correct diagnosis as this can yield information regarding vessel wall pathology. Certain diseases such as infectious vasculopathies and moyamoya disease are more prevalent in certain parts of the world, and physicians practicing in these regions should be mindful of these disorders. In this chapter, these non-atherosclerotic intracranial arterial diseases are discussed. Moyamoya disease will be described in another chapter.
© 2016 S. Karger AG, Basel
Arterial Dissection
Cervicocerebral artery dissections account for 1-2% of all ischemic strokes [1-3], and 10-25% of ischemic strokes in young and middle-aged patients [4, 5]. According to population-based studies, the incidence of spontaneous arterial dissections was 1.7-3.0/100,000 in the internal carotid arteries (ICAs) and was 1.0-1.5/100,000 in the vertebral arteries (VAs) [1, 6, 7]. The prevalence is higher in men than in women [8, 9], and females are younger and more often have migraine and multiple dissections [8].
Cervicocerebral artery dissections can result from either primary intimal tear with secondary dissection into the media layer or primary intramedial hemorrhage. The intramural hematoma is located within the medial layer or near the intimal or adventitial layer. A subintimal dissection leads to luminal stenosis and obstruction, resulting in an ischemic event. A subadventitial dissection may cause aneurysmal formation (dissecting aneurysm) and, when intracranial, may cause subarachnoid hemorrhage (SAH).
Dissections are categorized as traumatic or spontaneous (non-traumatic). In patients with spontaneous dissections, minor trauma in the form of stretching of the neck still plays a causative role. Inherent conditions predisposing to spontaneous arterial dissections include fibromuscular dysplasia, cystic medial necrosis, α1 antitrypsin deficiency, Ehlers-Danlos syndrome type IV, Loeys-Dietz syndrome, Marfan's syndrome, autosomal dominant polycystic kidney disease, tuberous sclerosis, migraine, and hyperhomocysteinemia [3, 10]. Ultrastructural morphological aberrations of dermal connective tissue were found in more than half of patients with spontaneous cervical artery dissections [11].
Intracranial Arterial Dissection
Intracranial arterial dissections are known to be less frequent than extracranial dissections. In a retrospective analysis of 263 patients with spontaneous cervicocerebral artery dissections at the Mayo Clinic between 1970 and 1991, 33 (12.5%) had intracranial dissections [3]. Another study showed that among 67 patients with cervicocerebral artery dissections, 9 (13.4%) had intracranial dissections [12]. In a study including a series of 169 patients with 195 VA dissections, 21 dissections (11%) occurred intracranially [8].
The frequency of intracranial dissections may have been underestimated because the diagnosis of intracranial dissection is more difficult than that of the extracranial counterpart. Extensive evaluation, such as repeated MRA in suspected patients [13], and utilization of high resolution vessel wall MRI, that can identify dissection, flap, or mural hematoma more easily [14], will increase the likelihood of diagnosis of intracranial dissection [15]. With advanced imaging, a recent study on dissections causing ischemic stroke or transient ischemic attack (TIA) reported that intracranial arterial dissection is two times more common than extracranial arterial dissection [15]. The most frequent site was the intracranial VA (ICVA).
In contrast to the cervical arteries, the intracranial arteries lack external elastic lamina and have only a thin adventitial layer. Intracranial dissections more readily lead to the development of subadventitial dissections and dissecting aneurysm formation and SAH [16, 17]. Pathological studies have shown that subadventitial dissections are more frequent in the ICVA than in the middle cerebral artery (MCA) [18, 19]. This could explain the relatively high frequency of SAH in ICVA dissections as compared to dissections occurring in the MCA. Trauma, either serious or minor is more closely associated with extracranial dissections than intracranial dissections [3, 15, 17]. Extracranial vessels may be more susceptible to compression against bony structures after trauma, such as that caused by neck rotation. As in atherothrombotic infarction, extracranial dissection usually cause stroke or TIA via artery to artery embolism, whereas branch occlusion is an important stroke mechanism in intracranial dissections. Intracranial dissection frequently causes deep (subcortical and brainstem) infarction [20].
Clinical Manifestations
Dissection in the Anterior Circulation
In the anterior circulation, dissections most often occur in the supraclinoid ICA or the proximal MCA. Distal ICA dissection occasionally extends to the MCA (fig. 1). In a recent series, MCA dissection (19%) was the more prevalent than distal ICA dissection (12%) as a cause of ischemic stroke. In a review of 54 patients with MCA dissections who had 59, most presented with cerebral infarction (91%), while SAH was uncommon (9%) [21]. Most patients showed vascular luminal stenosis (87%), and a small number of patients had aneurysmal dilatation (11%) or a double lumen (2%). Hemiparesis was the most frequent presenting symptom (92%), followed by headache (61%) and consciousness change (44%). Preceding trauma was more often found in isolated MCA dissections than intracranial ICA-MCA dissections (35 vs. 19%). The exact mechanism of how a blunt head injury causes MCA dissection is not clear. One proffered suggestion is that the impact of the MCA against the sphenoid ridge causes an intimal tear, which results in dissection [22]. In contrast, congenital vessel wall defects were found more often in intracranial ICA-MCA dissections than in isolated MCA dissections (26 vs. 4%) [21].
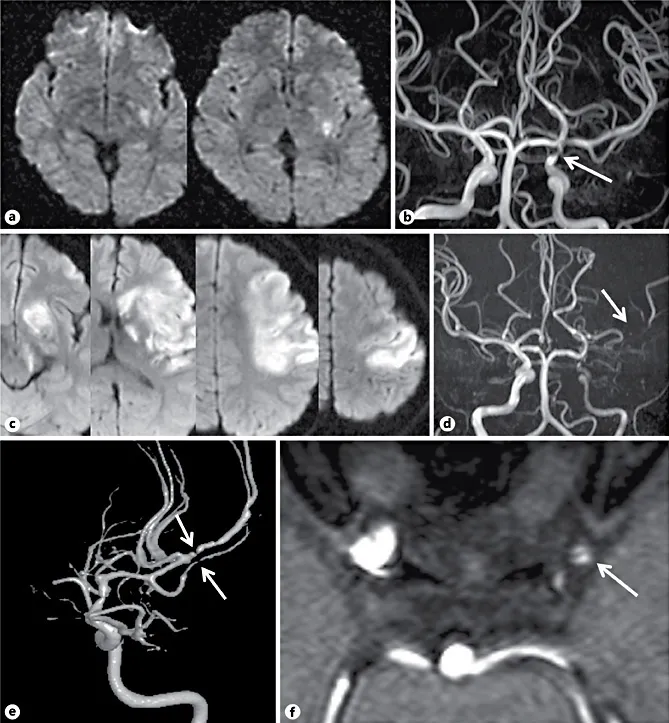
Fig. 1. A 26-year-old woman developed mild (IV/V) right limb weakness. Diffusion weighted MRI (DWI) showed an acute, focal, left basal ganglia infarction (a). MR angiogram showed focal stenosis in the left terminal internal carotid artery (ICA) (b, arrow). Three days later, she developed aphasia and her limb weakness progressed to grade I/V. Follow-up DWI showed extension of the infarction that involved most of the left middle cerebral artery (MCA) territory (c). MR angiogram showed more severe ICA stenosis and poor visualization of the left MCA (d, arrow). 3D reconstruction of conventional angiography showed severe stenosis in the left distal ICA, and diffuse narrowing of the M1 portion of the MCA, which suggests extension of the dissection. Multiple stenoses of the M2 portion of the MCA suggest embolic occlusion (e, arrows). Source image of three-dimensional time-of-flight (TOF) MR angiography showed a flap like structure inside the distal ICA and proximal MCA (f, arrow).
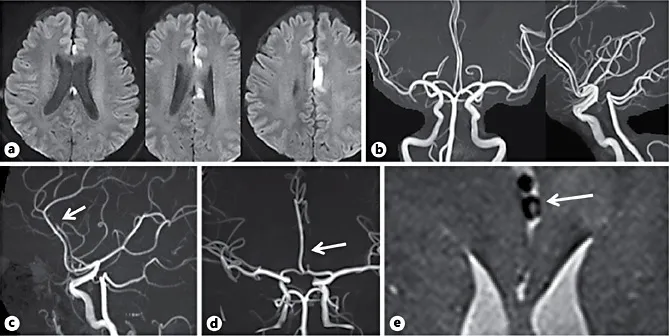
Fig. 2. A 54-year-old man without vascular risk factors developed slight (IV/V) right leg weakness. Diffusion weighted MRI showed left anterior cerebral artery (ACA) territory infarction (a). MR angiography findings were normal (b). After admission, the leg weakness worsened progressively (II/V). Four days later, ...
Table of contents
- Cover Page
- Front Matter
- Intracranial Arteries - Anatomy and Collaterals
- Pathological Characteristics
- Epidemiology
- Risk Factors
- Stroke Mechanisms
- Clinical Stroke Syndromes
- Biomarkers, Natural Course and Prognosis
- Vessel and Vessel Wall Imaging
- Transcranial Doppler
- Antithrombotic Therapy
- Angioplasty and Stenting
- Surgical Therapy
- Non-Atherosclerotic Intracranial Arterial Diseases
- Moyamoya Disease
- Author Index
- Subject Index
- Back Cover Page