eBook - ePub
Sleep-Related Breathing Disorders
- 160 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Sleep-Related Breathing Disorders
About this book
Many sleep-related breathing disorders (SRBD), especially obstructive sleep apnea, originate from upper airway abnormalities. The connection to cardio- and cerebrovascular comorbidities is significant and the impact on the general health of patients is noteworthy. In recent years, important advances have been made in the research, diagnosis, and treatment of SRBD due to a multidisciplinary approach. This volume incorporates contributions in which the efforts and expertise of more than thirty outstanding experts are shared. It provides a concise, practical, and comprehensive review of sleep medicine and will enable researchers and physicians to stay updated on the latest developments.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Sleep-Related Breathing Disorders by H. -C. Lin,H.-C., Lin, Patrick J. Bradley,Patrick J., Bradley in PDF and/or ePUB format, as well as other popular books in Medicine & Neurology. We have over one million books available in our catalogue for you to explore.
Information
Lin H-C (ed): Sleep-Related Breathing Disorders. Adv Otorhinolaryngol. Basel, Karger, 2017, vol 80, pp 125–135
DOI: 10.1159/000470882
DOI: 10.1159/000470882
______________________
Robotic Obstructive Sleep Apnea Surgery
Song Tar Toha–d · Pon Poh Hsub–g
aSingapore General Hospital, bSingHealth Duke-NUS Sleep Centre, cDuke-NUS Medical School, dSchool of Medicine, National University of Singapore, eDepartment of Otolaryngology, Head and Neck Surgery and fENT Specialist Clinic, Changi General Hospital, and gSingapore University of Technology and Design, Singapore, Singapore
______________________
Abstract
Since the first report of the use of the da Vinci robotic system (Intuitive Surgical, Sunnyvale, CA, USA) in transoral robotic tongue base reduction for obstructive sleep apnea (OSA) was published in 2010, this surgical tool and technique has been used worldwide for the resection of tongue base tissue in the multilevel surgical treatment of OSA. The combined knowledge of the published literature on its use has enlightened sleep surgeons worldwide on this new yet evolving surgical tool. Here we will discuss the use of the da Vinci robotic system in the treatment of OSA, the pertinent surgical anatomy for a safe surgical procedure, the primary and secondary outcomes to expect in the multilevel and primary use of this technology in treating the tongue base, the predictors for success or failure, and the complications associated with this technique. We will also compare this technology with other existing techniques for treating OSA and look to the future for other similar technologies in this application.
© 2017 S. Karger AG, Basel
Obstructive sleep apnea (OSA) is a multifactorial and complex disease associated with repeated upper airway collapse during sleep, resulting in oxygen desaturations, frequent arousals, and sleep fragmentation. Untreated OSA has been shown to have significant adverse effects on cardiovascular, cerebrovascular, metabolic, and neurocognitive functions, and contribute to poor quality of life and an increased risk of death [1–4].
Positive airway pressure (PAP) is the gold standard for treating OSA. However, PAP therapy is frequently limited by poor long-term compliance and adherence, and patients often do not want to use it [5, 6]. Surgical treatment can then be offered as an option.
Palatal surgery alone is ineffective in normalizing the apnea-hypopnea index (AHI) [7, 8]. Considering that OSA is characterized by multilevel airway collapse, multilevel surgery yields better outcomes [9].
Studies using drug-induced sleep endoscopy in the preoperative assessment of the upper airway showed that the base of the tongue and supraglottic regions are key sites of obstruction in a significant proportion of patients [10, 11]. The aim of hypopharyngeal OSA surgery is to widen the retroglossal and hypopharyngeal airway space.
Over the years, many tongue base procedures have been reported, including volumetric tongue base reduction procedures using extensive transcervical approaches to the tongue base area, radiofrequency reduction, midline glossectomy, lingual plasty, and submucosal minimally invasive lingual excision (SMILE), as well as procedures that increase tension on the genioglossal and geniohyoid muscles (genial tubercle advancements and hyoid suspension). Unfortunately, consistency in the results was lacking and “risk to lingual artery and hypoglossal nerve prevented more aggressive tongue reduction techniques” [12].
Transoral robotic surgery (TORS) was first described by O’Malley et al. [13] in 2006 to treat upper aerodigestive tract neoplasms. In 2010, Vicini et al. [14] published their preliminary report on TORS for volumetric reduction of the tongue base in their multilevel surgical management strategy for treating OSA. This pilot clinical and cadaveric anatomical study led to widespread use of this new application.
The da Vinci robotic system (Intuitive Surgical, Sunnyvale, CA, USA), with the angled scope and EndoWrist® technology, allowed the surgeon to work around the angled corner in the small oropharyngeal cavity while maintaining agility and visibility of the surgical area, thus allowing precise excision of the obstructing tongue tissue. Here, we will review the current indications and contraindications, surgical anatomy of the lingual vasculature, surgical setup and techniques, and results and complications using TORS for tongue base reduction in the multilevel surgical treatment strategy for treating OSA.
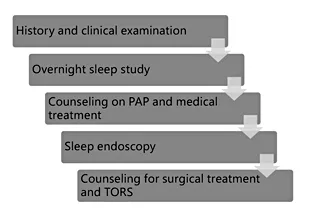
Fig. 1. Stepwise approach in the selection and counseling of patients for surgical treatment of obstructive sleep apnea and for TORS. PAP, positive airway pressure; TORS, transoral robotic surgery.
Assessment
Patients who have failed medical and PAP treatment for OSA with demonstrated tongue base obstruction during sleep endoscopy can be offered transoral robotic tongue base reduction. A stepwise approach (Fig. 1) starting with the patient history, clinical examination, sleep endoscopy, and counseling on options and results is required. The indications and contraindications for surgical treatment and TORS are listed in Table 1. Inadequate mouth opening and trismus is a contraindication for TORS.
Surgical Anatomy
Before conducting this surgical procedure, it is imperative to understand the anatomy of the lingual neurovascular bundle. The area of concern is the deep lingual artery, which is the terminal branch of the lingual artery. The average distance between the 2 deep lingual arteries in the substance of the tongue at the foramen caecum is 27.78 ± 6.57 mm, and the distance to the surface of the tongue is 29.27 ± 5.39 mm [15].
Table 1. Indications and contraindications for transoral robotic surgery
Indications | Contraindications |
Base of tongue obstruction | Severe cardiopulmonary diseases |
Lingual tonsillar enlargement | Uncontrolled psychiatric diseases |
Epiglottic collapse | Unrealistic expectations |
Supraglottic obstruction | Trismus |
Adequate mouth opening |
Table 2. Equipment needed for transoral robotic surgery
da Vinci S/Si/Xi surgical system (surgeon console, patient cart, and vision cart) 30° robotic lens (12 mm, 8.5 mm) Maryland EndoWrist dissector (5 mm) Monopolar EndoWrist cautery (5 mm) Tonsillectomy set with Crow Davis mouth gag and Davis Meyer blade (assorted sizes) Laryngoforce vascular clip, applicator and clip Endolaryngeal microsurgery black sucker Silverglide bipolar forceps | Camera port, 5-mm cannula x2 Antifog solution Tracheostomy set (standby) FK-WO TORS retractor set (standby) |
The safe area for resection between the 2 deep lingual arteries at the tongue base is about 31 mm wide with the tongue in a resting position [16]. However, these distances change as the tongue is protruded out of the oral cavity and with compression with the tongue retraction blade. With the tongue pulled out in the extended/protruded position, the depth of the deep lingual artery on the tongue dorsum becomes less and the interarterial distance is narrowed compared to the resting position at the foramen caecum and 1 cm before and 1 cm after the foramen caecum. The deep lingual artery is brought closer to the tongue surface at these 3 points (from about 28 to 24–25 mm) and closer together (from about 20 to 14 mm) at the foramen caecum [17]. The TORS robotic surgeon should bear in mind the changes in the anatomy of the 2 lingual arteries and changes in the safety margin during surgery for adequate resection.
The dorsal lingual branches arising from the main lingual artery supply the mucosal of the dorsum of the tongue. These vessels generally do not cause troublesome bleeding and can be easily hemostased with bipolar diathermy or suction diathermy.
Surgical Equipment and Setup
The robotic and general equipment needed is listed in Table 2. The configuration of the surgical bed, robotic cart, surgeon’s console, vision cart for the assisting surgeon to view the operation, and position of the assisting surgeon at the head of the table is shown in Figure 2. The da Vinci Robotic system is placed at about 30–45° to the long axis of the patient’s bed. The anesthetic machine and anesthetist is on the left of the patient and should not obstruct the view of the assisting surgeon. The final position with the robotic arm, camera, and gag in situ is shown in Figure 2.
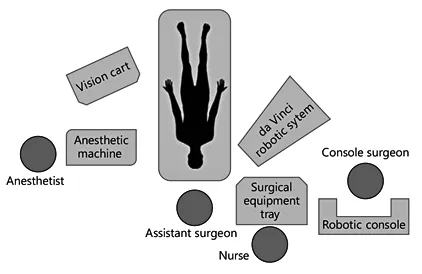
Fig. 2. Operating room setup for transoral robotic surgery using the da Vinci system.
Surgical Technique
Robotic tongue base reduction is performed as a component of multilevel surgery treatment in conjunction with other upper airway modification surgery (nasal, palatal, and pharyngeal) in the same setting. The technique, as first...
Table of contents
- Cover Page
- Front Matter
- A Succinct History of Sleep Medicine
- Advanced Concepts in the Pathophysiology of Obstructive Sleep Apnea
- The History of Sleep Surgery
- Advances in the Diagnosis of Obstructive Sleep Apnea: Drug-Induced Sleep Endoscopy
- Novel Positional Devices for the Treatment of Positional Obstructive Sleep Apnea, and How This Relates to Sleep Surgery
- Updated Concepts on Treatment Outcomes for Obstructive Sleep Apnea
- Updated Friedman Staging System for Obstructive Sleep Apnea
- Advancements of CPAP Therapy for Obstructive Sleep Apnea
- Advances in Oral Appliances for Obstructive Sleep Apnea
- Updated Nasal Surgery for Obstructive Sleep Apnea
- Updated Palate Surgery for Obstructive Sleep Apnea
- Updated Hypopharyngeal Surgery for Sleep Apnea
- Updated Minimally Invasive Surgery for Sleep-Related Breathing Disorders
- Advances in Box Surgery for Obstructive Sleep Apnea: Genioglossus Advancement, Hyoid Suspension, and Maxillomandibular Advancement
- Multilevel Obstructive Sleep Apnea Surgery
- Innovative Surgery for Obstructive Sleep Apnea: Nerve Stimulator
- Robotic Obstructive Sleep Apnea Surgery
- Pediatric Obstructive Sleep Apnea: Where Do We Stand?
- Future Perspectives in Sleep Medicine
- Future Perspectives in Sleep Surgery
- Author Index
- Subject Index
- Back Cover Page