eBook - ePub
The Diabetic Foot Syndrome
- 224 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
The Diabetic Foot Syndrome
About this book
In recent years, "diabetic foot" has become the common name given to chronic complications of diabetes mellitus in the lower limb. This book provides an up-to-date picture of the clinical scenario, the latest understanding of the mechanisms in regard to pathology, the current standards of therapy, and the organizational tasks that a modern approach to such a complex pathology warrants. All contributors have delivered articles that are as informative and straight-to-the point as possible, including not only their own experience in the field, but also giving a wider picture to link each article to the other. The Diabetic Foot Syndrome is not only relevant to specialists, but also to all the caregivers involved in the management of the patients at risk for developing the pathology, those affected, and those who are at risk of recurrences.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access The Diabetic Foot Syndrome by A. Piaggesi,J. Apelqvist,A., Piaggesi,J., Apelqvist, Massimo Porta,Massimo, Porta in PDF and/or ePUB format, as well as other popular books in Medicine & Cardiology. We have over one million books available in our catalogue for you to explore.
Information
Piaggesi A, Apelqvist J (eds): The Diabetic Foot Syndrome.
Front Diabetes. Basel, Karger, 2018, vol 26, pp 107–130 (DOI: 10.1159/000480057)
Front Diabetes. Basel, Karger, 2018, vol 26, pp 107–130 (DOI: 10.1159/000480057)
______________________
Surgical Management of the Charcot Foot
Luca Dalla Paola · Giuseppe Scavone · Anna Carone · Lucian Vasilache · Giulio Boscarino
Diabetic Foot Unit, Maria Cecilia Hospital, GVM Care and Research, Cotignola, Italy
______________________
Abstract
Charcot neuropathic osteoarthropathy is a severe complication of diabetic neuropathy. Even today the disease is difficult to recognize and treat. While in the early stages conservative therapy is extremely efficient and avoids progression into more advanced phases, when there are structural deformities and osteoarticular alterations, surgery often takes on the role of limb salvage therapy. Within this scenario, we take into consideration the physiopathology and anatomical/functional conditions that support the indication for surgery. In this paper, we review the surgical techniques, both in the field of reconstructive and prophylactic surgery aiming at correcting deformity and instability before ulcerative lesions onset, and in the field of emergent surgery once there is a complicated condition due to osteomyelitis in the bone structures.
© 2018 S. Karger AG, Basel
Introduction
Charcot neuropathic osteoarthropathy (CN) involving the foot and/or the ankle is a challenging clinical condition that causes progressive bone deformity and osteoarticular instability, which leads to ulcerations, spread of infection and, consequently, an elevated risk of amputation [1–7]. CN does not only entail a high risk of losing the limb; this condition is also linked to a reduction in the quality of life, high disability and increased risk of mortality [8–15].
Even if J.M. Charcot gave the first detailed description of the clinical aspect of the disease in 1868, CN is a pathological process still difficult to recognize and treat. As diabetes exponentially increases worldwide, all the health professionals need to be aware of its possible limb-threatening progression [16–19].
It is also important to notice how progression – from neuropathy to structural deformity – also involves transitional stages, and during the early phases it becomes possible to efficiently treat the condition, thereby preventing progression. The earlier CN is diagnosed and treated (total off-loading), the lesser the risk to develop deformity and articular instability that can lead to ulceration, osteomyelitis and, thus, amputation.
Fifty years ago, Eichenholtz [20] defined for the first time (in a landmark paper based on clinical examination and radiographic findings) the 3 independent but linear stages of CN: development, coalescent and reconstructive. The system proposed by Eichenholtz was modified by Shibata et al. [21] adding a stage prior to that of development characterized by lack of injury or osteoarticular disorders.
Chantelau has recently proposed a new CN classification based on magnetic resonance imaging (MRI) [22]. Stage A includes the acute or active phase, while stage B refers to the quiescent phase. These are differentiated by the presence or absence of bone marrow oedema on MRI. Each stage presents different numerical gradings (grade 0 is characterized by the absence of cortical fractures; grade 1 by the presence of cortical fractures). The stage influences decisions on treatment, while grading regards functionality, orthotic aid possibilities and prognosis. Each of the 4 categories clinically differs from each other in terms of histopathology and radiological imaging. It is extremely important to recognize the different stages of progression in order to effectively choose a treatment strategy. Indeed, the approach may vary according to the different stages of the natural history of the CN.
It is presently not possible to predict the onset of this complex pathology in diabetic patients with peripheral neuropathy. Yet, it is possible to diagnose early and detect the first clinical signs and symptoms. Recognizing the condition in its early stages, when there is no anatomic alteration yet, would allow the possibitly to opt for a conservative approach, avoiding deformity and osteoarticular instability stages that translate into the risk for amputation.
Early diagnosis of CN is based both on patient’s history and on clinical data. Any time a neuropathic patient presents a red, hot, swollen foot, we are led to thinking about an acute stage CN. The diagnosis is then confirmed once we get to know the patient’s history. The careful and accurate analysis of the medical history will enhance the diagnostic hypothesis and, in particular, will allow the opportunity to make a differential diagnosis as compared to other conditions (e.g., gout, arthritis, algodistrophy, osteomyelitis), which may show similar clinical and instrumental (radiological) findings.
The localization of the undermining anatomical-structural condition is equally important to define and predict the magnitude of the deformity and assess the need for corrective surgery.
In CN, Frykberg and Sanders [4–6] identified 5 patterns of damage in the foot and ankle and associated these different anatomical patterns (Fig. 1).
The location at Lisfranc and at the ankle/subtalar joints are the locations where the most severe structural deformity and instability are found. The pattern V is rare but may be correlated with an avulsion injury or isolated pathologic fracture of the posterior calcaneal tuberosity.
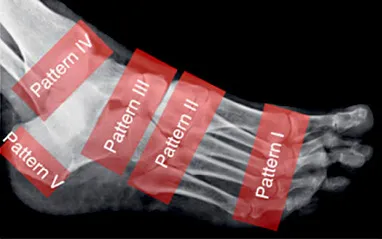
Fig. 1. Frykberg and Sanders anatomical classification of CN.
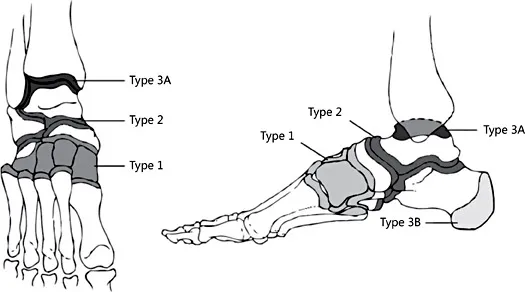
Fig. 2. Brodsky anatomical classification of CN.
Based on the 4 regions most commonly affected by CN, an anatomical classification is described also by Brodsky and Rouse (Fig. 2) [23].
This classification was further differentiated into a supplementary number of classes as of the elevated percentage of involvement of the midfoot and of the medial column [24–r26].
Acquired deformities are often complicated by large wounds that develop alongside bone deformities, and the progression of infection to osteomyelitis is frequent, with an increased risk of major amputation (Fig. 3) [12, 19, 23–29].
Bevan and Tomlinson [30] found (studying the radiographic images in weight-bearing conditions) that patients are at low risk of developing ulcerations or infections if their feet are radiographically consistently plantigrade. They observed that the risk of developing a wound was reduced if the axis of the hindfoot was reasonably collinear with the axis of the forefoot.

Fig. 3. Charcot foot complicated by plantar ulceration.
In CN, the degree of instability and deformity correlates with the risk of developing an ulcer and it must be considered the primary risk factor for amputation [13]. In these terms, the most proximal the deformity and instability is, the highest is the risk of wound onset. In the case of ankle involvement, the surgical approach should be carried out as soon as possible even before the onset of an ulcer [13, 25, 31–35].
The existence of a foot ulcer may require further investigations and treatment, including hospitalization, non-weight-bearing, specific antibiotic regimen and diagnostic imaging such as MRI or bone scans. The presence of a wound becomes the primary indication for surgical treatment of CN because it compromises the limb functionality, causing a high-risk of spreading infection through soft tissue and osteomyelitis [13].
Indications for Surgical Approach
Surgical treatment of Charcot neuroarthropathy is an extremely important chapter of the whole surgical approach to the diabetic foot. Actually, the Charcot foot surgery also embraces all the distinct classes of surgery described in the classification published by Armstrong and Frykberg (Table 1) [36].
Table 1. Classes of diabetic foot surgery
Diabetic foot surgery class | Description | Potential risk for high level amputation |
Class IV: emergent | Procedure performed to limit progression of acute infection | High |
Class III: curative | Procedure performed to assist in healing open wound | Moderate |
Class II: prophilactic | Procedure performed to reduce risk of ulceration or reulceration in person with loss of protective sensation but without open wound | Low |
Class I: elective | Procedure performed to alleviate pain or limitation of motion in a person without loss of protective sensation | Very low |
The ideal and stan...
Table of contents
- Cover Page
- Front Matter
- The Diabetic Foot Syndrome Today: A Pandemic Uprise
- A Complication of the Complications: The Complexity of Pathogenesis and the Role of Co-Morbidities in the Diabetic Foot Syndrome
- Re-Evaluating the Outcomes in Diabetic Foot Management
- The Charcot Foot Revisited: How the New Pathogenetic Findings Explain the Clinical Course of the Disease
- Diabetic Peripheral Arteriopathy: A Tale of Two Diseases
- Does Microangiopathy Contribute to the Pathogenesis of the Diabetic Foot Syndrome?
- The Organization of Care for the Diabetic Foot Syndrome: A Time-Dependent Network
- Offloading the Diabetic Foot: The Evolution of an Integrated Strategy
- Surgical Management of the Charcot Foot
- Indications to Revascularization in the Ischaemic Diabetic Foot
- An Integrated Approach for the Effective Management of Limb-Threatening Ischaemia in the Diabetic Foot
- Resistant Infections in the Diabetic Foot: A Frightening Scenario
- Antibacterial Treatment in Diabetic Foot Infections
- The Role of Surgery in the Management of the Infected Diabetic Foot
- Local Management of Diabetic Foot Ulcers, Dressings and Other Local Treatments
- Towards Extending Ulcer-Free Days in Remission in the Diabetic Foot Syndrome
- Author Index
- Subject Index
- Back Cover Page