- 392 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
About this book
The field of liver transplantation has undergone tremendous change and continues to evolve at a fast pace. This book covers topics beyond standard care and discusses issues that are new and rapidly evolving in the field. These include innovative surgical methods to maximize the donor pool, non-surgical methods to expand the existing pool of additional donors, the changing face of liver rejection, and management of infections in the presence of new antivirals.
This book is an interesting read for surgeons, hepatologists, and healthcare workers looking after patients who need or have had a liver transplant.
Contents:
- Preface
- Liver Transplantation for HCC: Moving Beyond Milan (Amit D Tevar)
- Liver Transplantation for Non-HCC Malignancies: Cholangiocarcinoma, Neuroendocrine Tumors, HEHE, and Colorectal Metastases (Daniel Zamora-Valdes and Julie K Heimbach)
- Developments in Donation After Cardiac Death in Liver Transplantation (David P Foley and David J Reich)
- Machine Preservation of Livers for Transplantation (Paulo Fontes, Arjan van der Plaats, Roberto Lopez, Kyle Soltys, Wallis Marsh, Ruy Cruz, Banan Babak, William R Light, and Christopher Hughes)
- Living Donor Hepatectomy: Laparaoscopic and Robotic Techniques (Salvatore Gruttadauria, Giovanni B Vizzini, Duilio Pagano, Bruno G Gridelli, and Angelo Luca)
- Adult Living-Donor Liver Transplant: Right Lobe (Young-In Yoon and Dong-Sik Kim)
- Adult Living-Donor Liver Transplant: Left Lobe (Hillary J Braun, Garrett R Roll, and John Paul Roberts)
- Pediatric Liver Transplantation with Technical Variant Allografts (Kyle Soltys, Geoff Bond, Rakesh Sindhi, and George Mazariegos)
- ABO-Incompatible Liver Transplant (Abhideep Chaudhary, Prashant Pandey, and Sunil Taneja)
- New Trends in Immunosuppression for Liver Transplantation: Minimization, Avoidance and Withdrawal (Shoko Kimura, Fermin Fontan, and James F Markmann)
- Antibody-Mediation Rejection in Liver Transplantation (James F Trotter)
- Hepatitis C and Liver Transplantation in the Era of New Antiviral Treatments (Elizabeth C Verna and Robert S Brown Jr)
- Obesity in Liver Transplantation (Michele Molinari and Subhashini Ayloo)
- Liver Transplantation for Metabolic Disease (Patrick McKiernan and Kyle Soltys)
- Fulminant Hepatic Failure: Integrating Devices with Liver Transplantation (Nigel Heaton and Shirin Elizabeth Khorsandi)
- Future Directions in Liver Replacement Therapy: Liver Xenotransplantation (Burcin Ekser and David K C Cooper)
Readership: Hepatologists, and surgeons and nurses in hepatology.
Key Features:
- Covers topics that are new and rapidly evolving in liver transplantation
- Written by experts in liver transplantation
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Liver Transplantation by Abhinav Humar, Amit Tevar, Christopher Hughes in PDF and/or ePUB format, as well as other popular books in Medicine & Gastroenterology & Hepatology. We have over one million books available in our catalogue for you to explore.
Information
Topic
MedicineSubtopic
Gastroenterology & Hepatology1.Liver Transplantation for HCC: Moving Beyond Milan
Amit D. Tevar
Division of Transplantation Surgery, University of Pittsburgh, Pittsburgh, PA 15213, USA
1.Introduction
Hepatocellular carcinoma (HCC) remains one of the most common causes of cancer death in the world. The incidence of HCC in regions of the world with endemic hepatitis B and C infection is substantially higher than other areas [1, 2]. Worldwide, the incidence of HCC is the sixth most common diagnosis of cancer and the third cause of cancer death, with the highest incidence rates in Asia and Africa [3]. This is likely a conservative estimate as many HCC diagnosed patients and deaths remain unreported in areas without significant medical infrastructure and reporting mechanisms. There has been a sharp rise in the incidence of HCC in the United States from 1.4/100,000 from 1976 to 1980 to 2.4/100,000 from 1991 to 1995. During this time period, there was also a significant increase in the overall mortality from HCC, with a 41% increase in the mortality rate based on review of the Surveillance, Epidemiology and End Results (SEER) database [4]. More recently in the United States despite a plateau in the overall incidence, there have been further significant increases in the liver cancer mortality from HCC, between 2007 and 2010 (Figure 1). This increase in mortality was found to be localized to African Americans, Hispanics, and white males greater than 50 years of age [5, 6].
Surveillance for HCC has been implemented for cirrhotic and fibrotic patients based on the recommendations of multiple societies. The current guidelines from the American Association of the Study of Liver Diseases (AASLD) suggest that ultrasound examination at an interval of 6 months for screening (Figure 2) [7]. Several studies have demonstrated the utility of a single dynamic imaging modality which demonstrates arterial uptake followed by “washout” in the venous phase to be sensitive for the noninvasive diagnosis of early and late HCC lesions [8, 9].
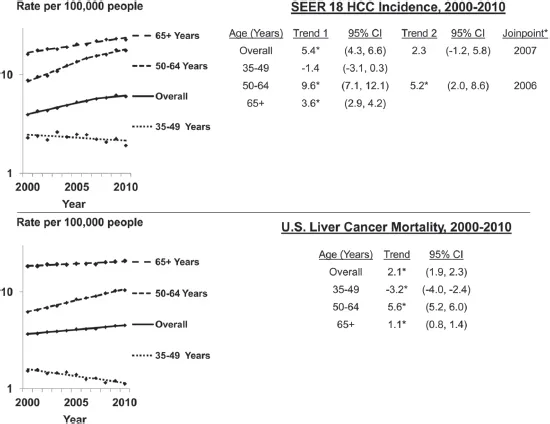
Figure 1.Age-adjusted SEER 18 HCC incidence and United States liver cancer mortality rates by age group and year, 2000–2010. CI: confidence interval; Trend: annual percent change (APC). Joinpoint regression defines when a trend changes. Up to one joinpoint is allowed in the 11-year period. (Reprinted with permission from Ref. [5]. Copyright © 2014 Nature Publishing Group.)
Note: * Slope of trend differs from zero (p < 0.05).
The staging of HCC remains a problematic and complex problem, as the disease progression and patient survival involves and changes with tumor biology, liver disease, and performance status. As a result, multiple staging algorithms have been proposed and attempted to be validated for prognosis of HCC. The first of these was introduced in 1985 as the OKUDA score and combined liver function and tumor parameters as predictor of survival [10]. The Italian Cancer of the Liver Italian Program (CLIP) reviewed 435 patients from 16 center and correlated survival based on liver function (Child–Pugh score) and tumor parameters, including portal vein thrombosis and alpha-fetoprotein (AFP) [11]. The Barcelona Clinic Liver Cancer (BCLC) system was introduced in 1999 and linked liver function, tumor parameters, and performance status into four stages: early, intermediate, advanced, and terminal [12]. The system of classification has been subsequently evaluated and validated in large Western and Asian cohorts with an enrollment of 3,892 Asian patients with HCC [13, 14]. Median survival times were noted to be 57.7 months at very early stage and 1.6 months at terminal stage. The BCLC is currently endorsed by European Associations for the Study of the Liver (EASL) and the AASLD and is used in practice throughout Europe and North America (Figure 3).
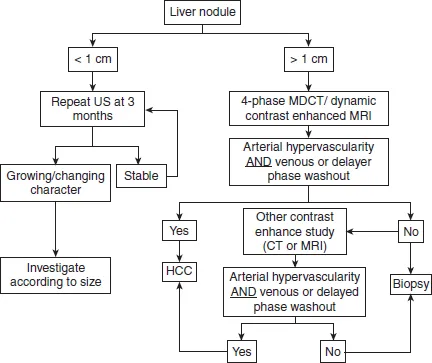
Figure 2.AASLD Practice Guidelines on HCC [7].
Several Asian scoring systems have also demonstrated significant survival prediction in the Asian cohort of patients. The Japan Integrated Staging (JIS) was originally released in 2003 and was based on a cohort of nearly 14,000 Japanese patients. Survival prediction is based on Japanese TNM factors (vascular invasion, number and size of lesions) and liver function (CPT Score) [16]. The survival accuracy was further increased in 2006 with the use of indocyanine green clearance on a review of 42,269 patients [17] and in 2008 included the addition of three separate HCC tumor markers and is now called the biomarker combined JIS (bm-JIS) [18]. Other Asian classification systems include the Hong Kong Liver Cancer (HKLC) classification system, the Taipei Integrated Scoring (TIS) system, the Advance Liver Cancer Prognostic System (ALCPS), the Chinese University Prognostic Index score, and others [19–22].
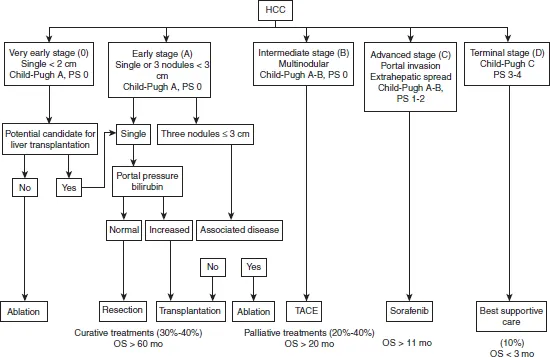
Figure 3.Barcelona Clinic Liver Cancer system. HCC: hepatocellular carcinoma; PS: performance status; TACE: transarterial chemoembolization. (Reprinted with permission from Ref. [15]. Copyright © 2016 The Author(s).)
2.Liver resection and local regional therapy as curative treatment options
Surgical resection as partial hepatectomy or hemihepatectomy is an effective modality of cure of the HCC in patients with noncirrhotic liver disease without evidence of significant portal hypertension. Approximately 80% of cases of HCC are found in patients with overt cirrhosis worldwide [23]. A very small cohort of patients exist in the East and West with noncirrhotic HCC and can be treated very effectively with primary surgical resection. A meta-analysis of all Eastern and Western studies on noncirrhotic HCC patients and lesions found no demographic patient differences but found that tumors were larger, with more microvascular invasion, in noncirrhotic HCC patients and that noncirrhotic HCC patients had more advanced tumor-node-metastasis (TNM) stage disease compared to cirrhotic patients [24]. In addition, it was noted that there were differences in postoperative morbidity (8.3–55.5%) or mortality (0–6.5%) between both groups. There is an obvious degree of selection bias in the cirrhotic population that undergoes resection as the primary treatment of HCC, but the most important difference that is seen between the two groups is in the disease-free survival (DFS). The largest multicenter report comes from the Liver Cancer Study Group from Japan and their cohort of 6,785 patients treated with resection for HCC [25]. Their cohorts’ 1-, 3-, 5-, and 10-year survival rates were noted to be 85, 64, 45 and 21%, respectively. The morbidity and mortality success rate in liver resection (LR) depends on optimizing patient selection and extent of resection to ensure adequate margin and adequate functional liver reserve (FLR) volume after resection. Several studies have demonstrated that adequate FLR be >20% in noncirrhotic livers and >40% in cirrhotics [26–28]. In addition, portal vein embolization is an important tool in the hypertrophy of the remnant liver to ensure adequate volume. A large multicenter study from France, USA, and China reviewing only major (more than segments) LRs for HCC demonstrated 3-, 5-, and 10-year overall survival (OS) of 54, 40, and 27% [29]. Factors predictive of poor long-term survival outcomes included AFP level >1,000 ng/mL, tumor size >5 cm, presence of major vascular invasion, presence of extrahepatic metastases, positive surgical margins, and earlier time period in which the major hepatectomy was performed [29].
Recurrence rates have been demonstrated to be the significant downside to surgical resection as there is an increased risk of de novo or recurrent HCC, in comparison to those patients who undergo liver replacement therapy with liver transplant(ation) (LT). Several scoring systems have been developed to predict the recurrence and OS following LR for HCC. These nomograms include the Singapore Liver Cancer Recurrence (SLICER) Score, the Surgery-Specific Cancer of the Liver Italian Program (SSCLIP) scoring system and the Memorial Sloan Kettering Cancer Center scoring system [30–32]. The scores were constructed to predict the 3- and 5-year DFS and all three identified preoperative AFP, vascular invasion and tumor size and independent predictors of successful long-term disease-free outcome. In these cohorts and other single and multi-institutional reviews, the recurrence rate after surgical resection has ranged widely [24, 33–35]. One of the largest series, collected in a prospective fashion, comes from Poon et al. and demonstrated 1-, 3-, 5- and 10-year DFS rates were 74, 50, 36, and 22% [33]. Predictors of poor recurrence rates were cirrhosis and number of lesions.
Local regional therapy is an interesting and selective effective modality for treatment of HCC. The experience with this modality comes from the patient in which LT or LR is contraindicated, in which case it has demonstrated prolonged OS. Several indications exist for the use of local regional therapy including as a primary treatment of HCC in those with early disease that are not candidates for LR or LT, a downstaging too for those with tumor size too large for successful transplant, and as a bridge therapy for those that may have a prolonged wait for cadaveric or live donor LT. Commonly used tumor ablative modalities include radiofrequency ablation (RFA), microwave ablation (MWA) or cryoablation. RFA is currently the more commonly used modality for ablative local regional therapy for primary HCC treatment, downstaging, and bridge therapy and works by tissue destruction with frictional heat generation from application of alternating current. The limitations of this modality, as it does require sustained heat generation to ensure tumor tissue necrosis with a margin, includes the “heat sink” effect that does occur from high-flow vasculature found within the liver providing for decreased temperature and therefore ineffect...
Table of contents
- Cover Page
- Title
- Copyright
- Preface
- Contents
- 1. Liver Transplantation for HCC: Moving Beyond Milan
- 2. Liver Transplantation for Non-HCC Malignancies: Cholangiocarcinoma, Neuroendocrine Tumors, HEHE, and Colorectal Metastases
- 3. Developments in Donation after Cardiac Death in Liver Transplantation
- 4. Machine Preservation of Livers for Transplantation
- 5. Living-Donor Hepatectomy: Laparoscopic and Robotic Techniques
- 6. Adult Living-Donor Liver Transplantation: Right Lobe
- 7. Adult Living-Donor Liver Transplantation: Left Lobe
- 8. Pediatric Liver Transplantation with Technical Variant Allografts
- 9. ABO-Incompatible Liver Transplantation
- 10. New Trends in Immunosuppression for Liver Transplantation: Minimization, Avoidance, and Withdrawal
- 11. Antibody-Mediated Rejection in Liver Transplantation
- 12. Hepatitis C and Liver Transplantation in the Era of New Antiviral Treatments
- 13. Obesity in Liver Transplantation
- 14. Liver Transplantation for Metabolic Disease
- 15. Fulminant Hepatic Failure: Integrating Devices with Liver Transplantation
- 16. Future Directions in Liver Replacement Therapy: Liver Xenotransplantation
- Index