![]()
Section 1:
Physiologic Considerations
of Newborn/Child
![]()
PEDIATRIC
THERMOREGULATION
AND METABOLISM | 1 |
David E. Carney and Miller C. Hamrick
NEWBORN AND CHILDHOOD PREDISPOSITION TO HEAT LOSS
The human newborn is a homeotherm desiring to maintain a stable core body temperature over a wide range of environmental changes while minimizing metabolic demand. Hypothermia has been found to increase morbidity and mortality in newborns of all gestational ages and birth weights. The range over which a newborn can maintain body temperature is more limited than that of an adult. The newborn has a high surface area to volume ratio, a distinct lack of subcutaneous fat, poor vasomotor response to cold, and a relative inability to produce heat by shivering.1 Therefore, equilibrium is maintained by a delicate balance between heat production and heat loss.
TYPES OF HEAT LOSS
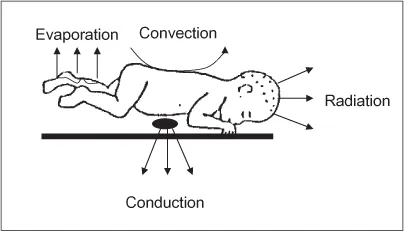
Heat loss between the newborn and the environment occurs via four major mechanisms including conduction, convection, radiation, and evaporation (Figure 1).
Figure 1. Modes of heat loss in infants and children.
A. Conduction: Involves the transfer of heat from the newborn to a cooler object that is in direct contact with the newborn (e.g. uncovered bed, X-ray plate, scales).
B. Convection: Involves heat loss from the infant due to cool air moving across the skin and dependent on air temperature and the amount of skin exposed; can be prevented by the use of isolette or plastic covering.
C. Radiation: Involves direct transfer of heat from an exposed surface of the newborn to surrounding surfaces and is compounded by moisture on the skin; can be prevented by the use of radiant warmer, hats and bundling.
D. Evaporation: Involves insensible water loss from the skin and respiratory mucosa of the newborn as moisture evaporates; prevented by the use of humidified air and bundling.
MAINTAINING CORE TEMPERATURE
The physiologic mechanisms to produce heat include both voluntary and involuntary actions. In the newborn, the most important of these is nonshivering thermogenesis that utilizes brown fat. Brown fat is located around the muscles and blood vessels of the scapulae, neck, axillae, and mediastinum. It has more mitochondria and a richer blood supply than white fat. Once the hypothalamus receives the message that the infant is cold, norepinephrine stimulates receptors in the brown fat causing oxidation of glycerol and fatty acids producing heat. Alternative mechanisms for maintaining body temperature include peripheral vasoconstriction and central shunting. Proper maintenance of temperature prevents peripheral vasoconstriction and allows for more accurate assessment of resuscitation. All of these mechanisms are important especially in the postoperative period to avoid the development of neonatal cold injury syndrome, which manifests as lassitude, apnea, bradycardia, acidosis, hyperglycemia, hyperkalemia, and oliguria. Prolonged hypothermia increases oxygen consumption, caloric demand, and rapidly decreases glycogen stores. Hypothermia is also associated with an increased rate of wound infections and postoperative sepsis.2
The newborn not only has difficulty conserving, but dissipating heat as well. In warm environments, the newborn increases evaporative heat loss by peripheral vasodilatation and sweating, though sweating does not occur in preterm infants. Even so, these mechanisms are often inadequate to prevent a rise in core temperature. Great care must be taken to closely regulate the body temperature of the newborn, with ideal ambient temperature ranging from 35°C (95°F) in preterm and low birth weight infants less than 6 weeks old to 29°C (84°F) for full-term infants heavier than 2–3 kg.
Preventing Heat Loss
Preventing heat loss is of utmost importance, especially in the first 12–24 hrs after birth, as these patients are most at risk for complications related to hypothermia. Multiple factors may predispose certain newborns to difficulties in maintaining normothermia including prematurity and those with CNS problems, sepsis, or prolonged resuscitation at birth. Monitoring of temperature should begin immediately after birth and checked every 4–6 hrs with a goal temperature of 36.7–37.3°C (98–99°F). If the temperature falls out of range, it should be checked every 30 mins until it returns to the target range.3 It is also important to monitor temperature every 1–2 hrs when a newborn undergoes an environment change for procedural purposes (e.g. imaging, exposure for line placement, surgery). Temperature regulation is most important in preterm and low-birth weight infants as their skin is not yet mature and their ability to initiate nonshivering thermogenesis is very limited.4 Also, brown adipose tissue begins to be deposited at 28 weeks gestational age; therefore, extremely premature infants have almost no ability to maintain body temperature. At birth, these high-risk infants should be delivered in a room with ambient temperature > 25°C (77°F) and be covered immediately from the neck down with an occlusive polythene wrapping for transfer to the neonatal ICU.5 Any infant less than 1.5 kg should be placed in an incubator with humidity levels between 50% and 80%. For those infants > 1.5 kg, a radiant warmer should be employed which provides heat by a combination of conduction via a gel mattress and radiation from above.6 This mechanism is also employed for those infants who require ease of access for procedures such as central line placement or lumbar puncture. Once the infant can maintain normothermia in a 26–28°C room, they can be moved to an open bassinette or crib but should always be covered in blankets and wear a hat. Most infants > 4 kg need only bundling and hats to maintain core temperature.
REFERENCES
1. Alden K. (2007) Physiologic and behavioral adaptations of the newborn. In: D Lowdermilk & S Perry (eds.), Maternity & Women’s Health Care, 9th edition, pp. 639–641. Mosby/Elsevier, St. Louis.
2. Sofer S, Bankovich E. (2000) Severe infantile hypothermia: Short and long-term outcome. Intensive Care Med 26(1):88–92.
3. Cheffer N. (2004) Adaptation to extrauterine life and immediate nursing care. In: S Mattson & J Smith (eds.), Core Curriculum for Maternal-Newborn Nursing, 3rd edition, pp. 422–423. Elsevier/Saunders, St. Louis.
4. Sedin G. (2006) Physical environment. Part I: The thermal environment of the newborn infant. In: R Martin, A Fanaroff & M Walsh (eds.), Fanaroff & Martin’s Neonatal-Perinatal Medicine: Diseases of the fetus and infant, 8th edition. Mosby, Philadelphia.
5. Sherman T, Greenspan J, St. Clair N, et al. (2006) Optimizing the neonatal thermal environment. Neonatal Network 25(4):251–260.
6. Williams PR, Oh W. (1974) Effects of radiant warmer on insensible water loss in newborn infants. Am J Dis Child 128:511.
![]()
FLUIDS, RESUSCITATION
AND ELECTROLYTES | 2 |
David E. Carney and Miller C. Hamrick
INTRODUCTION
The discussion of fluids, resuscitation and electrolyte management in infants and children is broad and a comprehensive understanding is well documented elsewhere.1–5 Here we briefly review how the newborn physiology varies from older children and adults and the impact of those differences on resuscitation. We then review the generic theme of maintenance fluid replacement and guiding principles to consider during acute resuscitation. Finally, signs of common electrolyte imbalance and treatment are reviewed.
Multiple factors must be assessed in determining the fluid status and fluid requirements of the pediatric population. Total body water in the fetus slowly decreases over time from 80% of total body weight at 32 weeks gestation, to 78% at term, and 60% by 18 months.6,7 Therefore, the initial duty of the infant kidney is to reduce extracellular fluid volume which begins immediately after birth. This manifests itself as a 4–5% decrease in total body water in the first week of life. Clinically this manifests as a ...