- English
- ePUB (mobile friendly)
- Available on iOS & Android
Pocket Guide to Physical Assessment
About this book
A concise, quick-reference handbook on history taking and physical examination
Pocket Guide to Physical Assessment is a compact yet comprehensive reference for students and practitioners alike, employing a step-by-step framework for effective patient assessment, diagnosis and planning of care.
This valuable guide covers topics including cardiovascular, respiratory, neurological and musculoskeletal system examinations, patient interviews, history taking and general health assessments. Clear diagrams and checklists illustrate key points, while easy-to-follow instructions and concise descriptions of clinical situations and diseases aid in clinical decision-making.
- Compact, pocket-sized guide that contains only the essential information for physical assessment
- Instructs readers on best clinical practice and how to present and communicate cases
- Develops and improves necessary skills for physical clinical examinations
- Ideal for use on the ward or as a companion to the accompanying textbook, Physical Assessment for Nurses and Healthcare Professionals
Pocket Guide to Physical Assessment is an invaluable reference for healthcare students, newly qualified and advanced nurse practitioners, and allied health practitioners.
Frequently asked questions
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Information
1
Interviewing and History Taking
1.1 General Procedures
1.1.1 Introduction
1.1.2 Approaching the Patient
- Put the patient at ease by being confident and quietly friendly (Hatton and Blackwood 2003; Jackson and Vessey 2010; Rudolf and Levene 2011; Sawyer 2012).
- Greet the patient: ‘Good morning, Mr/Mrs Smith’. (Address the patient formally and use the full name until the patient has given you permission for less formal address.)
- Shake the patient's hand or place your hand on theirs if the patient is ill. (This action begins your physical assessment. It will give you a baseline indication of the patient's physical condition. For example, cold, clammy, diaphoretic, or pyrexial.)
- State your name and title/role.
- Make sure the patient is comfortable.
- Explain that you wish to ask the patient questions to find out what the patient perceives is the problem or has happened. Start the history taking by stating something like ‘I want to start by asking you some questions about your health’. (Always begin with general questions and then move to more specific questions (Cox 2010) Inform the patient how long you are likely to take and what to expect. For example, after discussing what has happened to the patient, explain that you would like to examine them.
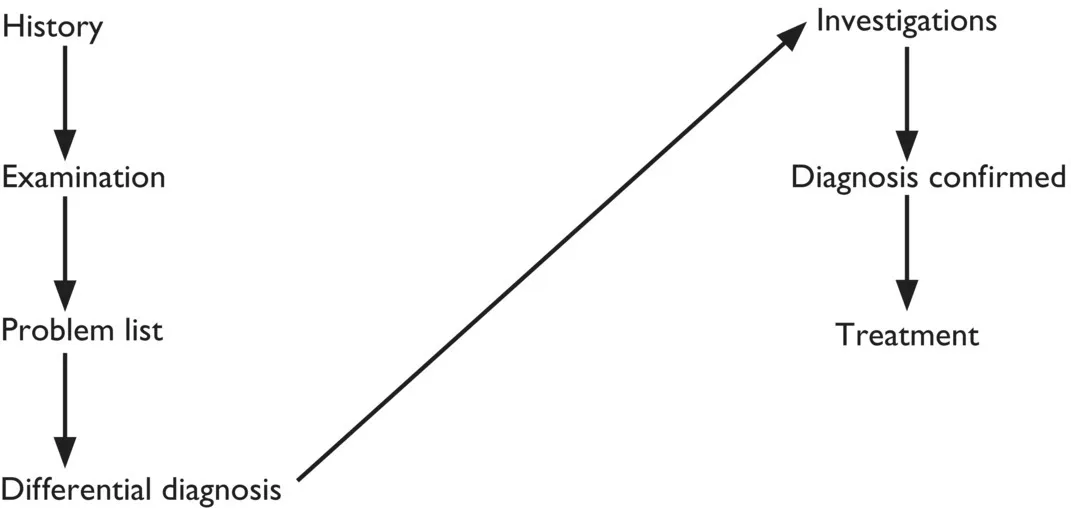
1.1.3 Usual Sequence of Events (Figure 1.1)
1.1.3.1 Importance of the History
- It identifies:
- what the problem is or has happened
- the personality of the patient
- how the illness has affected the patient and family
- any specific anxieties
- the physical and social environment.
- It establishes the practitioner–patient relationship.
- It provides the foundation for your differential diagnoses.
- It often gives the diagnosis.
- Find the principal symptoms or symptom. Ask one of the following questions:
- ‘How may I help you?’
- ‘What has the problem been?’
- ‘Tell me, why have you come to the surgery/clinic/hospital today?’ or ‘Tell me why you came to see me today?’ Effective history taking involves allowing the patient to talk in an unstructured way whilst you maintain control of the interview. Use language that the patient can understand and avoid the use of medical jargon (Collins‐Bride and Saxe 2013; Cox 2010; Sawyer 2012; Tally and O'Connor 2014). Avoid asking questions that can be answered by a simple ‘yes’ or ‘no’. Ask questions that require a graded response. For example, ‘Describe how your headache feels’. Avoid using multiple‐choice questions that may confuse the patient (Cox 2010; Jackson and Vessey 2010). Ask one question at a time. Avoid asking questions like: ‘What's wrong?’ or ‘What brought you here?’ Use clarification to confirm your understanding of the patient's problem. Avoid forming premature conclusions about the patient's problem and above all remain nonjudgemental in your demeanour. Avoid making judgemental statements.
- Let the patient tell their story in their own word...
Table of contents
- Cover
- Table of Contents
- List of Contributors
- Foreword
- Preface
- Acknowledgements
- 1 Interviewing and History Taking
- 2 General Health Assessment
- 3 Basic Examination, Notes, and Diagnostic Principles
- 4 Examination of the CardiovascularSystem
- 5 Examination of the Respiratory System
- 6 Examination of the Abdomen
- 7 Examination of the Male Genitalia
- 8 Examination of the Female Genitalia
- 9 Examination of the Nervous System
- 10 Examination of the Eye
- 11 Examination of the Musculoskeletal System
- 12 Presenting Cases and Communication
- Appendix A: Jaeger Reading Chart
- Appendix B: Visual Acuity 3 Meter/21 Foot Chart
- Appendix C: Hodkinson Ten‐Point Mental Test Score
- Appendix D: Barthel Index of Activities of Daily Living
- Appendix E: Mini‐Mental State Examination (MMSE)
- Appendix F: Glasgow Coma Scale
- Appendix G: Warning Signs of Alzheimer’s Disease
- Appendix H: Trigger Symptoms Indicative of Dementia
- Appendix I: The 12‐Lead Electrocardiogram
- Index
- End User License Agreement