
Obstetric Clinical Algorithms
- English
- ePUB (mobile friendly)
- Available on iOS & Android
Obstetric Clinical Algorithms
About this book
Clinical management algorithms for common and unusual obstetric problems have been developed to help guide practitioners to the best treatment options for patients. In this quick-reference guide, clear diagrams and concise notes show treatment options and evidence for over 80 high-risk obstetric complications, presented in two-page full color spreads to promote quick decision making in time-pressed situations.
This new edition includes sections on obesity, late-preterm and early term delivery, and pregnancy termination. As a clinical manual, the book provides guidance to many common and less common obstetric situations in which either the mother or her fetus is at risk. An algorithm for each situation provides obstetric care providers with a step-by-step guide of necessary actions for any given clinical case.
Written by internationally renowned experts, Clinical Obstetric Algorithms enables all obstetrics care providers to ensure delivery of a healthy mother and a healthy baby.
Tools to learn more effectively

Saving Books

Keyword Search

Annotating Text

Listen to it instead
Information
SECTION 1
Preventative Health
1
Abnormal Pap Smear in Pregnancy
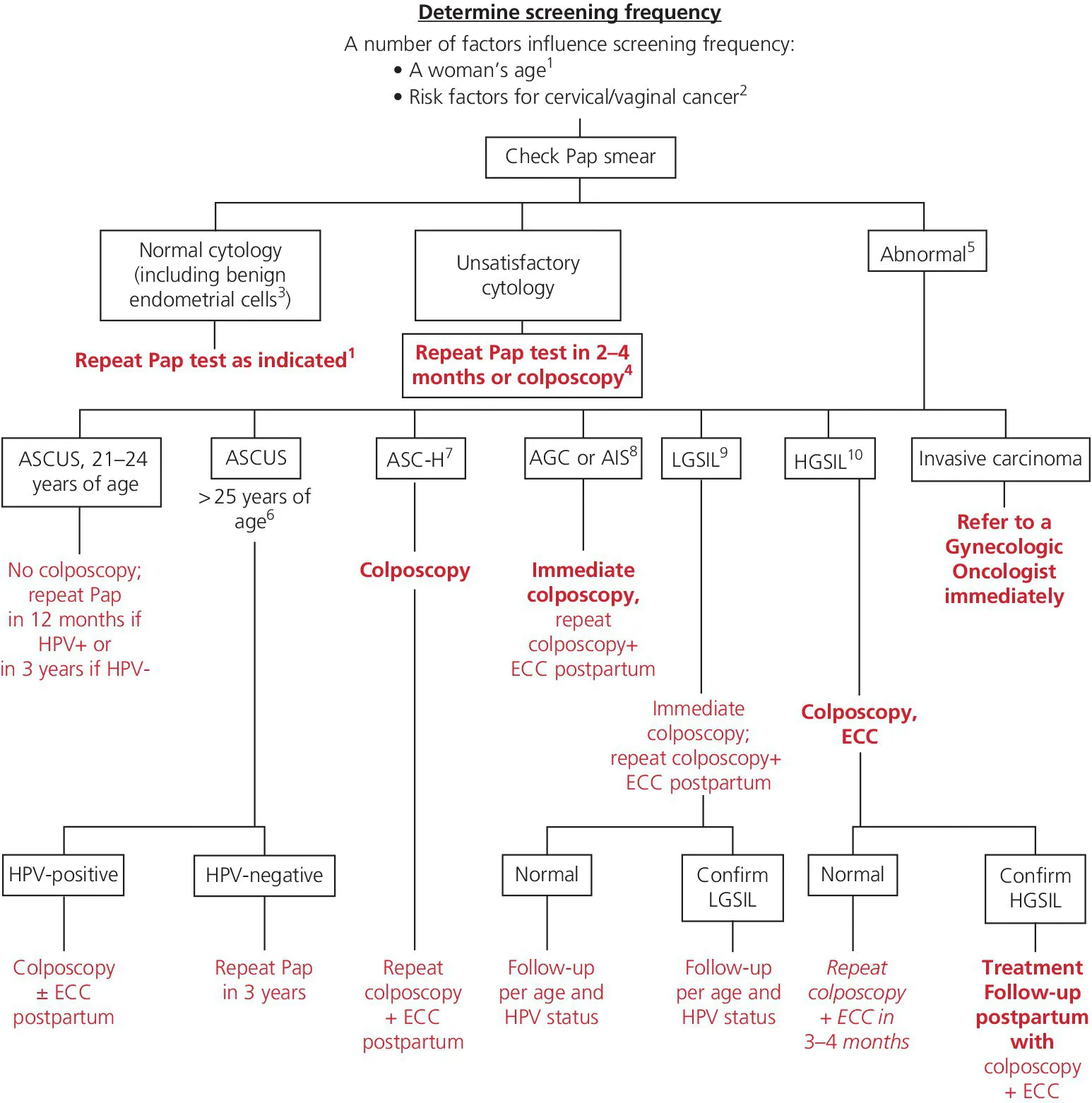
- Recommendations for screening and management of abnormal cervical cytology in pregnancy follow from the general guidelines for screening onset and frequency that were updated in 2012 to reflect the recommendations of the American Cancer Society ACOG, and U.S. Preventive Services Task Force for detection of cervical cancer. Routine pap screening should not be collected until age 21 regardless of first vaginal intercourse. The risk of severe dysplasia or cancer is very low among adolescents, but they should be encouraged to receive human papilloma virus (HPV) vaccination and counseled about safe sex practices to limit exposure to sexually transmitted infections. Women between the age of 21–29 years should be screened with cervical cytology alone. Women >30 years of age should be screened with cytology and HPV testing every 5 years (or with cytology alone every 3 years). Women with a history of cervical cancer, HIV or other risk factors (such as immunocompromise) should continue annual screening. These guidelines and the associated algorithm are based on a large database of patients including adolescents who were managed using former criteria in the Kaiser Healthcare system. The American Society of Colposcopy and Cervical Pathology (ASCCP) has developed an updated free App that can assist with the current recommendations.
- Women who have risk factors for cervical/vaginal cancer (such as a history of in utero diethylstilbestrol (DES) exposure, HIV, women who are immunocompromised, or those on chronic steroids) should be screened annually.
- Women aged 21–29 with normal cytology but absent or insufficient endocervical–transformation zone elements can continue regular screening, which should not include HPV testing. In women >30 years with a similar cytology result, HPV testing is recommended. Positive HPV results should prompt repeat co‐testing in one year, unless the HPV genotype is known to be 16 or 18, in which case, immediate colposcopy is recommended. A negative HPV result in a woman >30 years means that she can go back to routine screening.
- Unsatisfactory cytology is less common in current practice with the use of liquid‐based media for cervical screening. Insufficient squamous cells to detect epithelial abnormalities generally arise from blood or inflammation that obscures the result. Repeat cytology is recommended in 2–4 months. Colposcopy can be considered in women >30 years with positive HPV, and is recommended in those women who have had two consecutive unsatisfactory cytology test results.
- Women should always be informed of an abnormal Pap result by her physician or another healthcare professional who can answer basic questions and allay anxiety. Verbal notification should be followed with written information and clear recommendations for follow‐up. Additionally, if there is evidence of infection along with cellular abnormalities, the infection should be treated.
- The 2012 criteria substantially clarify the management of ASCUS, which is guided by HPV test results whether obtained reflexively or as a co‐test. The management in pregnancy differs only in that colposcopy and endocervical curettage (ECC) should be deferred until 6 weeks postpartum unless a CIN 2+ lesion is suspected. Women >25 years old with a negative HPV test should be returned to a regular three‐year follow‐up cycle. Following pregnancy colposcopy is recommended in women who are HPV+ with annual co‐test follow‐up. Similarly, an endocervical curettage (ECC) should be obtained whenever possible and excisional procedures should be avoided to prevent over‐treatment. In women 21–24 years old, cytology should be repeated in one year. A positive HPV result does not change the recommended follow‐up, but a negative result should return the woman to a three‐year follow‐up cycle.
- Atypical squamous cells cannot exclude high‐grade squamous intraepithelial lesions (HSIL) (ASC‐H), which is associated with a higher risk of CIN 3+ regardless of patient age and a five‐year invasive cancer risk of 2% regardless of HPV status. That said, HPV is highly correlated with ASC‐H, but the cancer risk demands that all women receive immediate colposcopy, including those 21–24 years of age. Colposcopy with directed biopsies of any area that might be concerning for micro invasion should be done by a highly trained clinician. Treatment should be dictated by histologic evaluation of the biopsied lesions.
- Atypical glandular cells (AGC) or adenocarcinoma in situ (AIS) warrant aggressive investigation and close follow‐up. Although the risk of cancer is lower in younger age groups, women >30 years have a 9% risk of CIN3+ and 2% risk of invasive cancer. All such women of all ages should have antenatal colposcopy with 6‐weeks postpartum follow‐up to include colposcopy, ECC and endometrial biopsy (EMB). Subsequent treatment and follow‐up are dictated by the biopsy results, maternal age, and the histologic evaluation of the glandular elements.
- Approximately 60% of low‐grade squamous intraepithelial lesions (LGSIL) will regress spontaneously without treatment depending on the age of the patient, HPV status, and HPV genotype. For women >25 years old in whom HPV testing is negative, repeat co‐testing in ome year is preferred but colposcopy is acceptable. However, if the HPV is positive, then colposcopy is preferred. If colposcopy is not part of the initial evaluation, subsequent co‐testing needs to be entirely normal to allow patients to return to three‐year follow‐up. Any abnormality at the one‐year follow‐up visit should result in colposcopy. In women 21–24 years old, annual repeat cytology without HPV testing is preferred and colposcopy should be avoided unless the results recur for two consecutive years or if one of the following lesions is detected: ASC‐H, AGC, or HSIL. Pregnant women >25 years old with low‐grade squamous intraepithelial lesions should undergo immediate colposcopy without ECC, while those 21–24 years old should be evaluated postpartum.
- High‐grade squamous intraepithelial lesions (HGSIL) are associated with a 60% risk of CIN2+ and a 2% risk of invasive cervical cancer. Immediate colposcopy with directed biopsies of any area that might be concerning for micro invasion is recommended, regardless of maternal age. The antepartum diagnosed of HGSIL should prompt a 6‐weeks postpartum follow‐up colposcopy with ECC and treatment as dictated by the biopsy results. If diagnosed early in pregnancy, colposcopy can be repeated every 12 weeks. Treatment during pregnancy should be reserved for invasive carcinoma and should be managed in concert with a gynecologic oncologist.
2
Immunization
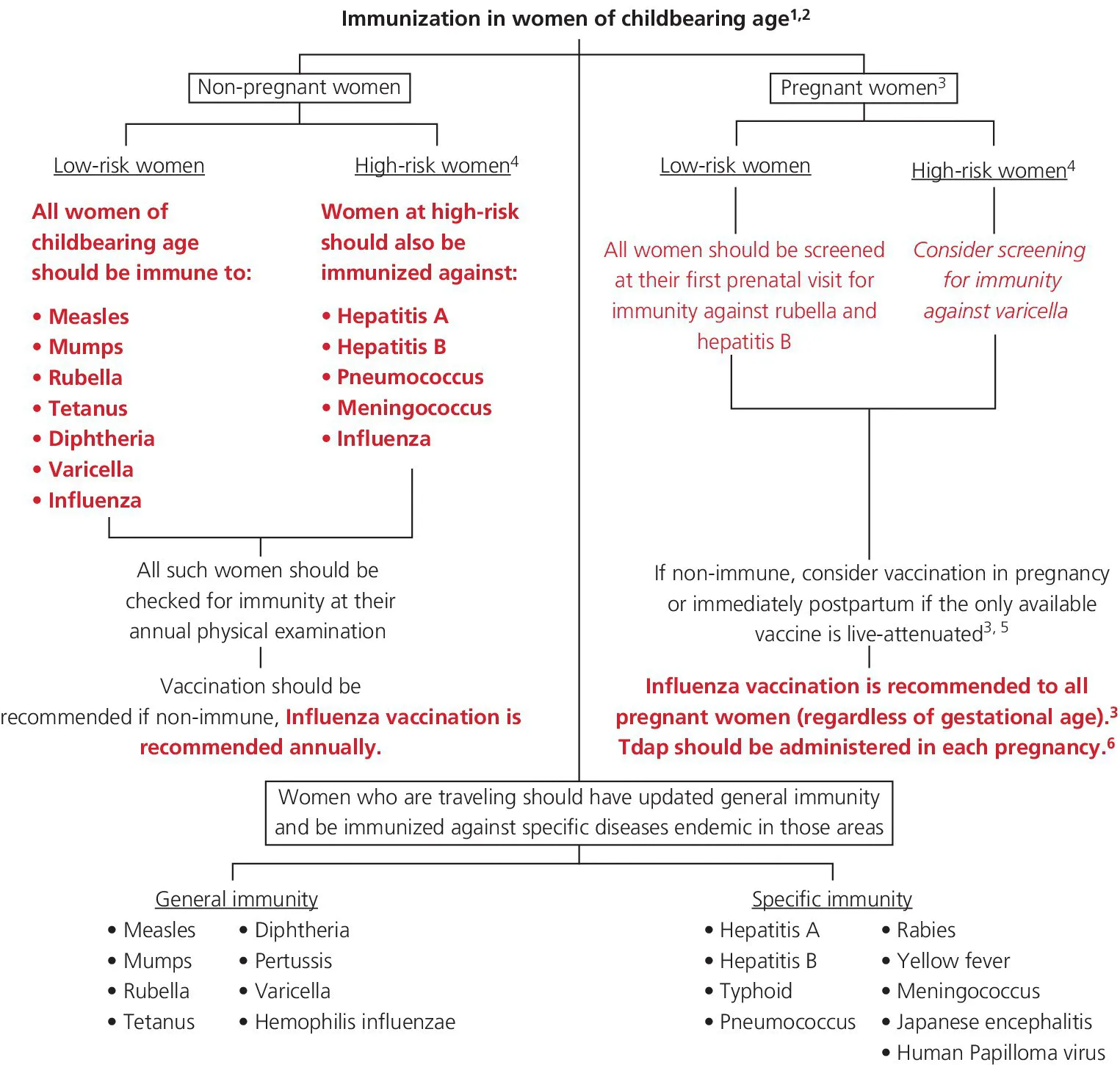
- Immunization can be active (vaccines, toxoid) or passive (immunoglobulin, antiserum/antitoxin). In active immunity, the immune response is induced by wild infection or vaccination, which is generally robust and long‐lasting. As such, subsequent exposure to the vaccine‐preventable infection will result in the release of antibodies and the prevention of illness. In passive immunity, antibodies are acquired passively through maternal transfer across the placenta or breast milk or through the receipt of exogenous immunoglobulins. Protection is temporary and fades within a few weeks to months. The immune system of the recipient is therefore not programmed, and subsequent exposure to vaccine‐preventable infections can lead to active infection.
- Vaccination works by inducing antibodies in recipients that protects them against infection after future exposure to specific disease‐causing microbes. The level of protection varies according to the strength and durability of the immune response induced by the vaccine as well as the virulence, prev...
Table of contents
- Cover
- Title Page
- Table of Contents
- Preface
- List of Abbreviations
- SECTION 1: Preventative Health
- SECTION 2: Maternal Disorders
- SECTION 3: Infectious Complications
- SECTION 4: Antenatal Complications
- SECTION 5: Intrapartum/Postpartum Complications
- SECTION 6: Obstetric Emergencies
- Recommended Reading
- Index
- End User License Agreement
Frequently asked questions
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app