Microneedles for Drug and Vaccine Delivery and Patient Monitoring
- English
- ePUB (mobile friendly)
- Available on iOS & Android
Microneedles for Drug and Vaccine Delivery and Patient Monitoring
About this book
Provides comprehensive coverage of microneedles for delivering and monitoring patient drugs and vaccines
Microneedles are an incredibly active research area and have the potential to revolutionize the way many medicines and vaccines are delivered. This comprehensive research book covers the major aspects relating to the use of microneedle arrays in enhancing both transdermal and intradermal drug delivery and provides a sound background to the use of microneedle arrays in enhanced delivery applications.
Beginning with a history of the field and the various methods employed to produce microneedles from different materials, Microneedles for Drug and Vaccine Delivery and Patient Monitoring discusses the penetration of the stratum corneum by microneedles and the importance of application method and force and microneedle geometry (height, shape, inter-needle spacing). Transdermal and intradermal delivery research using microneedles is comprehensively and critically reviewed, focusing on the outcomes of in vivo animal and human studies. The book describes the important topics of safety and patient acceptability studies carried out to date. It also covers in detail the growing area for microneedle use in the monitoring of interstitial fluid contents. Finally, it reviews translational and regulatory developments in the microneedles field and describes the work ongoing in industry.
- The only book currently available on microneedles
- Filled with tables, graphs, and black and white images (photographs, micrographs)
- Authored by four experts in pharmaceutics
Microneedles for Drug and Vaccine Delivery and Patient Monitoring is an ideal source for researchers in industry and academia working on drug delivery and transdermal delivery in particular, as well as for advanced students in pharmacy and pharmaceutical sciences.
Frequently asked questions
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Information
1
Genesis of Transdermal Drug Delivery
1.1 Skin Anatomy
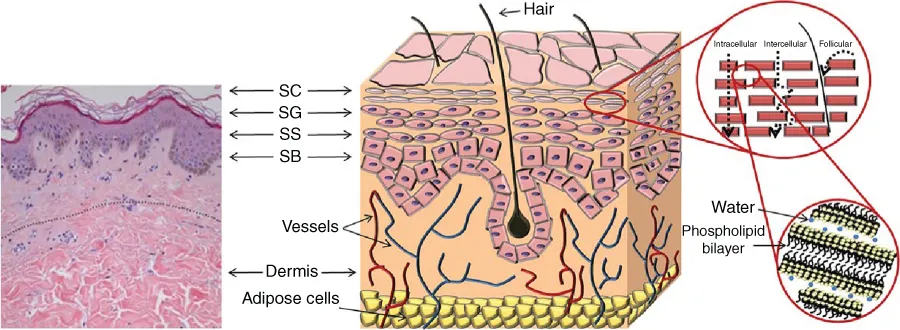
1.1.1 The Epidermis
Table of contents
- Cover
- Table of Contents
- Copyright
- List of Contributors
- About the Editors
- Preface
- Chapter 1: Genesis of Transdermal Drug Delivery
- Chapter 2: Microneedle Manufacturing and Testing
- Chapter 3: Microneedle‐mediated Drug Delivery
- Chapter 4: Microneedle‐mediated Vaccine Delivery
- Chapter 5: Microneedles for Gene Therapy: Overcoming Extracellular and Intracellular Barriers
- Chapter 6: Delivery of Nanomedicines Using Microneedles
- Chapter 7: Minimally‐invasive Patient Monitoring and Diagnosis Using Microneedles
- Chapter 8: Delivery of Photosensitisers and Precursors Using Microneedles
- Chapter 9: Microneedles in Improving Skin Appearance and Enhanced Delivery of Cosmeceuticals
- Chapter 10: Microneedles for Ocular Drug Delivery and Targeting: Challenges and Opportunities
- Chapter 11: Clinical Translation and Industrial Development of Microneedle‐based Products
- Index
- End User License Agreement