![]()
Part One: Mental and behavioral health context
![]()
1
Mental and behavioral health history and context
1.1 Historical perspective
1.1.1 History of psychiatric care
Individuals have attempted to define mental illness as long as we have endeavored to find cures. As a result of a variety of viewpoints, attitudes toward those inflicted with mental illness have ranged from punishing the ill to treating them with compassion. During the Middle Ages in Europe, hospices, workhouses, jails, and asylums housed mentally ill patients. Reports of Germany’s asylums around 1800 describe “mad-cages” where patients were locked up “like criminals.” The French government erected facilities as part of general hospitals, in which the psychiatric patients represented a portion of the residents. Around the same time in England, some psychiatric patients were hospitalized in public or private asylums, with a larger portion hospitalized in the private “nervous clinics” (Shorter, 1997).
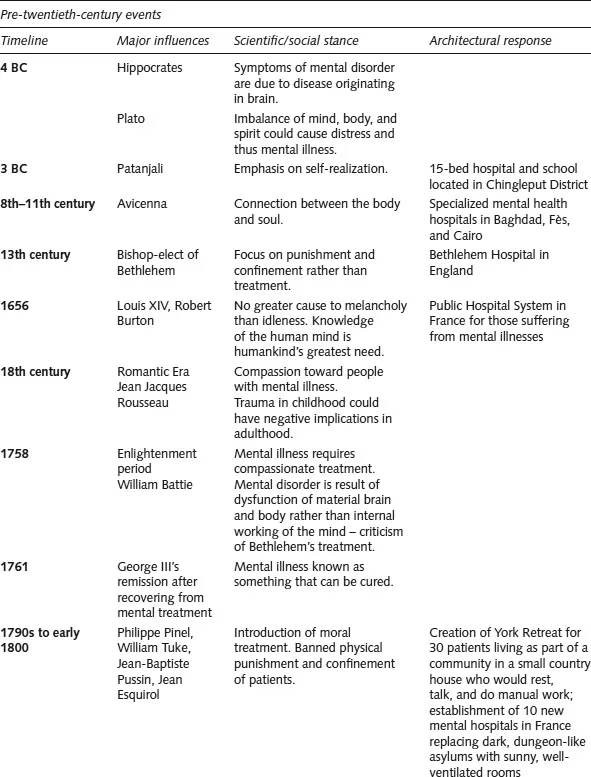
Mental illness was originally perceived to be a function of the mind rather than organic in nature and, as a result, patients were treated harshly. By the end of the nineteenth century, developments in medicine and an enhanced understanding of mental illnesses led to more individualized care and better-trained attendants, which reduced reliance on mechanical restraints (Caplan, 1969). With the evolution of treatment methods, the focus of treatment also changed. Later in the twentieth century, custody and security were not the chief concerns of the facilities. Rather, the emphasis was on providing efficient treatment and successful discharge of patients (Blain, 1956). A summary of scientific/social stances from 4 BC to the present is provided in Figure 1.1.
1.1.2 History of psychiatric facilities
In 1796 the York Retreat, an asylum that pioneered moral treatment, was established by an English businessman, William Tuke. Samuel Tuke, grandson of William, authored the book Practical Hints, in which he discussed design features that can support concepts of moral treatment. Tuke questioned the design of the asylums of the period, which, up to that time, focused on the secure incarceration of patients. Security, he recommended, was to be achieved through direct observation of patients rather than use of physical restraints (Tuke, 1815). He recommended design that allows flexible and liberal access of patients to daylit spaces with fresh air. To reduce anxiety and restlessness and to enhance a sense of autonomy, he recommended employing a variety of scenery and spaces such as galleries for indoor exercise, courts for outdoor exercise, and dayrooms for activity and social interaction. Tuke’s ideal asylum was one in the form of a double-cross or H-shape and included a chapel, baths, and accommodations for patients who also worked at the asylum or became ill (Tuke, 1815).
Figure 1.1: History of significant events and design implications regarding psychiatric care – pre-twentieth-century events
In 1751 the Pennsylvania Hospital in Philadelphia became the first U.S. hospital that accepted psychiatric patients. Shortly thereafter, psychiatric facilities were incorporated into New York Hospital as well as Massachusetts General Hospital. Later hospitals separated psychiatric patient wards from other patients and moved on to create a new form of management (Kirkbride, 1854). Although these mid-eighteenth- to early-nineteenth-century facilities were originally intended to cure patients, they were eventually used for custodial purposes and run by lay administrators who would seek physician consultations. Physical restraints and extreme temperatures were used, since the common belief at the time was that the mentally ill were insensitive to pain and that extreme conditions could shock them back to sanity (Talbott, 1978).
“For most of the nineteenth-century, doctors believed that between 70 and 90 percent of insanity cases were curable, but only if patients were treated in specially designed buildings” (Yanni, 2007, p. 1). U.S. asylums of the period followed a building style introduced by Dr. Thomas Kirkbride, who early in his career at the Institute of Pennsylvania Hospital wrote a book titled On the Construction, Organization and General Arrangements of Hospitals for the Insane. The proposed model included a series of designated patient wards that were staggered to form canted wings that were attached to a central section of the building housing common functions.
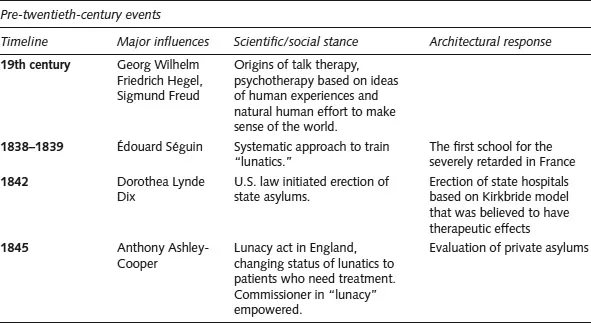
Kirkbride’s prototype provided separate wards dedicated to different groups of patients based on their mental state and gender. In his book, he recommends that each ward include chambers for patients and attendants as well as a dayroom, dining room, bathrooms, housekeeping and storage rooms, and dumbwaiters and staircases to access the common sections of the building. Areas of the building housing more violent or noisy patients were only one story and utilized the single-loaded corridor model. A ward for patients who needed quiet and seclusion was also located at grade. These wards had access to dedicated gymnasiums, yards, and activity areas. The building’s common areas included a lecture room (also used as a lab for experimental purposes), reception, private and common visitation rooms, and the medical and administrative offices. The superintending physician’s residential suite was on the third floor. The basement included building service spaces (kitchens, baker’s room, and laundry) and female workers’ rooms. Patient workrooms, museum, and reading rooms were located in another area (Kirkbride, 1854). Mental hospitals, as reported by Wilbur in 1877, were large and expensive, typically costing more to construct than the equivalent of $2,000 per bed – considerably more than a luxury hotel at the time (see Figure 1.2) (Yanni, 2007).
Figure 1.2: Number of beds per facility and cost, 1887 (Data source: Wilbur, 1887, cited by Yanni, 2007)
The concept of moral treatment was challenged at the end of the nineteenth century when the facilities faced the issue of overcrowding and discharge rates could not keep up with admission rates, which were often determined by court rulings. This problem was exacerbated as immigrant populations increased and state legislatures were reluctant to financially support these facilities. The inevitable imbalance led facilities to use more physical restraints to control patients, limit activities, and employ custodial care in place of moral treatment once again (Talbott, 1978).
The ever-growing patient rate necessitated implementing programs for early discharge of treated patients and preparing them for living in the community. A review of the available design literature at this point (e.g., the design process for the rehabilitation program in the state of Missouri) suggests that the major concern for discharge was that existing hospitals were overcrowded and lacked modern fireproof construction (Bowen, 1939).
As a result of the analysis of data from World War I troops, new principles of care for mental illnesses were established: “proximity, immediacy, and expectancy.” These terms suggest that treatment should take place near where the patient lives, should be provided immediately after the crisis, and that recovery should be expected (Salmon, 1917). The discovery of effective psychopharmacological agents in the 1950s fomented significant developments in the care of serious psychiatric conditions. With these developments, the need for constant observation, seclusion, or physical restraints in hospitals was reduced. More importantly, more patients could function at a level that would allow them to be discharged, which was a promising solution for the issue of overcrowding (Talbott, 1978).
Arguments against overcrowding and quality of residential services discouraged expansion of existing mental health hospitals in the 1950s (Caplan, 1969). Empowered by new methods of treatment and principles of care, discussions began concerning the provision of mental healthcare in different settings and contexts including outpatient clinics, home visiting, community mental health centers as well as the psychiatric units of the mental health hospitals (Caplan, 1969). Many new ideas emerged at this time regarding new forms of care settings such as branch hospitals for the aged as well as geriatric hospitals, day and night hospitals, halfway homes, psychiatric shelter workshops and rehabilitation centers, colonies for the mentally deficient, and therapeutic farms (Blain, 1956).
A series of articles dedicated to the design of mental hospitals appeared in Architectural Record in 1953. The articles were written by psychiatrists and hospital architects and covered new models of care and prototypes of new hospitals and outpatient buildings. Blain, medical director of the American Psychiatric Association at the time, discussed the need for a therapeutic regimen by “combining and focusing on a patient or a group of patients all the influences a hospital could muster to push the patient to recover” (Blain, 1953). Until this time, and based on the work of Salmon, the ideal model of care was to diagnose and treat patients with the goal of returning them to outpatient status as quickly as possible, and hence architects were called on to create environments that would help patients to heal (Guttersen, 1953a). The articles appearing in this issue of Architectural Record described a return to principles of design for moral care as mentioned by Tuke in 1815 (Guttersen, 1953a; 1953b).
However, as early as 1970, concerns were raised regarding the effectiveness of the new models of care that focused on increasing patient discharge rates and outpatient care (Talbott, 1978). Following research on the status of discharged psychiatric patients, a 1977 report sponsored by the National Institute of Mental Health (NIMH) was submitted to Congress addressing chronically mentally ill patients living within the community (Barchrach, 1976). The phenomenon of readmission became problematic at this time, with rates rising from 43% in 19...