![]()
Part I
Innovation and Market Access
![]()
Chapter 1
The Role of Value in Market Access and Pricing Negotiations
Ed Schoonveld
Introduction
Health economists sometimes seem to be their own worst enemy as they tend to insist on presenting evidence of what they think payers should be interested in, rather than focusing on what payers really act on.
How do payers perceive value? How can health outcomes and health economics evidence play a role in demonstrating value? What information can have an impact on market access and pricing decisions? In order to understand this, we must examine the decision-making processes that underlie drug prescribing and funding within each country’s health care system. Some global payer systems use cost-effectiveness methodologies for funding decisions, but most don’t. Many payers use “benefits”-based drug evaluations that are less directly tied to a cost impact benchmark. Health outcomes data can still have a substantial impact as a means of demonstrating value. It does mean, however, that we need to thoroughly understand the particular way in which we can guide decision making in each specific system. Before we look at the topic in more depth, let us first consider why governments feel the need to interfere in drug pricing and what their mindsets are in doing so.
The drug industry is very different from other industries due to cost structure, intellectual property-related aspects and ethical “right to health care” philosophies. A particularly important aspect is that the drug purchasing decision is not a simple buyer versus seller situation but a more complicated interchange between payer, physician and patient. Whether and how various stakeholders interact and influence drug use is very dependent on the payer system. Understanding this process and its implications goes a long way in the identification of critical success factors for market access and pricing of prescription drugs.
The Drug Purchasing Process
When you go to a grocery store to buy fruit, you may rest your eyes on a ripe mango and ask the grocer for the price. If acceptable, you may decide to buy the mango. If too expensive, you may decide to buy cheaper oranges instead. Now suppose you tell the grocer that you are still not convinced that the mangos are tastier than the oranges and insist that he lowers the price of the mangos. The angry response from the grocer may be inappropriate for printing, but will give reference to the fact that if I don’t like the price of the mangos, I should not buy them. Reading this example you may find the suggestion ridiculous; however, this is exactly what is happening for prescription drugs in many countries. Governments in many cases demand that a drug price be lowered rather than deciding not to buy or reimburse it. Why do governments think that it is necessary to insist on a lower price for a product for which they don’t appreciate the value that is claimed by the seller?
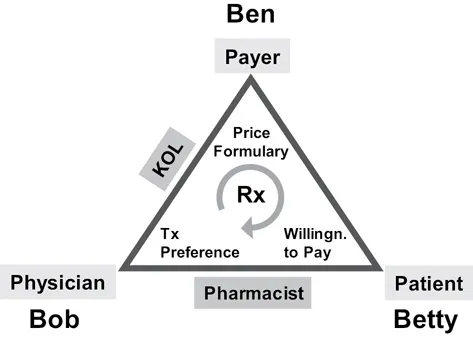
The situation in the prescription drug purchasing process was once described to me as “Dinner for Three” (see Figure 1.1). Imagine three people, Bob, Ben and Betty, go to a restaurant, where Bob orders a meal, Betty eats and Ben pays the bill. You can imagine the conversation where payer Ben suggests that lobster was perhaps a bit excessive. He would be concerned that absent of an obligation to pay, diner Betty may not be sufficiently cost sensitive and might waste his money. The thought of buying a hot dog on the street corner may very well appeal to Ben. He may even claim that hot dogs are not proven to be less healthy. This example may seem far-fetched, but it illustrates the impact of a situation where a natural balance in decision making is distorted. Many governments have felt compelled to intervene in the pricing and reimbursement process for prescription drugs, particularly as drug cost impacts their budget directly. Unfortunately, as many of these controls are ineffective, they tend to lead to new controls, thus moving further and further away from a balanced system, rather than restoring a form of controlled market. A detailed discussion of these and other factors in the economics of the pharmaceutical industry and global drug pricing can be found in Schoonveld (2015).
Understanding Payers
Government and private payers, whether central, regional or local, often play a key role in the availability of prescription drugs for physician prescribing. Payers and their systems vary significantly globally. When we try to convince payers of the need to allow broad usage of our product at a reasonable price, we need to try to understand how a payer evaluates our drug and its value proposition within the context of the system, its cost-management practices, and the decision makers’ individual priorities. How can the drug help a payer reach his or her objectives, and what evidence would he or she like to see to buy into any benefit claims that a manufacturer may put forward? As all payers are not the same, we need to consider how different payers might have different reactions to our value proposition. Hospital payers in Germany might have a different view on your drug’s value than a US managed care pharmacy director or the national Pharmaceutical Benefits Advisory Committee (PBAC) pricing authorities in Australia. The underlying reason for a different perspective on our value proposition can have various causes:
1.National vs. regional or local hospital scope of budget responsibilities
2.Differences in responsibilities with respect to the elements of health care under their remit, such as total medical cost (UK National Health Service or German sick fund) vs. pharmacy cost (for example US Medicare Part D or provincial drug budget holder in Canada)
3.Political and cultural differences between countries, such as a strong “market” philosophy in the US vs. a social equity-driven mindset in Europe
4.Legal differences, for example an obligation for health insurance companies to cover anti-cancer drugs in many US states
5.Differences in the decision-making process and the underlying cost-management principles that payers use in pricing and market access decisions
6.Specific local preferences and priorities, for example due to a particularly high or low incidence of a condition or cost of an intervention in comparison with other locations
The many differences in situations and perspectives between countries has caused every payer system to be unique, which makes the resulting global drug market access and pricing environment very complex. However, upon closer examination one can see that payers use a limited number of underlying cost-management principles to address their drive to ration healthcare utilization within their budget, as a controlling mechanism of an imperfect market for prescription drugs and to enforce their interests as a buyer.
Global Payer Archetypes and Segments
Payers around the world have found different ways to address their concerns with respect to pricing and/or reimbursement of prescription drugs, as described in the previous section. In the United States, private payers have instituted formularies, prior authorizations and step edits, together with co-pay and co-insurance rates, to incentivize patients to use generics and preferred brands. In France, the government has instituted a structured evaluation process of the therapeutic benefit of new drugs over existing “comparators” and is contr...