
eBook - ePub
Healthcare IT Transformation
Bridging Innovation, Integration, Interoperability, and Analytics
John C. Dodd
This is a test
Buch teilen
- 302 Seiten
- English
- ePUB (handyfreundlich)
- Über iOS und Android verfügbar
eBook - ePub
Healthcare IT Transformation
Bridging Innovation, Integration, Interoperability, and Analytics
John C. Dodd
Angaben zum Buch
Buchvorschau
Inhaltsverzeichnis
Quellenangaben
Über dieses Buch
This book gives examples from healthcare institutions that are using IT automation and innovation to drive change and provides guidance on the strategic direction of HIT over the next five years. Improving the delivery of healthcare through HIT is vital for both the economic success of healthcare organizations and the care of the patient, but most EMR systems do not have an integrated and architected approach. This book provides a detailed approach on how to leverage IT for transformation. It also shows how to build upon the experiences of other industries and helps foster innovation by providing a vision of where technology can be an enabler.
Häufig gestellte Fragen
Wie kann ich mein Abo kündigen?
Gehe einfach zum Kontobereich in den Einstellungen und klicke auf „Abo kündigen“ – ganz einfach. Nachdem du gekündigt hast, bleibt deine Mitgliedschaft für den verbleibenden Abozeitraum, den du bereits bezahlt hast, aktiv. Mehr Informationen hier.
(Wie) Kann ich Bücher herunterladen?
Derzeit stehen all unsere auf Mobilgeräte reagierenden ePub-Bücher zum Download über die App zur Verfügung. Die meisten unserer PDFs stehen ebenfalls zum Download bereit; wir arbeiten daran, auch die übrigen PDFs zum Download anzubieten, bei denen dies aktuell noch nicht möglich ist. Weitere Informationen hier.
Welcher Unterschied besteht bei den Preisen zwischen den Aboplänen?
Mit beiden Aboplänen erhältst du vollen Zugang zur Bibliothek und allen Funktionen von Perlego. Die einzigen Unterschiede bestehen im Preis und dem Abozeitraum: Mit dem Jahresabo sparst du auf 12 Monate gerechnet im Vergleich zum Monatsabo rund 30 %.
Was ist Perlego?
Wir sind ein Online-Abodienst für Lehrbücher, bei dem du für weniger als den Preis eines einzelnen Buches pro Monat Zugang zu einer ganzen Online-Bibliothek erhältst. Mit über 1 Million Büchern zu über 1.000 verschiedenen Themen haben wir bestimmt alles, was du brauchst! Weitere Informationen hier.
Unterstützt Perlego Text-zu-Sprache?
Achte auf das Symbol zum Vorlesen in deinem nächsten Buch, um zu sehen, ob du es dir auch anhören kannst. Bei diesem Tool wird dir Text laut vorgelesen, wobei der Text beim Vorlesen auch grafisch hervorgehoben wird. Du kannst das Vorlesen jederzeit anhalten, beschleunigen und verlangsamen. Weitere Informationen hier.
Ist Healthcare IT Transformation als Online-PDF/ePub verfügbar?
Ja, du hast Zugang zu Healthcare IT Transformation von John C. Dodd im PDF- und/oder ePub-Format sowie zu anderen beliebten Büchern aus Medicine & Public Health, Administration & Care. Aus unserem Katalog stehen dir über 1 Million Bücher zur Verfügung.
Information
Chapter 1
Wave 2: Integration–Interoperability and Analytics Overview
Abstract
A patient–consumer focused health learning system with active engaged patients will take new forms of integration, channels of interoperability, and fact-based analytics that both providers, health systems, and most importantly, the patients can use. Some of the key building blocks for this type of transformation are described. The book provides a framework that many can fill in the missing pieces. The current use of health IT has not shown true benefits and improved usability, better focus on integration, and use of new underlying technology that reduces the confusion, the complexity, and the burden on both the patient–consumer and the providers-community caseworkers. This can improve a new enabler of practice transformation for providers of the providers, commute foster engagement by patient–consumers, and link them to their neighborhoods and the communities of health interest. These new simplified interfaces and aligned systems can be real enablers for many with rare diseases, those suffering from cancer, and the most vulnerable populations.
1.1 Introduction
New approaches to health and human services (HHSs) IT can evoke fear and reluctance to change. Most organizations are now on some path toward transformation with a roadmap that is either ad hoc or planned. Those organizations taking the ad hoc path are not sure where that path is leading. The ad hoc path may have started by installing an electronic health record (EHR) system. In some cases, the transitions have not gone smoothly. Are the pieces integrated? Will they interoperate? Will they really contribute to better decision making and analytics? Will this IT transition simplify the provider’s life or make it more complicated? The first ad hoc steps are a key to making change happen.
However, the numerous changes have left many people frustrated, and a more systematic planning approach would be welcome, especially an approach based on lessons learned from the first wave of this transformation, and from other industries. As illustrated in Figure 1.1, we believe that
■ Wave 1 provides the initial building blocks for the transition
■ Wave 2 provides the integration, interoperability, and analytics steps
■ Wave 3 fully achieves systems medicine
There are some early models of Wave 2, such as the State Innovation Models and the Pilot Innovation Projects. However, they need to be integrated together and all turn toward the patient–consumer with each of the major population needs being addressed. Because all of these projects are physician driven, they listen to their colleagues about the payment system, the usability problems of EHRs, the blocking of interoperability by some of the vendors, and the pressure they face to transform their practices. Those issues all have to be addressed, but the key is to understand the needs of the high risk patient–consumer populations and to integrate those needs together into services, information, and actions that include their support teams. While functionality and process in hospitals have improved, and will continue to improve, the key is to keep the patient–consumer healthy and at home, but with the right level of care coordination. This transformation journey is focused on integration, interoperability, analytics, and security from the patient–consumer’s perspective.
A planned Roadmap is needed to move the healthcare and related human services toward better delivery of care to the patient–consumer. Currently, there is a lot of concern about physicians and other professionals. However, if integrated–interoperable IT systems only focus on hospital-to-hospital-to-doctor’s office, we will not make the necessary transformation. Those many fragmented system of systems (SOS) need interoperability as a foundation, but the current systems do not provide an integrated view for the patient–consumers. The focus must shift to the patient–consumer with special attention to high risk, high cost, and vulnerable populations. This book provides the foundational steps for this Patient–Consumer Focused Roadmap, and defines the choices that associations of family advocates, disease foundations, and professional groups along with State Innovation Programs and all healthcare organizations can use in creating their own individual Roadmaps. Establishing this patient–consumer centric foundation will require leadership from government organizations and standards groups. Patient–consumer centric solutions and recommendations are defined in each chapter, but ultimately each organization will have to define its own Roadmap. This does not mean throwing away the existing systems and the many EHRs systems or the websites or tools. It does mean integrating the many topics, services, and sources of information together without introducing any more confusion and complexity. Actually, we want to reduce the confusion by providing new frameworks for both the patient–consumer and a flexible care team with the right support tools (team scaffolding). All of the elements exist today. They just do not exist in the field of HHSs. Ideas are liberally brought from many other fields but adapted to the patient–consumer focus.
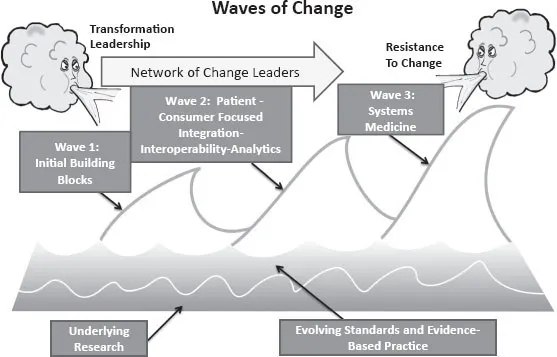
Figure 1.1 Waves of change for healthcare IT transformation.
This book provides advice that can be tailored and adapted to the needs of the individual organization, but there are some foundational elements that are recommended for all. This tailoring and adaptation begins with a focus in Chapter 2 on population patient–consumer needs analysis, the key focal point for the transformation. Many of the elements of confusion are common across all populations. All patient–consumers seem to suffer from some of the same issues with fragmented healthcare, confusing directions from physicians, unclear diagnostics, and a care plan that seems very challenging to follow and understand.
Throughout 2015, there were new messages given by leaders like Dr. Karen DeSalvo of the Office of the National Coordinator for Health Information Technology (ONC) in her many public meetings. Patient–consumer approaches were called for, along with encouraging patient engagement, such as in the October 12, 2015—Strategies for Improving Engagement through Health IT, and also in blogs, such as the December 11, 2015 post noting the meeting at the Bipartisan Policy Center (BPC) on December 8, 2015.
■ Dr. DeSalvo addressed a few key issues, including “the key in my transformation planning—Consumer Access. Consumer Access: Help consumers easily and securely access their electronic health information, direct it to any desired location, learn how their information can be shared and used, and be assured that this information will be effectively and safely used to benefit their health and that of their community.”
■ At the same time, the Secretary of Health for the State of Delaware delivered the same message—Rita Landgraf and the Delaware Center for Health Innovation: Patient and Consumer Messages.
■ As I shared my approaches with many, I heard about the confusion and the need to take the perspective of the patient and consumer rather than always using the physician’s point of view. Nurses and other front line family caregivers stated that they were not being heard.
■ I would even hear confusion at home as my wife dealt with potential health issues with her disabled sister who moved among the family caregivers.
■ The process of understanding the needs of the high risk, vulnerable population is the essence of this Roadmap, with the related solutions that are described, and with the related gap filling solutions that are being developed.
■ But the key is the shift in focus to the patient–consumer, and not to the functions performed in the clinician’s offices and hospitals. I resist the call from the many doctors who state that “those people” could not understand what is needed! In that case, the necessary changes must be presented in a better way. The Roadmaps also must be packaged in a way that is less confusing and that is engaging and interesting.
Those patient–consumer centric interoperable foundational steps are based on the integration and interoperability actions that other industries and other ultra-large systems of systems have undergone. However, these steps are tailored to healthcare IT and to some of the unique patient–provider–policy maker and payer ecosystems that exist in the current fragmented system. They are also tailored to ways the steps can be used as “bridges” connecting with a common set of keystone elements. Those integration and interoperable keystone elements can then create a platform that will allow many paths to transformation with healthcare IT, and will also allow innovation and the individual organization’s own strategic approach.
Today, change is occurring throughout the healthcare IT community, but there is a gap in the guidance. It only now has shifted to patient–consumer engagement. The types of solutions and recommendations in this book fill that void. It will take a number of years to shift the direction from the functional collection tools that are the focus of healthcare IT to those that are user friendly and interoperable, and that provide integrated information, unified content, and services that make sense to patient–consumers and their family caregivers. While this Roadmap aligns with the Federal Health IT Strategy and the ONC Interoperabilities, its focus is in the homes, with the families, and on the neighbors and other supports of those patients most in need of integrated services and information. This patient–consumer centric Roadmap must work at all levels: federal, state, community and, most importantly, with each population group. It will take some time, but most of the building blocks already exist; they just need to be integrated and be interoperable. Yes, easier said than done. But we got a “man on the moon” and we can solve this.
Change is difficult, especially without a Roadmap. Change has its challenges, controversies, and issues, including the overall challenge of political recognition of, and desire for, change. The architecture must be constructed so that it can adapt to
■ Different federal changes (new laws in 2015)
■ New policies and payment reforms
■ New Medicare networks of networks
■ Wider adoption of accountable care organizations (ACOs)
Each healthcare organization needs a flexible underlying integration–interoperability–analytics approach. But this approach does not have to start from scratch.
IT transformations affecting other industries have taken 10 or more years, but these transformations have not been intertwined with the government as is healthcare transformation. The need for IT transformation in many industries, as well as in healthcare, has begun with many small-scale innovations (Wave 1) with limited integration and interoperability. In other industries, Wave 2 would usually address integration and interoperability issues before Wave 3 introduced new innovations and radical new processes, like smart phones or, in the case of medicine, genomics and other new areas of medicine that will arrive.
But first, where are we today and what can we do over the next few years? Wave 3 will have to address not only cost effectiveness and payment reform, but also systems medicine. Wave 3 may break into two more waves, but first address the integration and interoperability that should have been included in Wave 2.
1.1.1 Do We Really Have to Change to Get Patient–Consumer Engagement?
There is currently a critical mass of IT changes being made now. All changes in healthcare IT are local and personal. The United States watched on the sideline while other countries began transformation efforts. The United States has finally moved onto the field, but without a political consensus, and with some rough implementation “incidents.” Incidents, like Healthcare.gov, and like hospitals and doctors’ offices installation of EHR and other systems that contain the basic building blocks but still lack full integration, have often resulted in poor interoperability and inadequate support for analytics. The year 2014 saw improvement in Healthcare.gov, and new standards are starting to address some of the key interoperability gaps. However, many organizations have still not focused on their healthcare IT transformation activities, and have demanded improvement from the vendors, the standards organizations, and the government. More community push is needed.
Engaging the patient–consumers will take more than pointing the folks to the portal. It will require a tailored, focused population-based approach as shown in Figure 1.2.
Some of the ideas have been borrowed from the field of education where those students who are poor (Title 1) or have other special needs are addressed with their own individual instructional education plan. Nursing clinical care plan and the education of nurses use many of those ideas, and also use concept mapping and a phased approach to presenting the complex health information in a more gradual manner. While doctors take pride in their ability to absorb the most complex information and make it through medical schools, they are survivors who recognize that the process they used in graduate school and residency cannot work in a life time of learning.
The Institute of Medicine (IOM) has worked to provide the conceptual basis for a Learning Health System. In the IOM 2011 Workshop Summary report Patients Charting the Course: Citizens Engagement and Learning Health System, there is a great summary and vision statement that begins the report. “The prosperity of a nation is tied fundamentally to the health and wellbeing of its citizens. It follows, then, that citizens—each one a past, current, or future patient—should represent both the healthcare system’s unwavering focus, and it’s fully engaged agents of change.” But that engagement is missing and not encouraged. The health system is confusing, fragmented, and does not ...