Despite decades of well-meaning effort, delivering quality healthcare remains an increasingly complex and costly proposition. Not only is there a long-standing tension between practitioners, political parties, hospital administrators, third-party payers, and patients, but much of the healthcare industry is at odds with fundamental free market business constraints. For example, there is the economic jolt to a once modest electronic medical record (EMR) market, thanks to the Health Information Technology for Economic and Clinical Health (HITECH) component of the American Recovery and Reinvestment Act (ARRA) of 2009 that at first enticed and then prodded physicians to “meaningfully” adopt electronic health records. Then, there is the enactment of the Affordable Care Act in 2010, through which millions of patients have come to view healthcare as an entitlement, immune to the law of supply and demand.
In many respects, the US healthcare industry is being squeezed to provide high-quality, low-cost healthcare to all, akin to FedEx offering guaranteed overnight delivery for the price of a first-class postage stamp, with pickup kiosks on every corner. This despite the fact that, in business, it is commonly accepted that improving the performance of an organization by increasing quality or availability is necessarily associated with a greater cost. It’s for this reason that most successful businesses define a niche for themselves by offering products and services that compete on the basis of quality, cost, or availability (speed)—mutually orthogonal characteristics. For example, FedEx enjoys a brisk business from well-heeled procrastinators by providing guaranteed overnight delivery across the country for 20 times what the US Postal Service charges for regular delivery.
Unlike many other industries, US healthcare has never really achieved steady state, but has instead maintained a more or less constant state of turmoil. Consider just some of the disruptors:
An aging population
The long-standing, worldwide economic slowdown
The increasing dependence on expensive, complex technology
The overhead of Health Insurance Portability and Accountability Act (HIPAA) compliance
The financial implications of the HITECH Act surrounding Meaningful Use
Rising patient expectations
Utter lack of political consensus on the future of healthcare at the federal level
Expansion of the electronic health record (EHR) to include not only the hospital-derived EMR, but the insurer-derived patient health record (PHR)
Evolving Medicare and Medicaid programs, with varying state and federal components
Diminishing physician job satisfaction with cookbook medicine becoming the norm
A long-standing belief among clinicians that financial issues should not interfere with what is best for their patients
Despite the turbidity caused by these divergent perspectives, it’s clear that every healthcare organization can benefit from compiling the metrics required by management to make informed decisions. With the need of hospitals to demonstrate not only EMR adoption but also Meaningful Use, defining and measuring the appropriate indicators are becoming even more critical for institutions dependent on Medicare and Medicaid payments.
The metrics that apply to most healthcare organizations, referred to variably as Key Performance Indicators (KPIs), Quality Indicators (QI), or simply indicators, have been defined by performance-promoting organizations such as the Joint Commission on Accreditation of Healthcare Organizations (JCAHO), Centers for Medicare and Medicaid Services (CMS), and the Agency for Healthcare Research and Quality (AHRQ). The purpose of these indicators ranges from simply securing full Medicare and Medicaid reimbursements to actually helping management more effectively direct the use of their healthcare organization’s resources, maximizing patient safety, and promoting clinical best practices, to increasing patient satisfaction with their healthcare provider.
1.1Performance Management
It is impossible for management to have low-cost access to unlimited quantities of high-quality indicator data—that is, without a disruptive technology, process, or strategy. One such strategy is Performance Management. The basis of Performance Management is the effective use of resources, as measured by quantifying processes and outcomes using indicators that gauge the performance of an organization in particular areas. The strategy relies in part on properly leveraging myriad information technologies, from database management systems’ high-speed networks to software and hardware for data analysis and display.
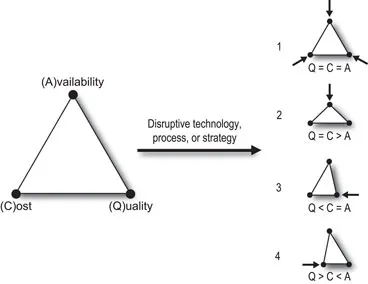
As noted above, cost, availability, and quality are orthogonal qualities in virtually every healthcare organization (see Figure 1.1, left). It is up to management, within physical, economic, and legal constraints imposed on the organization, to define the compromise between the three variables. For example, if management decides that availability—rapid access to care—is the organization’s highest priority, then the cost of care will likely increase and quality may suffer, all else being equal. To achieve this higher availability figure, the director of the emergency room (ER) department may decide to add additional full-time ER physicians on every shift, thereby increasing cost. If, instead, the additional staff are primarily residents from other clinical services, then the cost increase should be less dramatic, but the quality of care may suffer.
Figure 1.1Mutually orthogonal constraints of availability, cost, and quality.
The diagram on the left illustrates the constraints that apply to most business organizations, modeled as the apices of a triangle. As shown in the right diagram, the introduction of a disruptive technology, process, or strategy may reduce the interdependent constraints on each variable, modeled as contracted triangles. An increased focus on quality, cost, or availability incurs less of a deficit in the other two variables. The effect may be symmetrical (1) or asymmetrically favor availability (2), quality (3), or cost (4). Note that the models before and after the introduction of a disruptive technology, process, or strategy in Figure 1.1 are not to scale.
In Figure 1.1 (1), there is a symmetrical contraction of the availability, cost, and quality triangle. In (2), quality and cost remain constant, but availability increases. In (3), quality is improved, while cost and availability remain constant. In the last example, cost is diminished, with no change in quality or availability. The change in cost, availability, and quality is a function of the degree to which the introduction of a disruptive technology, process, or strategy improves the organization’s operation. Furthermore, the shift takes time, and the changes in availability, cost, and quality may not be in sync. For example, shifting from paper-based medical records to an EMR may increase cost acutely, but result in increased access to and quality of patient data. Chronically, cost may gradually decline to a value less than the original cost of maintaining paper records. Using the model introduced in Figure 1.1, the disruptive effects of the technology can be visualized as contraction of the triangle in response to the EMR’s introduction.
Before we delve deeper into the admittedly simplistic model, it’s important to acknowledge my bias. If you note the last sentence above, I unconsciously narrowed the definition of the disruptive agent to a technology. Taking the perspective of an information technology (IT) specialist, every problem calls out for an IT solution. Presuming a reader with an IT background, it’s important to at least recognize the potential bias toward technology solutions, and to be mindful of disruptive processes and strategies. Overreliance on IT technology in a Performance Management Initiative is akin to a clinician’s overindulgence on diagnostic technology. We’re all aware of the ranking of US healthcare worldwide, despite spending the most on healthcare and the associated clinical technologies. So, from here onward, when I mention disruptive technology, keep in mind that the statement generally applies to disruptive processes and strategies as well.
Of course, contraction of the axes of the model with the introduction of the disruptive technology, process, or strategy describes the best-case scenario. The disruptive technology might permanently increase overall cost of patient car...