![]()
CHAPTER 1
Squaring the circle: why physiological labour and birth matter in a technological world
Soo Downe, Sheena Byrom and Anastasia Topalidou
Introduction
The childbirth agenda has changed dramatically over the last decade. In 2004, it was largely taken for granted that both improving the safety and wellbeing of mothers and babies and minimising unnecessary intervention in childbirth were important goals (Downe 2004). However, at the same time as survival rates of women and babies have improved in most (though not all) countries around the world, concern about safety has increased in the public debate, particularly in high-income countries with low rates of maternal and infant deaths. This has occurred in parallel with technological innovation that has brought measuring and monitoring of physical signs closer to individuals, through smartphones and fitness devices. This combination offers the seductive promise of personalised/precision medicine. The argument goes as follows: if only measurement and monitoring can take place at the individual level, from the genetic to the physical, it will be possible to predict, prevent and treat any or all risks and actual pathologies, and reduce harms to zero. Such thinking promotes technical solutions as superior to simple physiology. It can even create an environment where it becomes a moral duty for each individual to submit to assessment of their current health status, to establish their risk for a whole range of future illnesses, and to accept prophylactic treatment of these potential future illnesses. The promise is that this will ensure the optimum health of the population, and especially a healthy old age, even if the identification of potential (but not actual) risk is associated with an increase in anxiety and a reduction in social, psychological, and/or emotional wellbeing.
However, acting on the promise of perfect health without clear evidence that it can indeed be fulfilled comes at a price. If health surveillance and treatment becomes a standard or even a morally expected norm, in the absence of concern for human experience and fulfilment, there is a risk that life choices will be determined only by assumptions about physical risk and pathology. In 2012 the front cover of the BMJ framed this as a slide from ‘Arming the health’ to ‘Alarming the Healthy’ to, eventually, ‘Harming the healthy’ if it is taken too far.a Beyond this, Nietzsche realised that hope (without knowledge of what will actually happen) is a fundamental characteristic of human optimism for life, saying ‘Let your love of life be a love for your highest hope’. (Nietzsche (transl Common) 1999, p29)
It is clear from qualitative studies of what women want and need around the world that both safety and human flourishing matter to childbearing women and their families. The pursuit of the best possible maternity care needs to keep both of these things in balance. Most women and babies in all countries of the world are able to give birth with supportive expert care, without needing treatments or technologies. However, the vast majority of the research and evidence produced in this area is still focused on complications, tests and treatments, and very little is known, still, about the nature and outcomes of physiological labour and birth, and how to enable women to experience it.
Indeed, as fewer women who take part in research studies experience physiological labour and birth, it becomes more and more likely that solutions that work in the context of interventions become generalised to all. For example, a recent study recommended the use of IV rather than IM oxytocin for managed third stage of labour, even though sub-analyses of the data, presented in the paper, imply that there was no benefit of this for women who had spontaneous onset of labour, or who were multiparous (Adnan 2018). There is also an implicit assumption that interventions that are now held to be overused can only be reduced by the introduction of different interventions, rather than by increased support for physiological birth. For example, anecdotally, the results of the recent ARRIVE trial (Grobman 2018) are being widely implemented, resulting in routine induction of all nulliparous women in some hospitals after 39 weeks gestation to reduce caesarean section rates. This demonstrates a very rapid translation of results from a study carried out in one healthcare context (the USA) to other healthcare contexts that vary in a range of ways. In contrast, there has been evidence for some years from studies carried out in a range of countries and contexts that continuous support in labour reduces caesarean section by a greater percentage than that resulting from the ARRIVE trial (Bohren 2017). However, this solution, which requires a reduction in technical support and an increase in human contact and relationships, has not been widely rolled out. The widespread introduction of induction of labour for healthy women and babies also carries the risk of as yet unknown long-term consequences for babies born after labour induction, as is suggested in a recent large population cohort study of almost half a million Australian mothers and babies (Peters 2018). This is in contrast to the introduction of labour support, which has no known short or longer term adverse effects. The paradox of the rapid introduction of technical solutions in maternity care, and the slow or minimal rollout of equally or more effective relationship-based solutions, is the context in which this book is set.
Focusing on solutions
For everyone working in this field, the goal is the same: to understand, to contextualise and to facilitate physiological labour and birth. But all those engaging with this topic do not speak the same scientific language. They do not use common methodologies throughout their daily practice. They may not even have the same views about the importance of this topic, or about the nature of its parameters. Within multinational multidisciplinary collaborations, the experiences and cultural history of each researcher add a particular flavour to the mix (Klein 1990; Frost and Jean 2003; Aram 2004). Getting there requires a kind of suspension of disbelief among all the participants.
The question asked in this book, from our various disciplinary and cultural perspectives, is ‘can we move from risk-disease-orientation to health-orientation in our research endeavours?’. And, in so doing, can we ensure the identification of true pathology while ensuring that false positives don’t render physiological labour and birth obsolete? This approach authentically meets the Alma-Ata definition of health as a state of complete physical, mental and social wellbeing, and not merely the absence of disease or infirmity (Declaration of Alma-Ata, 1978).
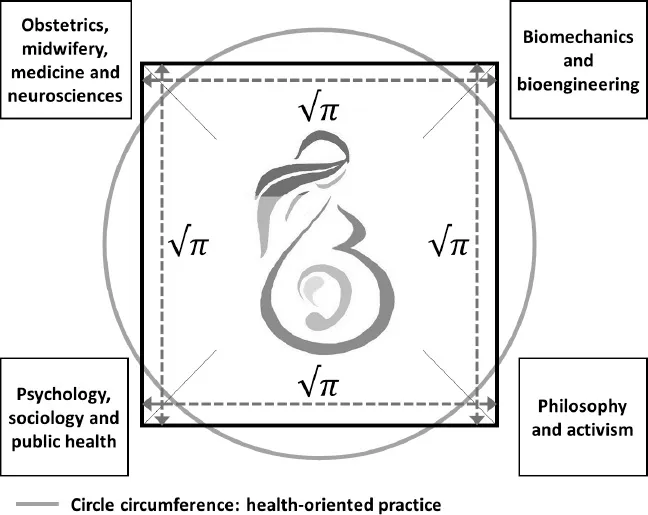
To do this, we have set the goal of squaring the circle of our multiple perspectives, beliefs and experiences. We conceptualise this geometrically in Figure 1. Assume that there is a square, each corner of which represents one scientific group. Let’s say that the angle A is the group of obstetrics, midwifery, medicine and neurosciences, the angle B is biomechanics and bioengineering, at the angle C is the group of psychology, sociology, and public health and at the angle D the group of philosophy and activism. Based on Euclidean definition, a circle is ‘a plane figure bounded by one line, and such that all right lines drawn from a certain point within it to the bounding line, are equal. The bounding line is called its circumference and the point its centre’ (Hazewinkel, 2001). We assume that we have a circle where the circumference is health-oriented and welfare practice, and the centre is the pregnant woman and the foetus, who are in any direction always equidistant from the health-oriented circumference (Figure 1). The following questions then arise: Can we round these corners? Can a scientific solution, a scientific square be created, with the same area as the given circle using only a finite number of steps with compass (scientific techniques) and straight-edge ruler (physiological birth)?
All we needed was to find pi (π). π is the ratio of the circumference of a circle to the diameter. For this book it was defined as authentic, trusting, relationship-based inter-disciplinary cooperation. In our model, this inter-disciplinary cooperation must always be equal to health-orientated practice divided by the wellbeing of the pregnant woman and the foetus.
Figure 1.
Squaring the circle
Conclusion
Reframing maternity services and practices depends on a clear analysis of the current issues, and on proposing new solutions that are exciting, feasible and acceptable. This book brings some of the evidence and debate about normal, physiological labour and birth up to date, from a multidisciplinary perspective. The chapters cover topics from architecture to epigenetics, and from organisational analysis to theory and philosophy. In the process, the authors engage with some of the key questions that are outstanding in this area. They all also offer insights into possible solutions and ways forward.
For the sake of the future health of mothers, babies, families and societies, we have to better understand childbirth physiology and how to support it, both to promote it where it is possible and desirable, and to identify and deal with true pathology. Squaring the interdisciplinary circle is probably the best and only way to achieve this. We hope that readers of this book find our attempt useful and enlightening.
References
Adnan, N. Conlan-Trant, R., McCormick, C., Boland, F., Murphy, D.J. (2018) ‘Intramuscular versus intravenous oxytocin to prevent postpartum haemorrhage at vaginal delivery: randomised controlled trial’ BMJ 2018; 362 doi: https://doi.org/10.1136/bmj.k3546
Aram, J.D. (2004) ‘Concepts of Interdisciplinarity: Configurations of Knowledge and Action’ Human Relations 57(4):379–412.
Bohren MA, Hofmeyr GJ, Sakala C, Fukuzawa RK, Cuthbert A. Continuous support for women during childbirth. Cochrane Database of Systematic Reviews 2017, Issue 7. Art. No.: CD003766. DOI: 10.1002/14651858. CD003766.pub6.
Declaration of Alma-Ata. (1978) International Conference on Primary Health Care, Alma-Ata, USSR, 6-12 September 1978.
Downe, S. (Ed) (2004) Normal Childbirth, Evidence and Debate, Churchill Livingston.
Frost, S.H. and Jean, P.M. (2003) ‘Bridging the Disciplines—Interdisciplinary Discourse and Faculty Scholarship’ Journal of Higher Education 74(2):119–149.
Grobman, W.A., Rice, M.M., Reddy, U.M., Tita, A.T.N., Silver, R.M., Mallett, G. et al (2018) ‘Labor Induction versus Expectant Management in Low-Risk Nulliparous Women (the ARRIVE trial)’. N Engl J Med; 379:513-523
Hazewinkel, M. (Ed) (2001), ‘Circle’, Encyclopedia of Mathematics, Springer, ISBN 978-1-55608-010-4
Klein, J.T. (1990) Interdisciplinarity: history, theory and practice, the Wayne State University Press, Detroit.
Nietzsche, F. (transl Common, T.) (1999) Thus Spake Zarathustra, Dover Publications, New York.
Peters, L.L., Thornton, C., de Jonge, A., Khashan, A., Tracy, M., Downe, S., Feijen-de Jong, E.I., Dahlen, H.G. (2018) ‘The effect of medical and operative birth interventions on child health outcomes in the first 28 days and up to 5 years of age: A linked data population-based cohort study’ Birth 45(4):347-357. doi: 10.1111/birt.12348. Epub 2018 Mar 25.
Illustrations
Figure 1: With permission from Olga Gouni (www.cosmoanelixis.gr): we also acknowledge that the central logo is used for EU COST Action IS1407 BIRTH (Building Intrapartum Research Through Health) eubirthresearch.eu, also with permission from Olga Gouni.
Footnote
a www.bmj.com/content/344/bmj.e3783/rr/588178
![]()
PART I
The nature and context of normal birth
![]()
CHAPTER 2
Nature and consequences of oxytocin and other neuro-hormones during the perinatal period
Sarah Buckley and Kerstin Uvnäs Moberg
Introduction
Childbearing is an amazing and biologically complex process. From pregnancy through to the early postpartum period, reproduction-related hormonal and neuro-hormonal systems facilitate adaptive physiological processes in both mother and foetus/baby that promote survival and safety for both.1, 2
Over millions of years of mammalian evolution, these hormonal processes have also supported successful lactation and maternal-infant bonding/attachment, both essential to species survival for all mammals, and biologically ‘intertwined and continuous’ with the processes of labour and birth.1, 2
Clinicians and researchers are increasingly acknowledging the importance and influence of the intricate neurohormonal orchestration of physiological birth, including long-term positive effects for mothers and babies.1–5. However, fewer women and babies are experiencing the full hormonal orchestration of physiological birth, due to rising rates of interventions worldwide.6
There is currently limited understanding of the impacts of interventions during and immediately after childbirth on these delicate, adaptive, organising processes. Current biological knowledge predicts that these positive effects could be disrupted by interventions, with possible longer-term consequences.7–9
This chapter summarises key knowledge and research findings in this area, focusing on the oxytocin system, the hypothalamic-pituitary-adrenal (HPA) axis (including cortisol), the autonomic nervous system (ANS) and other neurogenic and hormonal systems that mediate stress adaptations in childbear...