![]()
Chapter 1
Care of the Term Infant
1. How is a term infant defined?
The World Health Organization (WHO) defines a term infant as one who is greater than 37 weeks’ gestation. Recent evidence, however, has demonstrated that infants born at 37 weeks’ gestation behave differently from infants delivered at 39 and 40 weeks’ gestation. The more mature term infant (39 or 40 weeks) has fewer respiratory problems, less difficulty with feeding and hyperbilirubinemia, reduced birth injury, a greater ability to respond to infection, and an overall reduction in rates of neonatal complications.
Given that infants born before 37 weeks have even greater liability for problems, the recognition that true term status begins at about 39 weeks’ gestation has led the American College of Obstetrics and Gynecology (ACOG) and the American Academy of Pediatrics (AAP) to recommend that no infants be delivered electively before 39 weeks. ∗†
2. What is the average birth weight of a term infant?
The mean birth weight of a term infant is approximately 3400 grams, or approximately 7 pounds, 7 ½ ounces. Mean length, which is sometimes difficult to measure accurately, is approximately 52 to 53 centimeters, or 20 inches, and head circumference averages 34 centimeters, or approximately 13.5 inches. Of note is the fact that birth weight in recent years has declined slightly, even though premature births have been declining. ∗
3. How often is neonatal resuscitation necessary for a term infant?
Approximately 10% of all infants need some assistance at birth (e.g., stimulation, oxygen), and approximately 1% need extensive assistance (e.g., positive pressure ventilation, fluids, drugs) at the time of birth. ∗
4. What are the critical skills needed by any individual called upon to resuscitate a neonate?
The ability to rapidly and accurately evaluate the newborn’s condition
Knowledge of the risk factors that may predispose the neonate to resuscitation
Indications for neonatal resuscitation
Skill in airway management
Skill in umbilical catheter placement
Skill in insertion of chest tubes
Understanding of the capabilities of the resuscitation team
Knowledge of the hospitals’ facilities for neonatal care
5. What is an Apgar Score?
The Apgar score is a clinical assessment developed by Dr. Virginia Apgar at Columbia University during the early 1950s. Dr. Apgar was a great pioneer for women in medicine, and her development of the Apgar score is just one of her many landmark contributions to medicine. Although she was an anesthesiologist, she was very concerned about the status of newborn infants immediately after delivery. Her score, which was designed to evaluate both the immediate and long-term well-being of a neonate, has been reassessed periodically and still appears to be as valid today as when it was first introduced.
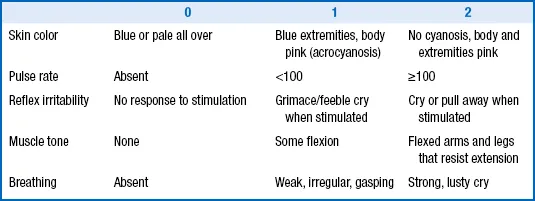
The Apgar score is determined at 1 and 5 minutes of life and consists of the measures listed in Table 1-1. These measures are scored 0, 1, or 2, then totaled.
TABLE 1-1
THE APGAR SCORE
It is rare for an infant to have an Apgar score of 10 (the highest possible score) in the absence of oxygen administration because the exposure of most newborn infants to the environmental temperature of the delivery room will cause some acrocyanosis of the hands and feet, reducing the potential score to 9. An Apgar score above 7 is considered good, one between 4 and 7 demands close observation, and one that is 3 or lower usually requires some intervention. Even with the changes that have occurred in modern medicine, the Apgar score has retained its value. ∗
5a. How should the Apgar change in the immediate postnatal period?
One of the other important aspects of the Apgar score is the change between 1 and 5 minutes of life. For vigorous term infants the Apgar score does not change significantly between 1 and 5 minutes of life. Changes in the Apgar score, however, are useful for assessing the response to resuscitation. For example, a newborn infant who has a 1-minute Apgar score of 3 and a 5-minute score of 8 has probably had some terminal difficulty at the time of delivery that has been quickly surmounted. On the other hand, the neonate with Apgar scores of 3 and 4 at 1 and 5 minutes is not responding well and may need further intervention. When an infant’s 5-minute score is 5 or lower, it has become customary to continue to provide Apgar scores every 5 minutes up to 20 minutes of life or until the score is above 7. Slow improvement in an Apgar score may be associated with some element of hypoxia or ischemia during the delivery, but there are many other reasons for low Apgar scores. A low Apgar score at 1 or 5 minutes has a poor positive predictive accuracy for later disabilities.
6. What should be done to prepare for the delivery of a term infant?
When called to the delivery of a term infant, the clinician should first make sure that all possible tools that might be needed for resuscitation and maintenance of a thermal neutral environment are ready. Although the great majority of term infants in an uncomplicated pregnancy do not require any intervention, it is important to be prepared for any possibility. In addition, a number of other routine items are necessary. On arrival in the delivery room the following items should be checked:
The radiant warmer should be turned on, and a temperature probe that can be attached to the skin should be available.
Several dry towels and blankets should be heated under the radiant warmer for the infant.
A resuscitation bag or a T-piece device should be available with masks of several sizes. If the gestational age of the infant is known, the most appropriate mask size can be chosen (typically a size 1 for term infants).
An oxygen source should be available. In most instances resuscitation with 21% oxygen can be used initially if respiratory intervention is required.
A laryngoscope and endotracheal (ET) tubes should be available. For the term infant, a 0 or 1 laryngoscope blade is appropriate, and a 3.5 FR ET tube should be used. Note: Although it may be easier to insert a smaller ET tube, this approach ignores the fact that work of breathing will be dramatically increased with a tube that is too small for the size of the infant.
Umbilical catheters, size 3.5 and 5 FR, should be available along with D10W fluid and lactated Ringer’s solution. Feeding tubes should also be available for insertion into the stomach to drain the contents or air.
A pulse oximeter should be available. In term infants needing resuscitation, the pulse oximeter provides valuable information (heart rate and oxygen saturation levels) regarding whether the interventions are succeeding.
A medication box should be present with all medications that might be necessary for resuscitation of a neonate. Although the use of medications such as bicarbonate and calcium have fallen out of favor, there are unique situations in which these solutions may be needed as well as pressor drugs, such as epinephrine, Prostaglandin E1 for ductal dilation, and narcotic antagonists such as naloxone. Rarely are any other medications required in the delivery room.
Suction for the removal of meconium and the emptying of stomach contents must be present.
An umbilical cord clamp and scissors should be on hand.
Erythromycin eye ointment should be present for prevention of gonococcal ophthalmia.
Vitamin K
1 for the prevention of vitamin K–dependent hemorrhagic disease of the newborn should be on hand.
7. Why is temperature control of the delivery room so important for a term infant?
Immediately before delivery the fetus is bathed in amniotic fluid and maintained at a temperature identical to that of the mother. Within se...