eBook - ePub
Scientific Aspects of Dialysis Therapy
H. Kawanishi, Y. Takemoto
This is a test
- 278 Seiten
- English
- ePUB (handyfreundlich)
- Über iOS und Android verfügbar
eBook - ePub
Scientific Aspects of Dialysis Therapy
H. Kawanishi, Y. Takemoto
Angaben zum Buch
Buchvorschau
Inhaltsverzeichnis
Quellenangaben
Über dieses Buch
This book brings together papers presented both during the 61st Annual Meeting of the Japanese Society for Dialysis Therapy (JSDT) and the 34th Congress of the International Society of Blood Purification (ISBP), held in Osaka in June and in Hiroshima in September 2016, respectively. They cover a broad spectrum of topics, ranging from hemodialysis, peritoneal dialysis, hemodiafiltration and technical innovations in blood purification to complications of chronic kidney disease and acute kidney injury, including mineral bone disease and anemia.
Häufig gestellte Fragen
Wie kann ich mein Abo kündigen?
Gehe einfach zum Kontobereich in den Einstellungen und klicke auf „Abo kündigen“ – ganz einfach. Nachdem du gekündigt hast, bleibt deine Mitgliedschaft für den verbleibenden Abozeitraum, den du bereits bezahlt hast, aktiv. Mehr Informationen hier.
(Wie) Kann ich Bücher herunterladen?
Derzeit stehen all unsere auf Mobilgeräte reagierenden ePub-Bücher zum Download über die App zur Verfügung. Die meisten unserer PDFs stehen ebenfalls zum Download bereit; wir arbeiten daran, auch die übrigen PDFs zum Download anzubieten, bei denen dies aktuell noch nicht möglich ist. Weitere Informationen hier.
Welcher Unterschied besteht bei den Preisen zwischen den Aboplänen?
Mit beiden Aboplänen erhältst du vollen Zugang zur Bibliothek und allen Funktionen von Perlego. Die einzigen Unterschiede bestehen im Preis und dem Abozeitraum: Mit dem Jahresabo sparst du auf 12 Monate gerechnet im Vergleich zum Monatsabo rund 30 %.
Was ist Perlego?
Wir sind ein Online-Abodienst für Lehrbücher, bei dem du für weniger als den Preis eines einzelnen Buches pro Monat Zugang zu einer ganzen Online-Bibliothek erhältst. Mit über 1 Million Büchern zu über 1.000 verschiedenen Themen haben wir bestimmt alles, was du brauchst! Weitere Informationen hier.
Unterstützt Perlego Text-zu-Sprache?
Achte auf das Symbol zum Vorlesen in deinem nächsten Buch, um zu sehen, ob du es dir auch anhören kannst. Bei diesem Tool wird dir Text laut vorgelesen, wobei der Text beim Vorlesen auch grafisch hervorgehoben wird. Du kannst das Vorlesen jederzeit anhalten, beschleunigen und verlangsamen. Weitere Informationen hier.
Ist Scientific Aspects of Dialysis Therapy als Online-PDF/ePub verfügbar?
Ja, du hast Zugang zu Scientific Aspects of Dialysis Therapy von H. Kawanishi, Y. Takemoto im PDF- und/oder ePub-Format sowie zu anderen beliebten Büchern aus Medicine & Nephrology. Aus unserem Katalog stehen dir über 1 Million Bücher zur Verfügung.
Information
Thema
MedicineThema
NephrologyPeritoneal Dialysis and Hemodialysis
Kawanishi H, Takemoto Y (eds): Scientific Aspects of Dialysis Therapy: JSDT/ISBP Anniversary Edition.
Contrib Nephrol. Basel, Karger, 2017, vol 189, pp 61-64 (DOI: 10.1159/000450672)
Contrib Nephrol. Basel, Karger, 2017, vol 189, pp 61-64 (DOI: 10.1159/000450672)
______________________
Peritoneal Dialysis or Hemodialysis: Present and Future Trends in the United States
Andre A. Kaplan
University of Connecticut Health Center, Farmington, Conn., USA
______________________
Abstract
In 2013, 88.4% of all incident end-stage renal disease (ESRD) patients began renal replacement therapy with hemodialysis (HD) while 9.0% began with peritoneal dialysis (PD). The remaining 2.6% received a preemptive kidney transplant. In the US, outpatient HD units are widely distributed and economy of scale has resulted in HD being the most common ESRD modality. Use of PD and preemptive kidney transplant were relatively more common in younger groups and relatively less common among Black and Hispanic patients. Of note is that the new Medicare reimbursement system, known as the ‘bundle’, provides substantial financial incentives to do PD as opposed to in-center HD. By the end of 2013, 63.9% of all prevalent ESRD cases were receiving HD, 6.9% were being treated with PD, and 29.3% had a functioning kidney transplant. Distributions of modality use by patient characteristics generally mirror those for incident patients. PD and kidney transplant were more commonly used among patients who were younger and were more likely to be non-Hispanic Whites. Differences in the use of home dialysis (PD and HD) are largely driven by differences among individual dialysis centers or groups of centers, rather than by large-scale regional effects. Thus, the future use of PD or home HD will be driven by the proclivities of the largest dialysis providers, which, in turn, are driven by financial reimbursement.
© 2017 S. Karger AG, Basel
Peritoneal Dialysis versus Hemodialysis in the United States: Current Status
In the US, the best data on dialysis modality is available from the USRDS (United States Renal Data System). This database is compiled from Medicare and Medicaid payment information, encompassing the quasi-totality of all end-stage renal disease (ESRD) patients treated. The most recent data is from 2013 when 88.4% of all incident dialysis patients began renal replacement therapy with hemodialysis (HD) while 9.0% began with peritoneal dialysis (PD) [1]. The remaining 2.6% received a preemptive kidney transplant. In the US, outpatient HD units are widely distributed and economies of scale have resulted in HD being the most common ESRD modality. Use of PD was relatively more common in younger groups and relatively less common among Black or Hispanic patients. Given that, as a group, American patients entering ESRD are getting older and given that Blacks and Hispanics are making up a larger percentage of the American population, PD may continue to represent a relatively minor percentage of ESRD treatments.
In 2013, the proportion of incident dialysis cases using home dialysis (PD and HD) was 10.2%. This represents a 52% increase from a decade ago in 2003 and 71% higher than at its nadir in 2007. Use of PD was 63% higher than in 2007 while home HD was 222% higher than in 2007; however, the overall use of home HD among incident ESRD patients is low, as only 9.1% of home dialysis patients were treated with it. Of note, the new Medicare reimbursement system, known as the ‘bundle’, provides substantial financial incentives to do PD as opposed to in-center HD. Reimbursement for home HD is more complex and depends on the machine used. The standard dialysis machines are the least expensive to run but require extensive plumbing alterations which become useless if the patient is transplanted. An increasingly popular home HD machine is by NxStage and does not require extensive plumbing. Unfortunately, the clearance provided by a single NxStage treatment is inferior to that of standard HD and most patients will require 4 or more treatments to meet adequacy goals. For PD, as with HD, there is a large difference in reimbursement depending on whether the patient is covered by Medicare or private insurance.
By the end of 2013, 63.9% of all prevalent ESRD cases were receiving HD, 6.9% were being treated with PD, and 29.3% had a functioning kidney transplant. Distributions of modality use by patient characteristics generally mirror those for incident patients. PD and kidney transplant were more commonly used among patients who were younger and were more likely to be non-Hispanic Whites. Differences in the use of home dialysis (PD and HD) are largely driven by differences among individual dialysis centers or groups of centers, rather than by large-scale regional effects. Thus, the future use of PD or home HD will be driven by the proclivities of the largest dialysis providers, which, in turn, are driven by financial reimbursement.
Table 1. BMI values of patients in PD studies
Hong Kong (1996-1999) | 22 |
ADEMEX (1998-2001) | 25.5 |
Canada (1999) | 25.5 |
CANUSA (1990-1992) | 24.6 |
USA (2002) | 28 |
Modified from [5]. | |
Peritoneal Dialysis versus Hemodialysis in the United States: How Did We Get to the Current Status?
In 1988, the USRDS described the use of PD in the US for each year from 1977 onward. The data demonstrated that the percentage of prevalent dialysis patients treated with PD gradually decreased from 16% in 1977 to about 13% by 1997 [2, 3]. Subsequent data reported by the USRDS in 2015 demonstrated a further decline in the percentage of dialysis patients treated with PD. This decline was heralded by a particular dip in the absolute number of PD patients, which became noticeable after 1997 (fig. 1) [1]. Some believe this dip in the percentage of PD patients is, at least partially, a result of the publication of the 1997 DOQI guidelines, recommending a Kt/V of 2 per week as adequate urea clearance [4]. As seen in table 2, this goal requires a larger burden of PD exchanges per day and may have convinced many physicians and their patients that PD would be too demanding, especially for larger patients as their residual renal function declined. In this regard, BMI estimates for PD patients in several landmark studies reveal that American dialysis patients tended to be larger than those in other countries [5].
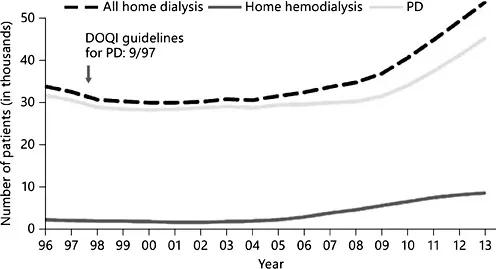
Fig. 1. Prevalent dialysis patients in the US from 1996 to 2013: PD and Home HD. Note the decline in PD patients after the introduction of the 1997 DOQI guidelines recommending a Kt/V urea of 2.0/week. Figure modified from the 2015 Annual Report of the USRDS.
Table 2. PD prescriptions to achieve a weekly Kt/V of 2
PD adequacy at a Kt/V of 2/week for 70 kg patient at 42 liters of V |
2 liters every 6 h (4 exchanges/day) would provide 2.5 liters of PD effluent every 6 h with 100% equilibration of urea = 10 liters of urea clearance/day = 10/42 × 7 days = 70/42 or Kt/V of 1.67/ week. To achieve a Kt/V of 2, the patient would need a Kt/V of 0.33/week from residual renal function = 0.33 × 2.0= 13.86 liters/week = 1.98 liters of urea clearance/day = 1.38 ml/min of residual renal clearance. This prescription would require only 4 exchanges per day. |
PD adequacy at Kt/V of 2/week for 90 kg patient at a Kt/V at 54 liters of V |
2 liters every 5 h (5 exchanges/day) would provide 2.5 liters of PD effluent every 5 h with 90% equilibration of urea = 11.25 liters of urea clearance/day = 11.25/54 × 7 days = 78.5/54 or Kt/V of 1.45/week. The patient would need a Kt/V of 0.55/week from residual renal function = 29.7 liters/ week = 4.24 liters of urea clearance/day = 2.94 ml/min of residual renal clearance. This prescription would require 5 exchanges/day and more residual renal function. |
Since the ADEMEX publication [6], the DOQI goals for PD adequacy have been reduced to a Kt/V urea of only 1.7 per week (table 1). This goal was more reasonable for many of the larger American dialysis patients and the percentage of incident dialysis patients choosing PD has begun to increase. At present, PD represents approximately 9.7% of all prevalent ESRD patients on dialysis.
Peritoneal Dialysis versus Hemodialysis in the United States: Where Are We Going?
In 2011, The Centers for Medicare and Medicaid Services (CMS) implemented a new payment system to reimburse physicians and dialysis providers for ESRD services. This new payment system, known as the ‘bundle’, combined payment for dialysis services with reimbursement for dialysis-related medication. By eliminating separate billing for dialysis-related drugs, CMS stated that they wanted to encourage use of home dialysis, with PD being the most common home-based modality. A detailed financial analysis resulting from the implementation of the ‘bundle’ has been presented by John Burkart [7]. Assuming practice patterns prevalent in 2006, he estimated the following changes: for each in-center HD patient, the total monthly reimbursement will likely be decreased by about USD 47.00. For each home PD patient, the total monthly reimbursement will likely be increased by about USD 629.00. These differences will provide substantial financial incentives to increase PD utilization.
Conclusions
In the past, the favored modality of in-center HD versus home PD had been driven by financial considerations and the difficulty of...
Inhaltsverzeichnis
Zitierstile für Scientific Aspects of Dialysis Therapy
APA 6 Citation
[author missing]. (2016). Scientific Aspects of Dialysis Therapy ([edition unavailable]). S. Karger. Retrieved from https://www.perlego.com/book/723063/scientific-aspects-of-dialysis-therapy-pdf (Original work published 2016)
Chicago Citation
[author missing]. (2016) 2016. Scientific Aspects of Dialysis Therapy. [Edition unavailable]. S. Karger. https://www.perlego.com/book/723063/scientific-aspects-of-dialysis-therapy-pdf.
Harvard Citation
[author missing] (2016) Scientific Aspects of Dialysis Therapy. [edition unavailable]. S. Karger. Available at: https://www.perlego.com/book/723063/scientific-aspects-of-dialysis-therapy-pdf (Accessed: 14 October 2022).
MLA 7 Citation
[author missing]. Scientific Aspects of Dialysis Therapy. [edition unavailable]. S. Karger, 2016. Web. 14 Oct. 2022.