
eBook - ePub
Adoptive Cellular Immunotherapy of Cancer
H. C. Stevenson
This is a test
Compartir libro
- 264 páginas
- English
- ePUB (apto para móviles)
- Disponible en iOS y Android
eBook - ePub
Adoptive Cellular Immunotherapy of Cancer
H. C. Stevenson
Detalles del libro
Vista previa del libro
Índice
Citas
Información del libro
This volume presents the most complicated and powerful cancer biotherapies developed. It provides an overview of human immune system function and the mechanisms by which adoptive cellular immunotherapies (ACI) harnesses the activity. The volume provides a vision on the developments in ACI.
Preguntas frecuentes
¿Cómo cancelo mi suscripción?
¿Cómo descargo los libros?
Por el momento, todos nuestros libros ePub adaptables a dispositivos móviles se pueden descargar a través de la aplicación. La mayor parte de nuestros PDF también se puede descargar y ya estamos trabajando para que el resto también sea descargable. Obtén más información aquí.
¿En qué se diferencian los planes de precios?
Ambos planes te permiten acceder por completo a la biblioteca y a todas las funciones de Perlego. Las únicas diferencias son el precio y el período de suscripción: con el plan anual ahorrarás en torno a un 30 % en comparación con 12 meses de un plan mensual.
¿Qué es Perlego?
Somos un servicio de suscripción de libros de texto en línea que te permite acceder a toda una biblioteca en línea por menos de lo que cuesta un libro al mes. Con más de un millón de libros sobre más de 1000 categorías, ¡tenemos todo lo que necesitas! Obtén más información aquí.
¿Perlego ofrece la función de texto a voz?
Busca el símbolo de lectura en voz alta en tu próximo libro para ver si puedes escucharlo. La herramienta de lectura en voz alta lee el texto en voz alta por ti, resaltando el texto a medida que se lee. Puedes pausarla, acelerarla y ralentizarla. Obtén más información aquí.
¿Es Adoptive Cellular Immunotherapy of Cancer un PDF/ePUB en línea?
Sí, puedes acceder a Adoptive Cellular Immunotherapy of Cancer de H. C. Stevenson en formato PDF o ePUB, así como a otros libros populares de Medicine y Immunology. Tenemos más de un millón de libros disponibles en nuestro catálogo para que explores.
Información
1
Adoptive Cellular Immunotherapy of Cancer: An Overview
National Cancer Institute, Bethesda, Maryland
A variety of distinct strategies to boost the immune system function of the cancer patient in an attempt to treat malignancy have been developed over the past several decades (1–6). It is clear from reviewing the immunological research of the past 100 years that the human immune system is capable of fulfilling its visualized objectives of eliminating nonself invaders from the body; this includes such distinct life forms as viruses, bacteria, and fungi. As will be detailed in this text, compelling evidence has recently been accumulated to indicate that host cells that have undergone malignant transformation not only behave as nonself invaders (attempting to take over the rest of the host), but they also bear chemical markers of malignant transformation (tumor antigens) that allow these cells to be “recognized” by the immune system; such malignantly transformed cells can also be destroyed by host immune system cells. The decade of the 1980s has focused extensively on the development of a new generation of cancer bio-therapies—new immunotherapeutic techniques designed to “up-regulate” human immune system function in an attempt to irradicate malignant cells from cancer patients.
Current biotherapy approaches to cancer treatment are diagramed in Figure 1. From a functional perspective, three different types of bio therapy research strategies are now being explored. One strategy involves the ex vivo manipulation of the cancer patient’s plasma in an effort to remove blocking factors or to add tumoricidal factors to the plasma before the plasma reinfusion. Such therapies usually require a centrifugation separation step to remove plasma from the other blood elements, followed by passage of the plasma over a separate column device such as is employed in staphyloccocal protein A column therapy (7). A more frequently employed biotherapy approach involves the direct in vivo treatment of cancer patients with biological response modifiers (BRM) in an attempt to utilize these agents to directly stimulate the failing immune system within the cancer patient’s body. Such BRM include the interferons (IFN), the interleukins (IL), colony-stimulating factors (CSF), monoclonal antibodies (MAb) and other immunopotentiating agents, such as muramyldipeptide (MDP) and Corynebacterium parvum (C. parvum) (4, 8, 9). (More details about certain of these BRMs will follow in this chapter.) A final functional classification of current biotherapy focuses on the ex vivo activation of cancer patient’s leukocytes with BRM in an attempt to expand their numbers or to increase their antitumor capabilities, or both; this approach has been termed adoptive cellular immunotherapy (ACI). Adoptive cellular immunotherapy is usually initiated with the performance of a cytapheresis procedure to separate the white blood cells (WBC) from the plasma and the red blood cells (RBC); the plasma and RBC are returned to the patient immediately; alternatively, the WBC may be isolated from patient tumor specimens directly. The WBC undergo further processing, including their incubation with BRM designed to augment or to increase their tumor-killing capabilities. These activated WBC are then reinfused back into the patient. The purpose of this volume is to present our current understandings of the mechanics and mechanisms of action of the ACI protocols currently being performed.
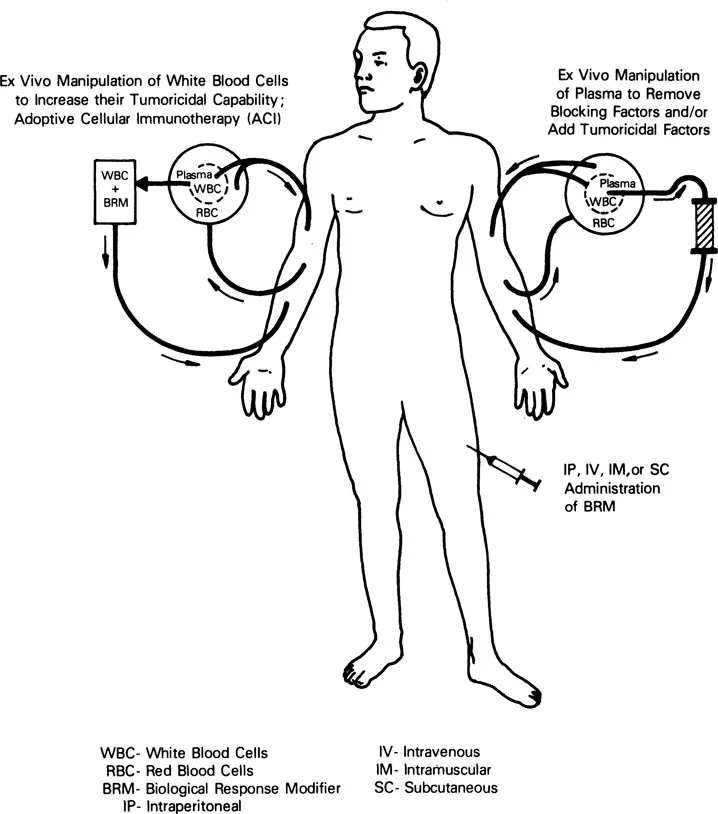
Figure 1 Representation of the functional mechanics involved in the performance of the three major types of cancer bio therapy: (a) Adoptive cellular immunotherapy (ACI), (b) ex vivo manipulation of patient plasma to remove blocking factors or add tumoricidal factors, and (c) in vivo administration of BRM.
THE ANTITUMOR ACTIVITIES OF THE HUMAN IMMUNE SYSTEM
Within the past two decades, we have gleaned many insights into the overall operation of the human immune system and the potential applicability of this system to the treatment of cancer. As shown in Figure 2, the immune system mechanisms that are felt to be operative in the elimination of tumor cells from the body are rather straightforward. There are four basic cell types whose function has been associated with antitumor cell immunity. The B-lymphocytes secrete protein factors [immunoglobulins (Ig)] into the blood plasma, which have the capability of identifying and binding to targets that bear specific molecular markers that they can recognize. From a functional perspective, each individual possesses enough different types (clones) of B lymphocytes (and thus enough different Ig types) to identify most nonself invaders; this specific component of humoral (plasma-borne) immunity is a potent mechanism for identifying and labeling nonself invaders. It is noteworthy, however, that Ig-labeled target cells, in and of themselves, perform in a relatively unimpeded fashion; that is, additional factors are required for Ig-coated targets (such as tumor cells) to be destroyed. The two dominant mechanisms whereby Ig-coated targets are cleared from the body are through the complement cascade (the nonspecific component of humoral immunity) and the antibody-dependent cell-mediated cytotoxicity (ADCC) mechanisms (cellular mechanisms reviewed below). The complement proteins are a series of proteins that exist in an inactive state in the blood plasma under normal conditions. However, upon encountering an immunoglobulin (IgG or IgM)-coated target, these plasma proteins assemble into a trocarlike mechanism that is capable of lysing nonself invader cells (including tumor cells). The complement proteins are chiefly secreted by the mononuclear phagocyte series (blood monocytes). Since the advent of MAb technology (4), great attention has been focused on the protein products of B lymphocytes and the application of these Ig proteins to the treatment of cancer. For this reason, neither the Ig proteins nor their cellular factories (the B lymphocytes) will be discussed further in this volume, except to mention that the B lymphocytes are subject to activation and regulation by a variety of protein signal molecules—the BRM-chemotherapy agents, and other chemicals that can influence their function. These modulating agents will be reviewed relative to the other leukocyte subsets that participate in the overall immune response to cancer.
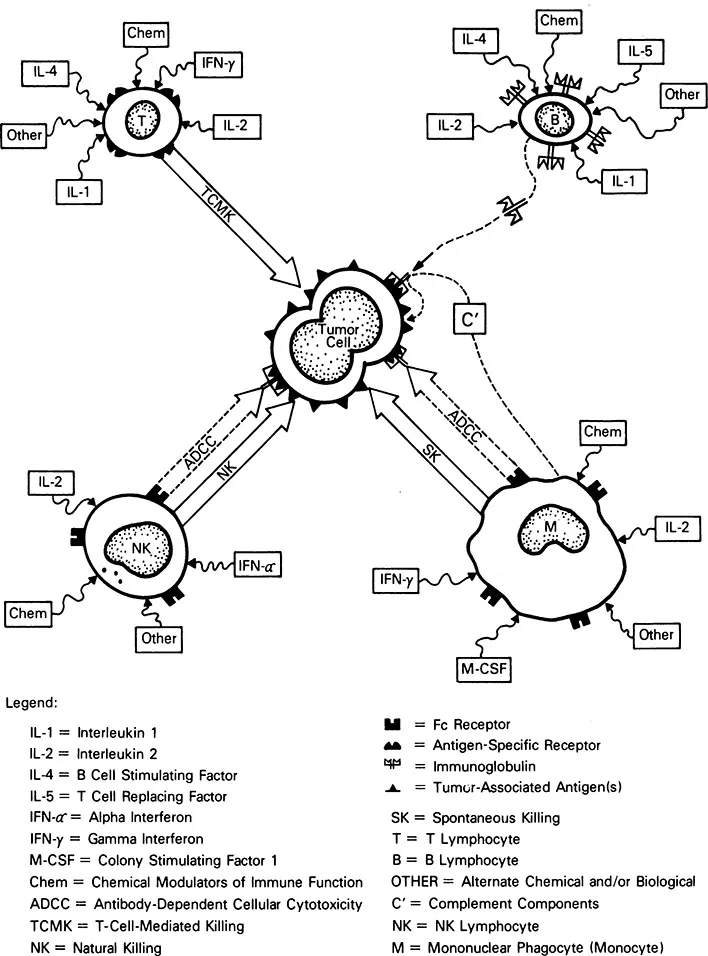
Figure 2 Representation of the potential mechanisms of action whereby B, T, and NK lymphocytes and mononuclear phagocytes (monocytes and macrophages) may eliminate tumor cells.
The two remaining lymphocyte subsets have been harnessed for ACI. They are the natural killer (NK) lymphocytes and the T lymphocytes. The T lymphocytes exist in clones as do the B lymphocytes; in contrast with B lymphocytes, they do not function by synthesizing proteins for transport through the blood stream to mediate tumor cell killing but, rather, they physically travel to the site of tumor cell invasion and locally arrange for the destruction of the tumor cells. As shown in Figure 2, T lymphocytes possess antigen-specific receptors, and each T-lymphocyte clone has the capacity to recognize (and potentially destroy) a tumor cell carrying complementary marker molecules on its membrane (tumor-associated antigens). Given the total spectrum of T-lymphocyte clones present in the body, it appears that each individual possesses the total range of T-lymphocyte clones required to eliminate most types of tumor cells (1). The T lymphocytes destroy tumor cells through their antigen-specific receptors. Such killing is termed T-cell-mediated killing (TCMK) and is antigen-specific; that is, each T-lymphocyte clone can eliminate only a very narrowly related group of tumor cells bearing the same tumor-associated antigen. Moreover, TCMK by T lymphocytes is restricted by the major histocompatibility (MHC) molecules; that is, tumor cell killing by T-lymphocyte clones requires identity between the MHC molecules found on the surface of the tumor cell and specific MHC receptors found on the surface of the T lymphocyte. T-cell-mediated killing can be modulated by a variety of influences. These include many BRMs, such as interleukin-1 (IL-1), interleukin-2 (IL-2) and interleukin-4 (IL-4), and inter-feron-γ (IFN-γ) (reviewed later), as well as chemotherapy agents and other chemicals. Some researchers believe that tumor-infiltrating lymphocyte (TIL) therapy is mediated by activated antigen-specific T-lymphocyte clones; however, this particular ACI topic is the subject of a substantial amount of controversy that is excellently summarized in Chapter 9. The developers of the tumor-derived activated cell (TDAC) therapy believe that they infuse activated antigen-specific T lymphocytes into their patients as reviewed in Chapter 10.
The natural killer (NK) lymphocyte is the third well-characterized lymphocyte subset that has antitumor cell reactivity. In contrast with the T lymphocyte, the NK lymphocyte bears no evidence of clonality; that is, a single type of cell appears to be capable of destroying a wide range of human tumors. This large-volume lymphocyte subset has distinctive granules in its cytoplasm and also has been termed the large granular lymphocyte (LGL; 10, 11). Natural killer lymphocytes have two distinct mechanisms for the destruction of tumor cells. One is a mechanism known as antibody-dependent cellular cytotoxicity (ADCC). This cytotoxicity occurs when special membrane receptors (Fc receptors) on the surface on the NK lymphocyte bind to the terminal (Fc) portion of Ig molecules (IgG) that have bound to the tumor-associated antigens found on the surface of tumor cells. The Ig molecule then functions as a ligand between the NK lymphocyte and the tumor cell and promotes the rapid destruction of the tumor cell. Alternatively, NK lymphocytes can kill tumor cells independent of Ig; this killing is termed natural killing (NK). The precise molecular marker that promotes natural killing is not now known; however, it appears to be a glycolipid molecule (ganglioside) that appears on virtually all malignantly transformed cells. The baseline natural-killing capability of NK cells can be upregulated by a variety of BRM including interferon-α (IFN-a) and IL-2 (reviewed later); it can also be modulated by chemotherapy agents and other chemicals. The lymphokine-activated killer lymphocyte (LAK) can be generated by upregulating the tumoricidal activity of NK lymphocytes by the in vitro incubation of this cell type with the BRM, IL-2; however other LAK precursor cells may exist. This issue is addressed in Chapter 2.
The third subset of WBC that can be harnessed for ACI trials is not a lymphocyte, but rather is from the mononuclear phagocyte series, chiefly in the form of blood monocytes. Like the NK lymphocytes, monocytes possess two independent mechanisms for destroying tumor targets. Mon...