![]()
Buchfelder M, Guaraldi F (eds): Imaging in Endocrine Disorders.
Front Horm Res. Basel, Karger, 2016, vol 45, pp 80-96 (DOI: 10.1159/000442319)
______________________
Gonadal Imaging in Endocrine Disorders
Fabio Lanfranco · Giovanna Motta
Divisione di Endocrinologia, Diabetologia e Metabolismo, Dipartimento di Scienze Mediche, Università di Torino, Turin, Italy
______________________
Abstract
Ultrasound (US) is the most widely available method of diagnostic imaging for the evaluation and characterization of gonadal lesions and is usually the method of choice because of its high accuracy, low cost and wide availability. Today’ s high-resolution images allow for a confident diagnosis of many scrotal and adnexal lesions, with high sensitivity and specificity. Magnetic resonance imaging (MRI) is reliable in the detection of gonadal lesions in males, allowing the differentiation into testicular or nontesticular lesions, and their characterization. It is also an accurate and cost-effective diagnostic adjunct in those patients with solid scrotal lesions for whom the findings of clinical and US evaluations are inconclusive. In females, MRI is recommended as a second-line investigation for the characterization of complex adnexal masses that are indeterminate on US. In this review, gonadal pathologies related with the steroidogenic and gametogenic function of the testes and ovaries will be discussed. The main imaging features of benign and malignant lesions will also be presented.
© 2016 S. Karger AG, Basel
Male Gonads
Introduction
Scrotal ultrasound (US) is the most widely available method of diagnostic imaging and is usually the method of choice for examining the scrotum because of its high accuracy, excellent anatomic depiction, low cost and wide availability [1, 2]. Recent technical advances of US applications and postprocessing developments have enabled new aspects in the structural and functional analysis of testicular tissue and can suggest a specific diagnosis for a wide variety of testicular diseases [3].
Magnetic resonance imaging (MRI) is reliable in the detection of scrotal lesions, allowing the differentiation into testicular or nontesticular lesions and their characterization, including cysts and fluid, solid masses, fat and fibrosis [4]. MRI is an accurate and cost-effective diagnostic adjunct in those patients with solid scrotal lesions for whom the findings from clinical and US evaluations are inconclusive [5].
CT (computed tomography) scan is not commonly used in testis imaging because it involves ionizing radiation and because it is expensive. However, it can play an important role in testis cancer staging and in cryptorchidism in order to localize undescended testes [6].
In this section, scrotal pathologies related with the steroidogenic and spermatogenic functions of the testes will be discussed. For a more comprehensive overview of other benign and malignant testicular or extratesticular scrotal lesions the reader is referred to recent reviews such as those by Appelbaum et al. [2], and Pearl and Hill [7].
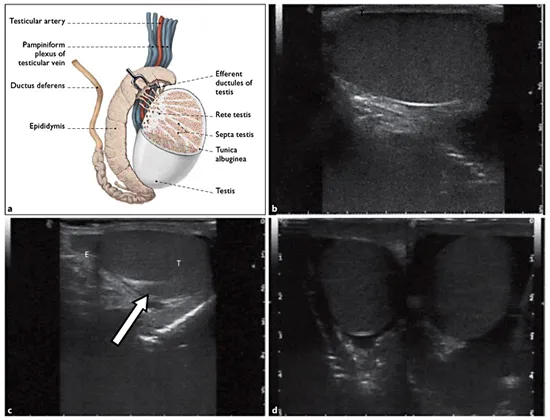
Fig. 1. a Sagittal view of the normal anatomy of the testicle, epididymis and mediastinum testis; reproduced with permission from Köpf-Maier [44]. Transverse (b) and longitudinal (c) US images showing a normal testis (T), epididymis (E) and mediastinum testis (arrow). d Transverse view of both testes for comparison of size, shape and echogenicity.
Normal Anatomy of the Scrotum
The normal postpubertal testes are symmetric and ovoid, and measure approximately 5 × 3 × 2 cm (fig. 1a). On US examination, the testis usually has medium level homogeneous echoes (fig. 1b-d), although normal variants have been described and include a unilateral striated pattern, thought to represent fibrosis (fig. 2), or hypoechoic intratesticular bands in the middle third of the testis which may contain arterial and venous components and represent a normal variant of intratesticular vessels. The fibrous tunica albuginea, which surrounds the testis, can be seen as a thin echogenic line [7].
The epididymis is a 6- to 7-cm tubular structure that normally courses inferiorly along the posterior aspect of the testis and is composed of a head, body and tail. The epididymal head measures 5-12 mm in diameter, is located at the superior pole of the testis and is round, triangular or pyramidal in shape [7, 8]. The body and tail are narrower, measuring 2-5 mm in diameter [8], and gradually taper as they course inferiorly along the testis to its lower pole (fig. 1a).
Testicular flow is supplied primarily by the testicular arteries, which arise from the aorta distal to the renal artery, course through the inguinal canal along the spermatic cord and reach the upper pole of the testes to divide into capsular arteries [2] (fig. 1a). On color Doppler US (CDUS) normal testicular tissue shows a typical stellar vascular pattern [3].
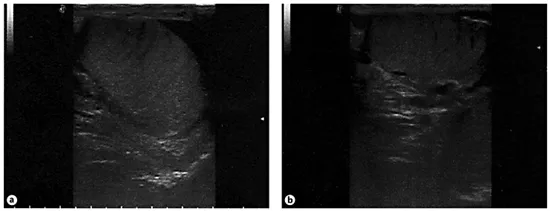
Fig. 2. Longitudinal (a) and transverse (b) US scans of a normal striated testis.
The epididymis and the extratesticular tissues are supplied by the deferential and cremasteric arteries. Venous drainage is accomplished by the pampiniform plexus, which drains into the ipsilateral testicular vein and subsequently into the inferior vena cava on the right or the renal vein on the left testis (fig. 1a).
Scrotal Ultrasound: Technique of Examination
The patient lays supine with the scrotal sac supported by a draped towel over the thighs and the penis covered with a towel over the pubis. A large amount of gel is applied over the scrotal sac [2]. For structural analysis mainly grayscale or B-mode US with a high-resolution, near-focused, linear-array transducer with a frequency of 7.5-14 MHz or greater is used. Bilateral transverse and longitudinal slices of the scrotum and inguinal region are performed to allow side-to-side comparison of their sizes and echo texture [3]. Any intratesticular or extratesticular finding should be imaged and measured in different planes [2].
Grayscale US is mainly used for the measurement of testicular volume and for estimation of tissue texture based on alterations in echogenicity. This technique demonstrates the alteration of size and echogenicity in an atrophic testis as well as alteration of echogenicity in a testis with partial infarction or ischemia in comparison to normal testicular tissue. A slightly impaired echo texture indicates a decreased testicular function. Testicular volume in infertile men is related to semen profiles. Up to 70-80% of the testicular volume consists of the seminiferous tubules and reflects spermatogenesis [3]. A strong correlation between testicular function and testicular volume measured by US or other techniques has been proven by Sakamoto et al. [9]. For further functional analysis the native or unenhanced CDUS, the contrast-enhanced CDUS and the advanced contrast agent detection techniques like MVI (microvessel imaging, Philips) and the calculation of TIC (time intensity curve) are implemented [3].
Unenhanced CDUS is well established to illustrate macrovascularity and therefore perfusion. Testicular perfusion can be evaluated with color Doppler, power Doppler and spectral Doppler US [3]. CDUS and power Doppler US represent a promising method for the assessment of patients affected by azoospermia by allowing the discrimination of obstructive azoospermia (normal vessel distribution) from nonobstructive azoospermia (reduced or absent testicular vessels) [3].
Contrast-enhanced US (CEUS) can be used for the illustration of macrovascularity and microvascularity. For this, micro bubbles with a lipid or galactose shell filled with an inert gas and a diameter of 7-10 μm are administered intravenously. These microbubbles can be used as an echo enhancer for CDUS leading to a visualization of blood flow also in the microvessels [3]. Thierman et al. [10] found out that CEUS is potentially applicable to the investigation of vascular disorders of the testis. The use of a pulse inve...