
eBook - ePub
Blood Cells
A Practical Guide
Barbara J. Bain
This is a test
Partager le livre
- English
- ePUB (adapté aux mobiles)
- Disponible sur iOS et Android
eBook - ePub
Blood Cells
A Practical Guide
Barbara J. Bain
Détails du livre
Aperçu du livre
Table des matières
Citations
À propos de ce livre
- Enables both the haematologist and laboratory scientist to identify blood cell features, from the most common to the more obscure
- Provides essential information on methods of collection, blood film preparation and staining, together with the principles of manual and automated blood counts
- Completely revised and updated, incorporating much newly published information: now includes advice on further tests when a specific diagnosis is suspected
- 400 high quality photographs to aid with blood cell identification
- Highlights the purpose and clinical relevance of haematology laboratory tests throughout
Foire aux questions
Comment puis-je résilier mon abonnement ?
Il vous suffit de vous rendre dans la section compte dans paramètres et de cliquer sur « Résilier l’abonnement ». C’est aussi simple que cela ! Une fois que vous aurez résilié votre abonnement, il restera actif pour le reste de la période pour laquelle vous avez payé. Découvrez-en plus ici.
Puis-je / comment puis-je télécharger des livres ?
Pour le moment, tous nos livres en format ePub adaptés aux mobiles peuvent être téléchargés via l’application. La plupart de nos PDF sont également disponibles en téléchargement et les autres seront téléchargeables très prochainement. Découvrez-en plus ici.
Quelle est la différence entre les formules tarifaires ?
Les deux abonnements vous donnent un accès complet à la bibliothèque et à toutes les fonctionnalités de Perlego. Les seules différences sont les tarifs ainsi que la période d’abonnement : avec l’abonnement annuel, vous économiserez environ 30 % par rapport à 12 mois d’abonnement mensuel.
Qu’est-ce que Perlego ?
Nous sommes un service d’abonnement à des ouvrages universitaires en ligne, où vous pouvez accéder à toute une bibliothèque pour un prix inférieur à celui d’un seul livre par mois. Avec plus d’un million de livres sur plus de 1 000 sujets, nous avons ce qu’il vous faut ! Découvrez-en plus ici.
Prenez-vous en charge la synthèse vocale ?
Recherchez le symbole Écouter sur votre prochain livre pour voir si vous pouvez l’écouter. L’outil Écouter lit le texte à haute voix pour vous, en surlignant le passage qui est en cours de lecture. Vous pouvez le mettre sur pause, l’accélérer ou le ralentir. Découvrez-en plus ici.
Est-ce que Blood Cells est un PDF/ePUB en ligne ?
Oui, vous pouvez accéder à Blood Cells par Barbara J. Bain en format PDF et/ou ePUB ainsi qu’à d’autres livres populaires dans Medicina et Hematología. Nous disposons de plus d’un million d’ouvrages à découvrir dans notre catalogue.
Informations
CHAPTER 1
Blood sampling and blood film preparation and examination
Obtaining a blood specimen
Performing an accurate blood count and correctly interpreting a blood film require that an appropriate sample from the patient, mixed with the correct amount of a suitable anticoagulant, is delivered to the laboratory without undue delay. No artefacts should be introduced during these procedures.
The identity of the patient requiring blood sampling should be carefully checked before performing a venepuncture. This is usually done by requesting the patient to state surname, given name and date of birth and, for hospital inpatients, by checking a wristband to verify these details and, in addition, the hospital number. To reduce the chance of human error, bottles should not be labelled in advance. The person performing the phlebotomy must conform to local guidelines, including those for patient identification. Although traditionally more attention has been given to patient identification in relation to blood transfusion, it should be noted that wrong treatment has also followed the misidentification of patients from whom samples are taken for a blood count and identification must also be taken seriously in this field. More secure identification of inpatients can be achieved by the use of electronic devices in which the patient’s identity is scanned in from a bar-coded wristband by means of a hand-held device.
Patients should either sit or lie comfortably and should be reassured that the procedure causes only minimal discomfort; they should not be told that venepuncture is painless, since this is not so. It is preferable for apprehensive patients to lie down. Chairs used for venepuncture should preferably have adjustable armrests so that the arm can be carefully positioned. Armrests also help to ensure patient safety, since they make it harder for a fainting patient to fall from the chair. I have personally observed one patient who sustained a skull fracture when he fainted at the end of a venepuncture and fell forward onto a hard floor, and two other patients, neither previously known to be epileptic, who suffered epileptiform convulsions during venepuncture. Such seizures may not be true epilepsy, but consequent on hypoxia following brief vagal-induced cessation of heart beat [1]. If venepunctures are being performed on children or on patients unable to cooperate fully, then the arm for venepuncture should be gently but firmly immobilized by an assistant. Gloves should be worn during venepuncture, for the protection of the person carrying out the procedure. Non-latex gloves must be available if either the phlebotomist or the patient is allergic to latex. The needle to enter the patient must not be touched, so that it remains sterile.
In some circumstances, the patient should rest prior to venesection. In endurance athletes being tested for a ‘biological passport’, 10 minutes’ rest in a seated position has been found to be sufficient for the haemoglobin concentration (Hb) and haematocrit (Hct) to fall to a stable level [2].
Peripheral venous blood
In an adult, peripheral venous blood is most easily obtained from a vein in the antecubital fossa (Fig. 1.1) using a needle and either a syringe or an evacuated tube. Of the veins in the antecubital region, the median cubital vein is preferred since it is usually large and well anchored in tissues, but the cephalic and basilic veins are also often satisfactory. Other forearm veins can be used, but they are frequently more mobile and therefore more difficult to penetrate. Veins on the dorsum of the wrist and hand often have a poorer flow and performing venepuncture at these sites is more likely to lead to bruising. This is also true of the anterior surface of the wrist where, in addition, venepuncture tends to be more painful and where there is more risk of damaging vital structures. Foot veins are not an ideal site for venepuncture and it is rarely necessary to use them. Injuries that have been associated with obtaining a blood sample from the antecubital fossa include damage to the lateral antebrachial cutaneous nerve [3] and inadvertent arterial puncture. Complications are more likely with the less accessible basilic vein than with the median antecubital or the cephalic vein. If anterior wrist veins have to be used, there is a risk of damage to the radial or ulnar nerve or artery. Use of foot veins is more likely to lead to complications, e.g. thrombosis, infection or poor healing.
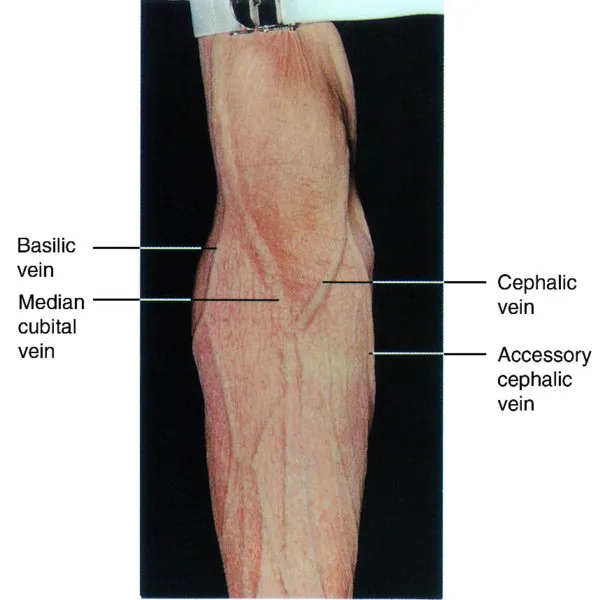
Fig. 1.1 Anterior surface of the left arm showing veins most suitable for venepuncture.
When a vein is identified it is palpated to ensure it is patent. A patent vein is soft and can be compressed easily. A thrombosed vein feels cord-like and is not compressible. An artery has a thicker wall and is pulsatile. If a vein is not visible (in some dark-skinned or overweight people) it is identified by palpation after applying a tourniquet to achieve venous distension. If veins appear very small, warming of the arm to produce vasodilatation helps, as does tapping the vein and asking the patient to clench and unclench the fist several times.
It should be noted that pathogenic bacteria can be cultured from reusable tourniquets and it is prudent practice to use disposable tourniquets, at least for patients at particular risk of infection [4].
The arm should be positioned on the armrest so that the vein identified is under some tension and its mobility is reduced. The skin should be cleaned with 70% ethanol or 0.5% chlorhexidine and allowed to dry, to avoid stinging when the skin is penetrated. A tourniquet is applied to the arm, sufficiently tightly to distend the vein, but not so tightly that discomfort is caused. Alternatively, a sphygmomanometer cuff can be applied and inflated to diastolic pressure, but the use of a tourniquet is usually quicker and simpler. If it is particularly important to obtain a specimen without causing haemoconcentration, e.g. in a patient with suspected polycythaemia, the tourniquet should be left on the arm only long enough to allow penetration of the vein. Otherwise it can be left applied while blood is being obtained, to ensure a continuing adequate flow of blood. It is preferable that the tourniquet is applied for no more than a minute, but the degree of haemoconcentration may not be great, even after 10 minutes’ application. In one study the increase of the Hb and the red blood cell count (RBC) was about 2% at 2 and at 10 minutes [5]. However, in another study Hb rose by 9 g/l by 3 minutes and RBC and Hct by a corresponding amount [6].
Blood specimens can be obtained with a needle and an evacuated tube (see below) or with either a needle or a winged blood collection cannula (a ‘butterfly’) and a syringe. A winged cannula may reduce the chance of injury to nerves [7] and is certainly preferable for small veins and difficult sites. A 19 or 20 gauge needle is suitable for an adult and a 21 or 23 gauge for a child or an adult with small veins. When using a syringe, the plunger should first be moved within the barrel of the syringe to ensure that it will move freely. Next the needle is attached to the syringe, which, unless small, should have a side port rather than a central port. The guard is then removed. The needle is now inserted into the vein with the bevel facing upwards (Fig. 1.2). This may be done in a single movement or in two separate movements for the skin and the vein, depending on personal preference and on how superficial the vein is. With one hand steadying the barrel of the syr...