
eBook - ePub
Pocket On Call
Andrew Stewart
This is a test
Condividi libro
- 151 pagine
- English
- ePUB (disponibile sull'app)
- Disponibile su iOS e Android
eBook - ePub
Pocket On Call
Andrew Stewart
Dettagli del libro
Anteprima del libro
Indice dei contenuti
Citazioni
Informazioni sul libro
This genuinely pocket-sized guide to being on call is ideal for medical students and newly qualified junior doctors seeking a convenient and concise handbook to refer to in busy clinical settings. Clear, concise and systematic, Pocket on Call contains exactly what you need to make rapid and appropriate decisions without overwhelming or extrane
Domande frequenti
Come faccio ad annullare l'abbonamento?
È semplicissimo: basta accedere alla sezione Account nelle Impostazioni e cliccare su "Annulla abbonamento". Dopo la cancellazione, l'abbonamento rimarrà attivo per il periodo rimanente già pagato. Per maggiori informazioni, clicca qui
È possibile scaricare libri? Se sì, come?
Al momento è possibile scaricare tramite l'app tutti i nostri libri ePub mobile-friendly. Anche la maggior parte dei nostri PDF è scaricabile e stiamo lavorando per rendere disponibile quanto prima il download di tutti gli altri file. Per maggiori informazioni, clicca qui
Che differenza c'è tra i piani?
Entrambi i piani ti danno accesso illimitato alla libreria e a tutte le funzionalità di Perlego. Le uniche differenze sono il prezzo e il periodo di abbonamento: con il piano annuale risparmierai circa il 30% rispetto a 12 rate con quello mensile.
Cos'è Perlego?
Perlego è un servizio di abbonamento a testi accademici, che ti permette di accedere a un'intera libreria online a un prezzo inferiore rispetto a quello che pagheresti per acquistare un singolo libro al mese. Con oltre 1 milione di testi suddivisi in più di 1.000 categorie, troverai sicuramente ciò che fa per te! Per maggiori informazioni, clicca qui.
Perlego supporta la sintesi vocale?
Cerca l'icona Sintesi vocale nel prossimo libro che leggerai per verificare se è possibile riprodurre l'audio. Questo strumento permette di leggere il testo a voce alta, evidenziandolo man mano che la lettura procede. Puoi aumentare o diminuire la velocità della sintesi vocale, oppure sospendere la riproduzione. Per maggiori informazioni, clicca qui.
Pocket On Call è disponibile online in formato PDF/ePub?
Sì, puoi accedere a Pocket On Call di Andrew Stewart in formato PDF e/o ePub, così come ad altri libri molto apprezzati nelle sezioni relative a Medicine e Public Health, Administration & Care. Scopri oltre 1 milione di libri disponibili nel nostro catalogo.
Informazioni
Section B
Acutely unwell patients
Being alerted to unwell patients
During on-call shifts, acutely unwell patients may be brought to your attention in a number of ways.
Handover: The structure of this will vary between hospitals. Typically, there will be a ‘handover’ from the day teams at the end of a normal working day. Any outstanding jobs or patients who have been particularly unwell during the day will be handed over to the on-call ‘cover’ team. This may be via an electronic computer-based system or by verbal communication.
Emergency buzzers: These are usually activated by pulling an ominous red button which can be found attached to the wall in most bed spaces. Their appearance will vary between hospitals, and it is worth familiarizing yourself with what they look (and sound) like in your hospital.
Cardiac arrest bleep: In most hospitals the cardiac arrest team consists of the on-call medical team, the on-call anaesthetist, and sometimes a senior nurse from the cardiac care unit (CCU) or the emergency department (ED). The bleep tone is usually faster and prolonged and is followed by a speech message alerting you to the location of the arrest.
Fast bleep: These pages are received when a doctor is required urgently and will usually sound similar to the cardiac arrest bleep.
Early warning scores: Most hospitals now operate early warning score (EWS) systems as a means of rapidly identifying deteriorating patients. Every time nursing staff record clinical observations (OBS) a total score is generated based on whether the numbers are within or stray outside of set physiological parameters. Abnormal observations will generate a number; the more abnormal the physiology, the higher the number. Depending on the score generated, the nursing staff will request a medical review within a designated time frame. The following illustrates an example of a typical early warning score.
The National Early Warning System (NEWS)
The NEWS system is a new early warning tool produced in collaboration with the Royal Colleges of Physicians and Nursing and the National Outreach Forum. It is set to become the gold standard across the country. The diagram on page 11, reprinted with permission from the Royal College of Physicians, displays the NEWS system as it would appear on the back of the observation chart.
‘Doctor, the patient’s NEWS is …’
This is a very common bleep from nursing staff, particularly during on-call shifts and out of hours. Consider asking the following over the phone before setting off to assess the patient:
• Score break down: Ask for the individual observations (OBS) (gives you an idea of what you are going to).
• Ask about trends: What is the patient’s usual blood pressure (BP), heart rate (HR), etc.
• Why is the patient in the hospital? Working diagnosis?
• Any specific symptoms? Chest pain, shortness of breath (SOB), palpitations, etc.
• Past medical history (PMHx).
Remember: Depending on the situation, it may be possible to delegate certain tasks to nursing staff before you arrive (e.g. starting oxygen, repeating OBS); this can speed things up in an acute situation.
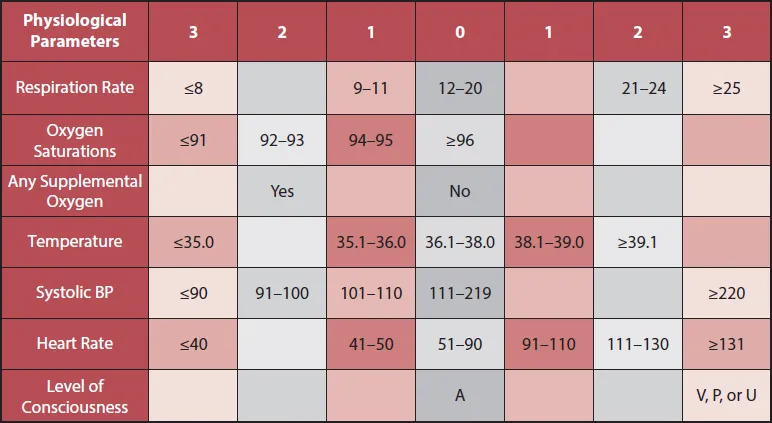
* The NEWS initiative flowed from the Royal College of Physicians’ NEWSDIG, and was jointly developed and funded in collaboration with the Royal College of Physicians, Royal College of Nursing, National Outreach Forum and NHS Training for Innovation.
Remembering the alphabet … the ‘A, B, C, D, E’ assessment
Rather conveniently, the first five letters of the alphabet also lay out the crucial five stages of the initial emergency assessment, or A, B, C, D, E examination. This is a well-established system used to rapidly examine and optimize any acutely unwell patient.
The basic principle is to assess each step in order, correcting any abnormality as soon as it is identified. Each and every patient you are called to see should receive an initial assessment using this systematic approach.
The basis of this is logical – in any acute situation, the overall emphasis is to ensure optimal oxygen delivery at the cellular level, in addition to correcting the underlying pathology. To achieve this you must have:
1. A patent, unobstructed airway (A).
2. Efficient gas exchange at the alveolar – capillary membrane (B).
3. An intact cardiovascular system to perfuse the lungs and carry oxygenated blood to tissues (C).
Step D stands for disability, and represents a focused neurological assessment.
Step E stands for exposure – a general top-to-toe assessment including factors such as body temperature, abdominal examination, and blood glucose measurement. (Remember: Hypoglycaemia is a common cause of reduced Glasgow Coma Score (GCS) and is easily correctable.)
Your initial assessment will no doubt vary a little depending on the particular circumstances, but it is useful to consider the ‘ideal’ A, B, C, D, E assessment as a starting point.
The A, B, C, D, E assessment – in practice
It should be stressed this is different from the standard examination that accompanies a full medical clerking. The A, B, C, D, E approach is used in the context of the acutely unwell patient. The following provides a practical approach:
A – airway
Observe and speak to the patient: Is he or she maintaining his or her airway?
Optimize as appropriate using:
Airway manoeuvres – head tilt, chin lift, jaw thrust.
Airway adjuncts – oropharyngeal/nasal airway.
Suction of oropharynx if required.
Airway manoeuvres – head tilt, chin lift, jaw thrust.
Airway adjuncts – oropharyngeal/nasal airway.
Suction of oropharynx if required.
B – breathing
Measure respiratory rate + assess breathing pattern.
Note position of trachea.
Auscultate the chest + expansion/resonance.
Attach pulse oximeter + consider arterial blood gas (ABG) if indicated.
Commence interventions as appropriate – oxygen, nebulizer, etc.
C – circulation
Pulse – assess rate, rhythm, and volume.
Measure BP.
Consider attaching heart monitor.
Central capillary refill time.
Auscultate praecordium.
Secure IV access + bloods + IV fluids as appropriate.
12-lead ECG if indicated.
If catheterized, measure urine output.
D – disability
Assess pupils.
Observe limb movement for reduced power/asymmetry.
GCS assessment.
Babinski/plantar reflex.
E – exposure
Measure core body temperature.
Abdominal examination.
Examine the calves for swelling, pain, asymmetry (think about deep vein thrombosis (DVT)).
Check glucose (don’t forget the mantra ‘never ever forget glucose’).
Note any other stigmata of disease.
A note about the...