- 151 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Pocket On Call
About this book
This genuinely pocket-sized guide to being on call is ideal for medical students and newly qualified junior doctors seeking a convenient and concise handbook to refer to in busy clinical settings. Clear, concise and systematic, Pocket on Call contains exactly what you need to make rapid and appropriate decisions without overwhelming or extrane
Tools to learn more effectively

Saving Books

Keyword Search

Annotating Text

Listen to it instead
Information
Topic
MedicineSubtopic
Internal Medicine & DiagnosisSection B
Acutely unwell patients
Being alerted to unwell patients
During on-call shifts, acutely unwell patients may be brought to your attention in a number of ways.
Handover: The structure of this will vary between hospitals. Typically, there will be a ‘handover’ from the day teams at the end of a normal working day. Any outstanding jobs or patients who have been particularly unwell during the day will be handed over to the on-call ‘cover’ team. This may be via an electronic computer-based system or by verbal communication.
Emergency buzzers: These are usually activated by pulling an ominous red button which can be found attached to the wall in most bed spaces. Their appearance will vary between hospitals, and it is worth familiarizing yourself with what they look (and sound) like in your hospital.
Cardiac arrest bleep: In most hospitals the cardiac arrest team consists of the on-call medical team, the on-call anaesthetist, and sometimes a senior nurse from the cardiac care unit (CCU) or the emergency department (ED). The bleep tone is usually faster and prolonged and is followed by a speech message alerting you to the location of the arrest.
Fast bleep: These pages are received when a doctor is required urgently and will usually sound similar to the cardiac arrest bleep.
Early warning scores: Most hospitals now operate early warning score (EWS) systems as a means of rapidly identifying deteriorating patients. Every time nursing staff record clinical observations (OBS) a total score is generated based on whether the numbers are within or stray outside of set physiological parameters. Abnormal observations will generate a number; the more abnormal the physiology, the higher the number. Depending on the score generated, the nursing staff will request a medical review within a designated time frame. The following illustrates an example of a typical early warning score.
The National Early Warning System (NEWS)
The NEWS system is a new early warning tool produced in collaboration with the Royal Colleges of Physicians and Nursing and the National Outreach Forum. It is set to become the gold standard across the country. The diagram on page 11, reprinted with permission from the Royal College of Physicians, displays the NEWS system as it would appear on the back of the observation chart.
‘Doctor, the patient’s NEWS is …’
This is a very common bleep from nursing staff, particularly during on-call shifts and out of hours. Consider asking the following over the phone before setting off to assess the patient:
• Score break down: Ask for the individual observations (OBS) (gives you an idea of what you are going to).
• Ask about trends: What is the patient’s usual blood pressure (BP), heart rate (HR), etc.
• Why is the patient in the hospital? Working diagnosis?
• Any specific symptoms? Chest pain, shortness of breath (SOB), palpitations, etc.
• Past medical history (PMHx).
Remember: Depending on the situation, it may be possible to delegate certain tasks to nursing staff before you arrive (e.g. starting oxygen, repeating OBS); this can speed things up in an acute situation.
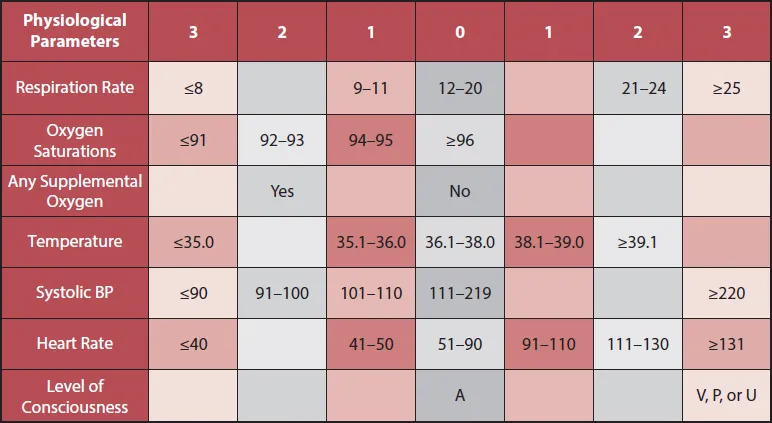
* The NEWS initiative flowed from the Royal College of Physicians’ NEWSDIG, and was jointly developed and funded in collaboration with the Royal College of Physicians, Royal College of Nursing, National Outreach Forum and NHS Training for Innovation.
Remembering the alphabet … the ‘A, B, C, D, E’ assessment
Rather conveniently, the first five letters of the alphabet also lay out the crucial five stages of the initial emergency assessment, or A, B, C, D, E examination. This is a well-established system used to rapidly examine and optimize any acutely unwell patient.
The basic principle is to assess each step in order, correcting any abnormality as soon as it is identified. Each and every patient you are called to see should receive an initial assessment using this systematic approach.
The basis of this is logical – in any acute situation, the overall emphasis is to ensure optimal oxygen delivery at the cellular level, in addition to correcting the underlying pathology. To achieve this you must have:
1. A patent, unobstructed airway (A).
2. Efficient gas exchange at the alveolar – capillary membrane (B).
3. An intact cardiovascular system to perfuse the lungs and carry oxygenated blood to tissues (C).
Step D stands for disability, and represents a focused neurological assessment.
Step E stands for exposure – a general top-to-toe assessment including factors such as body temperature, abdominal examination, and blood glucose measurement. (Remember: Hypoglycaemia is a common cause of reduced Glasgow Coma Score (GCS) and is easily correctable.)
Your initial assessment will no doubt vary a little depending on the particular circumstances, but it is useful to consider the ‘ideal’ A, B, C, D, E assessment as a starting point.
The A, B, C, D, E assessment – in practice
It should be stressed this is different from the standard examination that accompanies a full medical clerking. The A, B, C, D, E approach is used in the context of the acutely unwell patient. The following provides a practical approach:
A – airway
Observe and speak to the patient: Is he or she maintaining his or her airway?
Optimize as appropriate using:
Airway manoeuvres – head tilt, chin lift, jaw thrust.
Airway adjuncts – oropharyngeal/nasal airway.
Suction of oropharynx if required.
Airway manoeuvres – head tilt, chin lift, jaw thrust.
Airway adjuncts – oropharyngeal/nasal airway.
Suction of oropharynx if required.
B – breathing
Measure respiratory rate + assess breathing pattern.
Note position of trachea.
Auscultate the chest + expansion/resonance.
Attach pulse oximeter + consider arterial blood gas (ABG) if indicated.
Commence interventions as appropriate – oxygen, nebulizer, etc.
C – circulation
Pulse – assess rate, rhythm, and volume.
Measure BP.
Consider attaching heart monitor.
Central capillary refill time.
Auscultate praecordium.
Secure IV access + bloods + IV fluids as appropriate.
12-lead ECG if indicated.
If catheterized, measure urine output.
D – disability
Assess pupils.
Observe limb movement for reduced power/asymmetry.
GCS assessment.
Babinski/plantar reflex.
E – exposure
Measure core body temperature.
Abdominal examination.
Examine the calves for swelling, pain, asymmetry (think about deep vein thrombosis (DVT)).
Check glucose (don’t forget the mantra ‘never ever forget glucose’).
Note any other stigmata of disease.
A note about the...
Table of contents
- Cover
- Half Title
- Title Page
- Copyright Page
- Dedication
- Table of Contents
- Foreword
- Section A ‘Getting set’
- Section B Acutely unwell patients
- Section C Situations and communication
- Section D Prescribing
- Bibliography
- Index
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn how to download books offline
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 990+ topics, we’ve got you covered! Learn about our mission
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more about Read Aloud
Yes! You can use the Perlego app on both iOS and Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app
Yes, you can access Pocket On Call by Andrew Stewart in PDF and/or ePUB format, as well as other popular books in Medicine & Internal Medicine & Diagnosis. We have over one million books available in our catalogue for you to explore.