eBook - ePub
Essentials of Cardiac Anesthesia for Noncardiac Surgery E-Book
A Companion to Kaplan's Cardiac Anesthesia
Joel A. Kaplan
This is a test
Condividi libro
- 796 pagine
- English
- ePUB (disponibile sull'app)
- Disponibile su iOS e Android
eBook - ePub
Essentials of Cardiac Anesthesia for Noncardiac Surgery E-Book
A Companion to Kaplan's Cardiac Anesthesia
Joel A. Kaplan
Dettagli del libro
Anteprima del libro
Indice dei contenuti
Citazioni
Informazioni sul libro
- Provides guidance on the anesthetic diagnosis and management of the full range of cardiac lesions, helping minimize adverse outcomes and reduce complications for patients with common, complex, or uncommon cardiac conditions.
- Includes complete coverage of echocardiography and current monitoring techniques needed for thorough perioperative assessment – all from the anesthesiologist's perspective.
- Discusses safe and effective perioperative anesthetic management of patients presenting with advanced levels of cardiac care such as drug-eluting stents, multiple antiplatelet drugs, ventricular assist devices, multiple drugs for end-stage heart failure, and implanted electrical devices that produce cardiac resynchronization therapy, as well as patients with complicated obstetric problems or other significant cardiovascular issues.
- Features a concise, easy-to-navigate format and Key Points boxes in each chapter that help you find answers quickly.
- Provides guidance on the anesthetic diagnosis and management of the full range of cardiac lesions, helping minimize adverse outcomes and reduce complications for patients with common, complex, or uncommon cardiac conditions.
- Includes complete coverage of echocardiography and current monitoring techniques needed for thorough perioperative assessment – all from the anesthesiologist's perspective.
- Discusses safe and effective perioperative anesthetic management of patients presenting with advanced levels of cardiac care such as drug-eluting stents, multiple antiplatelet drugs, ventricular assist devices, multiple drugs for end-stage heart failure, and implanted electrical devices that produce cardiac resynchronization therapy, as well as patients with complicated obstetric problems or other significant cardiovascular issues.
- Features a concise, easy-to-navigate format and Key Points boxes in each chapter that help you find answers quickly.
Domande frequenti
Come faccio ad annullare l'abbonamento?
È semplicissimo: basta accedere alla sezione Account nelle Impostazioni e cliccare su "Annulla abbonamento". Dopo la cancellazione, l'abbonamento rimarrà attivo per il periodo rimanente già pagato. Per maggiori informazioni, clicca qui
È possibile scaricare libri? Se sì, come?
Al momento è possibile scaricare tramite l'app tutti i nostri libri ePub mobile-friendly. Anche la maggior parte dei nostri PDF è scaricabile e stiamo lavorando per rendere disponibile quanto prima il download di tutti gli altri file. Per maggiori informazioni, clicca qui
Che differenza c'è tra i piani?
Entrambi i piani ti danno accesso illimitato alla libreria e a tutte le funzionalità di Perlego. Le uniche differenze sono il prezzo e il periodo di abbonamento: con il piano annuale risparmierai circa il 30% rispetto a 12 rate con quello mensile.
Cos'è Perlego?
Perlego è un servizio di abbonamento a testi accademici, che ti permette di accedere a un'intera libreria online a un prezzo inferiore rispetto a quello che pagheresti per acquistare un singolo libro al mese. Con oltre 1 milione di testi suddivisi in più di 1.000 categorie, troverai sicuramente ciò che fa per te! Per maggiori informazioni, clicca qui.
Perlego supporta la sintesi vocale?
Cerca l'icona Sintesi vocale nel prossimo libro che leggerai per verificare se è possibile riprodurre l'audio. Questo strumento permette di leggere il testo a voce alta, evidenziandolo man mano che la lettura procede. Puoi aumentare o diminuire la velocità della sintesi vocale, oppure sospendere la riproduzione. Per maggiori informazioni, clicca qui.
Essentials of Cardiac Anesthesia for Noncardiac Surgery E-Book è disponibile online in formato PDF/ePub?
Sì, puoi accedere a Essentials of Cardiac Anesthesia for Noncardiac Surgery E-Book di Joel A. Kaplan in formato PDF e/o ePub, così come ad altri libri molto apprezzati nelle sezioni relative a Medicine e Cardiology. Scopri oltre 1 milione di libri disponibili nel nostro catalogo.
Informazioni
Argomento
MedicineCategoria
CardiologySection II
Anesthesia for Noncardiac Surgery
Chapter 9
Cardiovascular Monitoring in Noncardiac Surgery
Gerard R. Manecke Jr, MD, Timothy M. Maus MD
Keywords
hemodynamic monitoring; electrocardiogram; central venous pressure; cardiac output; goal-directed therapy
Key Points
- 1. Excellent cardiac and hemodynamic management is essential to achieving good outcomes in patients with cardiovascular disease, particularly those undergoing high-risk noncardiac surgery.
- 2. Much cardiovascular information can be obtained from the standard American Society of Anesthesiologists monitors, including those usually associated with evaluation of respiratory function (pulse oximetry, capnography). The pulse oximeter plethysmograph can be used to assess adequacy of the peripheral circulation; expired capnography reflects pulmonary blood flow and cardiac output.
- 3. The five-electrode electrocardiographic system commonly used perioperatively allows rapid diagnosis of a wide variety of cardiac abnormalities, including rhythm disturbances, conduction abnormalities, myocardial ischemia, myocardial infarction, and electrolyte abnormalities.
- 4. Although often unreliable as an intravascular volume monitor, invasive monitoring of the central venous pressure (CVP) can be useful in the management of cardiac patients. CVP provides information about the systolic and diastolic performance of the heart in response to fluid administration, as well as waveform information that can aid in the diagnosis of abnormalities such as tricuspid regurgitation and junctional rhythms.
- 5. The pulmonary artery catheter is a very powerful monitor, providing a wide array of data that include right-sided pressures, cardiac performance, and a surrogate for left atrial pressure (pulmonary capillary wedge pressure). Although its use has declined in noncardiac surgery, it is still very useful in select patients such as those with pulmonary hypertension or right ventricular failure. It is also useful for monitoring left ventricular function and solving hemodynamic problems when transesophageal echocardiography is unavailable.
- 6. Minimally invasive and noninvasive means of continuously monitoring arterial blood pressure, as well as cardiac output and dynamic parameters such as stroke volume variation, are now widely used. They are particularly useful in cardiac patients undergoing high-risk surgery. They facilitate perioperative goal-directed therapy (PGDT), enhanced recovery from surgery, and rapid diagnosis of hemodynamic problems.
- 7. Noninvasive monitors that assess tissue oxygenation, pH, and perfusion are likely to be further developed and used. Because the purpose of circulation is tissue perfusion, it is logical to quantify tissue perfusion and oxygenation. Somatic near-infrared spectroscopy is currently used for this purpose in PGDT algorithms.
Perioperative care includes effective cardiac, hemodynamic, and fluid management. Excellent cardiovascular management is particularly important in patients undergoing major noncardiac surgery and those with preexisting cardiovascular disease. It is only with meaningful, accurate monitoring that appropriate cardiac, hemodynamic, and fluid therapy can be provided. This chapter focuses on the various means by which the cardiac and hemodynamic status can be monitored, ranging from noninvasive to highly invasive techniques. Other indicators of cardiovascular function, such as urine output, are discussed as well. Echocardiography is not discussed here; it is presented in Chapter 10.
Standard American Society of Anesthesiologists Monitors
Most of the standard American Society of Anesthesiologists (ASA) monitors provide information about the cardiovascular system (Box 9.1). Electrocardiogram (ECG), arterial blood pressure, heart rate, and intraarterial pressure tracings are obviously useful, but those used to monitor respiratory function, such as end-tidal carbon dioxide (ETCO2) and pulse oximetry with its plethysmograph tracing, can also provide valuable cardiovascular information. The standard ASA monitors are listed in Table 9.1.
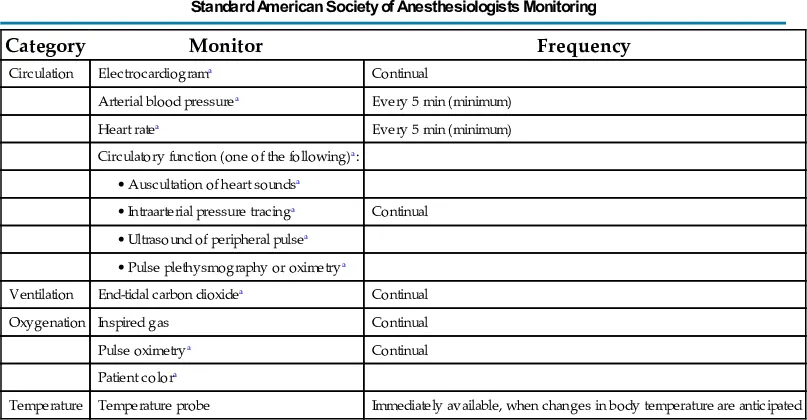
Table 9.1
| Category | Monitor | Frequency |
|---|---|---|
| Circulation | Electrocardiograma | Continual |
| Arterial blood pressurea | Every 5 min (minimum) | |
| Heart ratea | Every 5 min (minimum) | |
| Circulatory function (one of the following)a: | ||
• Auscultation of heart soundsa | ||
• Intraarterial pressure tracinga | Continual | |
• Ultrasound of peripheral pulsea | ||
• Pulse plethysmography or oximetrya | ||
| Ventilation | End-tidal carbon dioxidea | Continual |
| Oxygenation | Inspired gas | Continual |
| Pulse oximetrya | Continual | |
| Patient colora | ||
| Temperature | Temperature probe | Immediately available, when changes in body temperature are anticipated |
aParameters that are useful in cardiovascular monitoring.
From American Society of Anesthesiologists Standards for Basic Monitoring, http://www.asahq.org.
Electrocardiogram
The ECG is a mainstay for monitoring cardiac status. Continuously monitoring cardiac electrical activity, it provides heart rate and rhythm data, as well as assessment of cardiac conduction (PR interval, QRS duration) and repolarization (ST segment, T-wave morphology, and QT interval). The normal morphologies of the ECG signal and the ECG intervals are shown in Fig. 9.1.
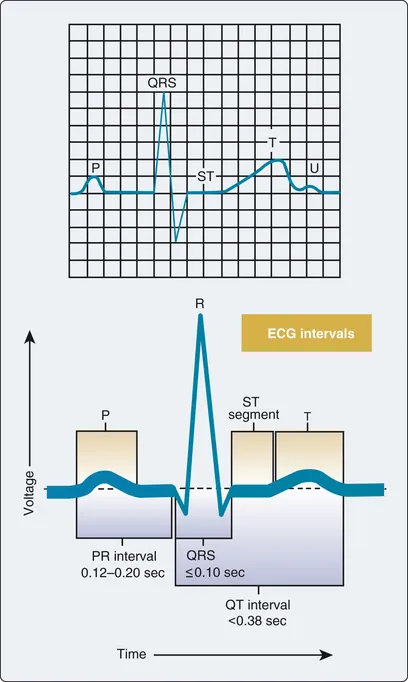
Fig. 9.1 Electrocardiographic morphology of one cardiac cycle and intervals.
A three-lead system, using three or four electrodes (right arm, left arm, left leg, ground), allows monitoring of limb leads I, II, or III, providing primarily rhythm and conduction data. This can suffice for healthy patients, but a five-electrode system (right arm, left arm, left leg, precordial, ground) is usually used perioperatively and in intensive care units. This system allows simultaneous monitoring of a limb lead (usually lead II) and a precordial “V” lead that enhances the detection of myocardial ischemia. The sensitivity for detecting myocardial ischemia when using a combination of leads II and V5 has been reported to be 80%. The V lead can be placed according to the particular area of interest, ranging from anterior (V1) to lateral (V6) (Fig. 9.2), with V3 to V5 generally being the most sensitive for anterior-lateral myocardial ischemia (lead II is used for inferior wall ischemia).
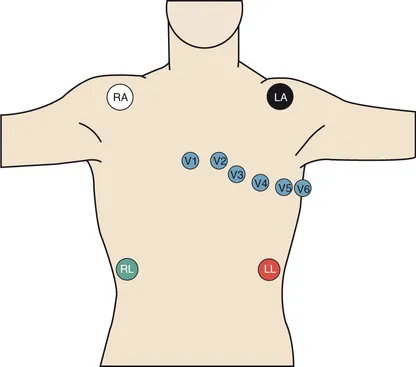
Fig. 9.2 Placement of the five-electrode system commonly used in operating rooms and intensive care units. The precordial lead (V) can be placed according to the area of interest, with the V3 to V5 positions generally being the most sensitive for myocardial ischemia.
Myocardial ischemia most often manifests as ST-segment depression, although elevated ST segments, change in T-wave morphology, new conduction defects, or frequent premature ventricular contractions may also be signs of myocardial ischemia. ECG monitoring systems have automated digital signal processing to continuously display heart rate, QT interval, and ST-segment depression or elevation, as well as alarm systems for these parameters.
Abnormal rhythms, such as sinus bradycardia and tachycardia, junctional rhythms, atrial fibrillation, right and left bundle branch blocks, and heart block, are not uncommon in cardiac patients. All these abnormalities can be detected using a five-electrode system (Tables 9.2 and 9.3). Whereas a limb lead such as lead II is preferred for conduction and rhythm detection, the precordial leads are preferred for diagnosis of myocardial ischem...