eBook - ePub
Essentials of Cardiac Anesthesia for Noncardiac Surgery E-Book
A Companion to Kaplan's Cardiac Anesthesia
Joel A. Kaplan
This is a test
Buch teilen
- 796 Seiten
- English
- ePUB (handyfreundlich)
- Über iOS und Android verfügbar
eBook - ePub
Essentials of Cardiac Anesthesia for Noncardiac Surgery E-Book
A Companion to Kaplan's Cardiac Anesthesia
Joel A. Kaplan
Angaben zum Buch
Buchvorschau
Inhaltsverzeichnis
Quellenangaben
Über dieses Buch
- Provides guidance on the anesthetic diagnosis and management of the full range of cardiac lesions, helping minimize adverse outcomes and reduce complications for patients with common, complex, or uncommon cardiac conditions.
- Includes complete coverage of echocardiography and current monitoring techniques needed for thorough perioperative assessment – all from the anesthesiologist's perspective.
- Discusses safe and effective perioperative anesthetic management of patients presenting with advanced levels of cardiac care such as drug-eluting stents, multiple antiplatelet drugs, ventricular assist devices, multiple drugs for end-stage heart failure, and implanted electrical devices that produce cardiac resynchronization therapy, as well as patients with complicated obstetric problems or other significant cardiovascular issues.
- Features a concise, easy-to-navigate format and Key Points boxes in each chapter that help you find answers quickly.
- Provides guidance on the anesthetic diagnosis and management of the full range of cardiac lesions, helping minimize adverse outcomes and reduce complications for patients with common, complex, or uncommon cardiac conditions.
- Includes complete coverage of echocardiography and current monitoring techniques needed for thorough perioperative assessment – all from the anesthesiologist's perspective.
- Discusses safe and effective perioperative anesthetic management of patients presenting with advanced levels of cardiac care such as drug-eluting stents, multiple antiplatelet drugs, ventricular assist devices, multiple drugs for end-stage heart failure, and implanted electrical devices that produce cardiac resynchronization therapy, as well as patients with complicated obstetric problems or other significant cardiovascular issues.
- Features a concise, easy-to-navigate format and Key Points boxes in each chapter that help you find answers quickly.
Häufig gestellte Fragen
Wie kann ich mein Abo kündigen?
Gehe einfach zum Kontobereich in den Einstellungen und klicke auf „Abo kündigen“ – ganz einfach. Nachdem du gekündigt hast, bleibt deine Mitgliedschaft für den verbleibenden Abozeitraum, den du bereits bezahlt hast, aktiv. Mehr Informationen hier.
(Wie) Kann ich Bücher herunterladen?
Derzeit stehen all unsere auf Mobilgeräte reagierenden ePub-Bücher zum Download über die App zur Verfügung. Die meisten unserer PDFs stehen ebenfalls zum Download bereit; wir arbeiten daran, auch die übrigen PDFs zum Download anzubieten, bei denen dies aktuell noch nicht möglich ist. Weitere Informationen hier.
Welcher Unterschied besteht bei den Preisen zwischen den Aboplänen?
Mit beiden Aboplänen erhältst du vollen Zugang zur Bibliothek und allen Funktionen von Perlego. Die einzigen Unterschiede bestehen im Preis und dem Abozeitraum: Mit dem Jahresabo sparst du auf 12 Monate gerechnet im Vergleich zum Monatsabo rund 30 %.
Was ist Perlego?
Wir sind ein Online-Abodienst für Lehrbücher, bei dem du für weniger als den Preis eines einzelnen Buches pro Monat Zugang zu einer ganzen Online-Bibliothek erhältst. Mit über 1 Million Büchern zu über 1.000 verschiedenen Themen haben wir bestimmt alles, was du brauchst! Weitere Informationen hier.
Unterstützt Perlego Text-zu-Sprache?
Achte auf das Symbol zum Vorlesen in deinem nächsten Buch, um zu sehen, ob du es dir auch anhören kannst. Bei diesem Tool wird dir Text laut vorgelesen, wobei der Text beim Vorlesen auch grafisch hervorgehoben wird. Du kannst das Vorlesen jederzeit anhalten, beschleunigen und verlangsamen. Weitere Informationen hier.
Ist Essentials of Cardiac Anesthesia for Noncardiac Surgery E-Book als Online-PDF/ePub verfügbar?
Ja, du hast Zugang zu Essentials of Cardiac Anesthesia for Noncardiac Surgery E-Book von Joel A. Kaplan im PDF- und/oder ePub-Format sowie zu anderen beliebten Büchern aus Medicine & Cardiology. Aus unserem Katalog stehen dir über 1 Million Bücher zur Verfügung.
Information
Thema
MedicineThema
CardiologySection II
Anesthesia for Noncardiac Surgery
Chapter 9
Cardiovascular Monitoring in Noncardiac Surgery
Gerard R. Manecke Jr, MD, Timothy M. Maus MD
Keywords
hemodynamic monitoring; electrocardiogram; central venous pressure; cardiac output; goal-directed therapy
Key Points
- 1. Excellent cardiac and hemodynamic management is essential to achieving good outcomes in patients with cardiovascular disease, particularly those undergoing high-risk noncardiac surgery.
- 2. Much cardiovascular information can be obtained from the standard American Society of Anesthesiologists monitors, including those usually associated with evaluation of respiratory function (pulse oximetry, capnography). The pulse oximeter plethysmograph can be used to assess adequacy of the peripheral circulation; expired capnography reflects pulmonary blood flow and cardiac output.
- 3. The five-electrode electrocardiographic system commonly used perioperatively allows rapid diagnosis of a wide variety of cardiac abnormalities, including rhythm disturbances, conduction abnormalities, myocardial ischemia, myocardial infarction, and electrolyte abnormalities.
- 4. Although often unreliable as an intravascular volume monitor, invasive monitoring of the central venous pressure (CVP) can be useful in the management of cardiac patients. CVP provides information about the systolic and diastolic performance of the heart in response to fluid administration, as well as waveform information that can aid in the diagnosis of abnormalities such as tricuspid regurgitation and junctional rhythms.
- 5. The pulmonary artery catheter is a very powerful monitor, providing a wide array of data that include right-sided pressures, cardiac performance, and a surrogate for left atrial pressure (pulmonary capillary wedge pressure). Although its use has declined in noncardiac surgery, it is still very useful in select patients such as those with pulmonary hypertension or right ventricular failure. It is also useful for monitoring left ventricular function and solving hemodynamic problems when transesophageal echocardiography is unavailable.
- 6. Minimally invasive and noninvasive means of continuously monitoring arterial blood pressure, as well as cardiac output and dynamic parameters such as stroke volume variation, are now widely used. They are particularly useful in cardiac patients undergoing high-risk surgery. They facilitate perioperative goal-directed therapy (PGDT), enhanced recovery from surgery, and rapid diagnosis of hemodynamic problems.
- 7. Noninvasive monitors that assess tissue oxygenation, pH, and perfusion are likely to be further developed and used. Because the purpose of circulation is tissue perfusion, it is logical to quantify tissue perfusion and oxygenation. Somatic near-infrared spectroscopy is currently used for this purpose in PGDT algorithms.
Perioperative care includes effective cardiac, hemodynamic, and fluid management. Excellent cardiovascular management is particularly important in patients undergoing major noncardiac surgery and those with preexisting cardiovascular disease. It is only with meaningful, accurate monitoring that appropriate cardiac, hemodynamic, and fluid therapy can be provided. This chapter focuses on the various means by which the cardiac and hemodynamic status can be monitored, ranging from noninvasive to highly invasive techniques. Other indicators of cardiovascular function, such as urine output, are discussed as well. Echocardiography is not discussed here; it is presented in Chapter 10.
Standard American Society of Anesthesiologists Monitors
Most of the standard American Society of Anesthesiologists (ASA) monitors provide information about the cardiovascular system (Box 9.1). Electrocardiogram (ECG), arterial blood pressure, heart rate, and intraarterial pressure tracings are obviously useful, but those used to monitor respiratory function, such as end-tidal carbon dioxide (ETCO2) and pulse oximetry with its plethysmograph tracing, can also provide valuable cardiovascular information. The standard ASA monitors are listed in Table 9.1.
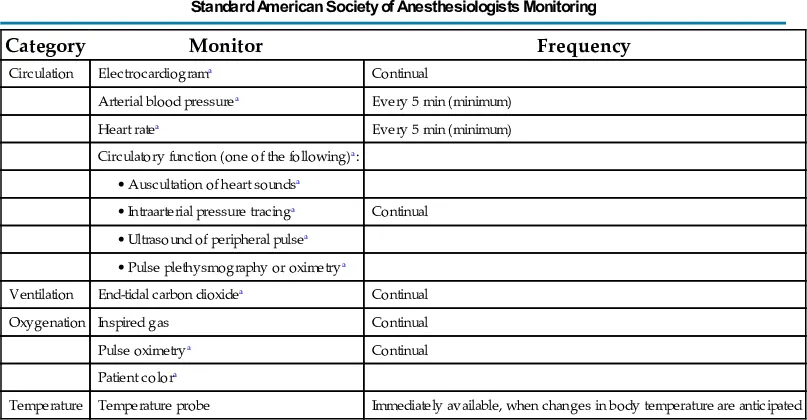
Table 9.1
| Category | Monitor | Frequency |
|---|---|---|
| Circulation | Electrocardiograma | Continual |
| Arterial blood pressurea | Every 5 min (minimum) | |
| Heart ratea | Every 5 min (minimum) | |
| Circulatory function (one of the following)a: | ||
• Auscultation of heart soundsa | ||
• Intraarterial pressure tracinga | Continual | |
• Ultrasound of peripheral pulsea | ||
• Pulse plethysmography or oximetrya | ||
| Ventilation | End-tidal carbon dioxidea | Continual |
| Oxygenation | Inspired gas | Continual |
| Pulse oximetrya | Continual | |
| Patient colora | ||
| Temperature | Temperature probe | Immediately available, when changes in body temperature are anticipated |
aParameters that are useful in cardiovascular monitoring.
From American Society of Anesthesiologists Standards for Basic Monitoring, http://www.asahq.org.
Electrocardiogram
The ECG is a mainstay for monitoring cardiac status. Continuously monitoring cardiac electrical activity, it provides heart rate and rhythm data, as well as assessment of cardiac conduction (PR interval, QRS duration) and repolarization (ST segment, T-wave morphology, and QT interval). The normal morphologies of the ECG signal and the ECG intervals are shown in Fig. 9.1.
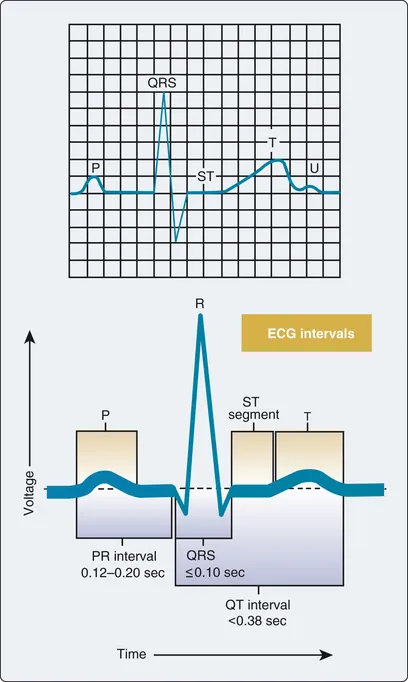
Fig. 9.1 Electrocardiographic morphology of one cardiac cycle and intervals.
A three-lead system, using three or four electrodes (right arm, left arm, left leg, ground), allows monitoring of limb leads I, II, or III, providing primarily rhythm and conduction data. This can suffice for healthy patients, but a five-electrode system (right arm, left arm, left leg, precordial, ground) is usually used perioperatively and in intensive care units. This system allows simultaneous monitoring of a limb lead (usually lead II) and a precordial “V” lead that enhances the detection of myocardial ischemia. The sensitivity for detecting myocardial ischemia when using a combination of leads II and V5 has been reported to be 80%. The V lead can be placed according to the particular area of interest, ranging from anterior (V1) to lateral (V6) (Fig. 9.2), with V3 to V5 generally being the most sensitive for anterior-lateral myocardial ischemia (lead II is used for inferior wall ischemia).
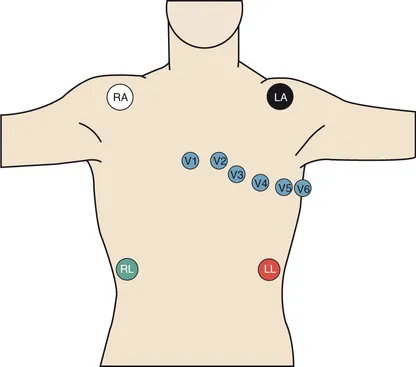
Fig. 9.2 Placement of the five-electrode system commonly used in operating rooms and intensive care units. The precordial lead (V) can be placed according to the area of interest, with the V3 to V5 positions generally being the most sensitive for myocardial ischemia.
Myocardial ischemia most often manifests as ST-segment depression, although elevated ST segments, change in T-wave morphology, new conduction defects, or frequent premature ventricular contractions may also be signs of myocardial ischemia. ECG monitoring systems have automated digital signal processing to continuously display heart rate, QT interval, and ST-segment depression or elevation, as well as alarm systems for these parameters.
Abnormal rhythms, such as sinus bradycardia and tachycardia, junctional rhythms, atrial fibrillation, right and left bundle branch blocks, and heart block, are not uncommon in cardiac patients. All these abnormalities can be detected using a five-electrode system (Tables 9.2 and 9.3). Whereas a limb lead such as lead II is preferred for conduction and rhythm detection, the precordial leads are preferred for diagnosis of myocardial ischem...