eBook - ePub
Handbook of Obstetric High Dependency Care
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Handbook of Obstetric High Dependency Care
About this book
Concise practical guidance to managing an Obstetric High Dependency unit
The team and clinical environment is the starting point for the Handbook of Obstetric High Dependency Care. The book discusses the structure and requirements of a unit, both clinically and in terms of equipment, protocols and management aims. The main sections cover the investigation, diagnosis and management of clinical disease resulting from pregnancy and incidental to it.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Handbook of Obstetric High Dependency Care by David Vaughan,Neville Robinson,Nuala Lucas,Sabaratnam Arulkumaran in PDF and/or ePUB format, as well as other popular books in Medicine & Gynecology, Obstetrics & Midwifery. We have over one million books available in our catalogue for you to explore.
Information
CHAPTER 1
Morbidity and mortality in the parturient
Maternal mortality and CEMACH
The Confidential Enquiry into Maternal Deaths in England and Wales was launched in 1955. The report evolved into the Confidential Enquiry into Maternal and Child Health (CEMACH) which came into being on 1 April 2003. CEMACH, funded by the National Patient Safety Agency (NPSA), was an independent body with board members being made up of representatives from the Royal College of Obstetricians and Gynaecologists (RCOG), Midwives (RCM), Anaesthetists (RCA), Pathologists, Paediatrics and Child Health and the Faculty of Public Health Medicine of the Royal College of Physicians. The report is the longest running and most complete record of the causes of maternal death in the developed world. The reduction on maternal death rates not only in the UK but also throughout the world owes a huge debt to these triennial reports. On 1 July 2009, CEMACH became an independent charity with the new name ‘Centre for Maternal and Child Enquiries’ (CMACE).
The leading causes of maternal mortality are shown in Box 1.1.
Box 1.1 Causes of maternal mortality in the UK (CEMACH 2003–2005)
Direct
- Thrombosis/thromboembolic disease (TED)
- Pre-eclampsia/eclampsia
- Amniotic fluid embolism
- Genital tract sepsis
- Haemorrhage
Indirect
- Cardiac disease
- Psychiatric disease
The leading cause of direct maternal death in the UK is thrombosis and/or thromboembolic disease, and this has been the case for more than 20 years. However, within this group the pattern of disease has changed over this period. There has been a decrease in the number of deaths due to pulmonary embolism after caesarean section, almost certainly as a result of increased awareness in the obstetric team and meticulous use of thromboprophylaxis guidelines. This pattern has not been reflected in the number of antepartum deaths where there has been a slight increase since 1985.
Genital tract sepsis has again become a leading cause of maternal death in the UK and this is of particular relevance to the maternity high dependency unit (MHDU) where it is likely that not only women with a diagnosis of sepsis may be cared for but also women who are at risk of maternal sepsis. It was commented upon in the last confidential enquiry that the advent of antibiotics and aseptic precautions had led to a dramatic reduction in the number of deaths from sepsis in the early years of the confidential enquiry and that this in turn had removed the anxiety of maternal sepsis from our ‘collective memory’. The report recommended action to raise awareness of the recognition and management of maternal sepsis in all healthcare professionals who may care for the obstetric patient and also that maternal early warning scoring systems be implemented.
Cardiac disease is now the leading overall cause of maternal death in the UK. The principal causes of death in this group are aortic dissection and myocardial ischaemia. The changes over the last 50 years in the population of women of childbearing age in the UK (rising maternal age at childbirth, increasing levels of obesity) are likely to have had an impact in this area.
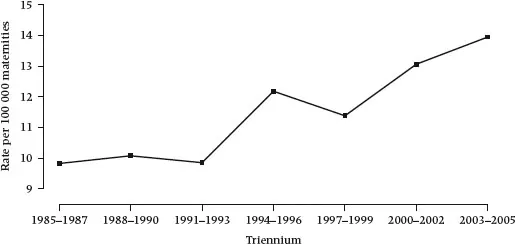
Despite the huge impact of the report, the UK maternal mortality rate has not fallen in recent years (Figure 1.1). A number of factors may have contributed to this lack of decline. One possible explanation for this is the increasing numbers of high risk patients becoming pregnant.
Figure 1.1 Overall maternal mortality rate (deaths from direct and indirect causes combined) per 100 000 maternities, UK, CEMACH.
Maternal morbidity
There is increasing recognition of the importance of the relationship between mortality and morbidity. Unlike maternal mortality, the full extent of maternal morbidity is not known. In a case control study published by Waterstone et al. (2001) estimated the incidence of severe obstetric morbidity at 12.0/100 deliveries. Another study from the USA estimated that 43% of women experienced some form of maternal morbidity.
Women who have experienced and survived a severe health condition in the antepartum period, at delivery or in the post-partum period are considered as cases of ‘near miss’ or ‘severe acute maternal morbidity’ (SAMM). The terms ‘near miss’ and ‘SAMM’ have been used interchangeably but the World Health Organization (WHO) working group on maternal morbidity and mortality recommends the use of the term ‘maternal near miss’. There are various definitions of maternal near miss and these have been amalgamated by the WHO to provide one clear definition (Box 1.2).
Box 1.2 WHO International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD10) – Definition of maternal near miss
A woman who nearly died but survived a complication during pregnancy, childbirth or within 42 days of termination of the pregnancy
In the past, maternal mortality and morbidity have been studied in isolation from one another, but it is clear that if the two are treated as separate clinical entities and by only investigating mortality, the chance to detect other problems in maternity care is lost. The relationship between morbidity and mortality in pregnancy has been described as a ‘continuum of adverse pregnancy events’ (Box 1.3).
Box 1.3 The continuum of adverse pregnancy events
Normal healthy pregnancy → Morbidity → Severe Morbidity → Near miss → Death
Source: Stacie E Geller. Am J Obstet Gynecol 2004;191:939–944.
Studies into maternal near miss cases have shown that the predominant underlying obstetric causes of obstetric morbidity differ somewhat from the major causes of maternal mortality. In the most recent CEMACH report, haemorrhage was the fourth commonest cause of direct maternal death, but in the Scottish audit of obstetric morbidity it was by far the most common cause of obstetric morbidity. Therefore it has been suggested that while enquiries into maternal near misses cannot completely act as a surrogate for maternal mortality, they can deliver information that complements the findings of studies into maternal deaths. What is perhaps even more interesting is the fact that it has been shown that a woman’s progression along the continuum is affected by medical decision-making. This would suggest that identification of the high risk parturient as early as possible should have a major role in the primary and secondary prevention of morbidity and mortality.
Maternal mortality, morbidity and the MHDU
The purpose of an MHDU is to provide care to women at risk of or experiencing morbidity at any stage during the antenatal or postnatal period. It is required to improve care and reduce maternal mortality and morbidity for the sick or high risk obstetric patient. There are two major components of MHDU care (Box 1.4).
Box 1.4 Major components of maternity high dependency care
- Timely recognition of the sick or high risk obstetric patient
- Delivery of high quality, dedicated maternity high dependency care
The high risk parturient
The term ‘high risk’ in association with pregnancy is often used interchangeably to refer to either the mother or the fetus being high risk. For the purposes of this discussion, the term ‘high risk parturient’ refers to a pregnant woman at risk of developing serious morbidity or mortality. Factors that may put a woman into the high risk parturient group may be divided into four categories (Box 1.5).
Box 1.5 Factors that may predispose a parturient to becoming high risk
Pre-existing disease
- Heart disease – congenital, ischaemic, valvular
- Respiratory disease – asthma, cystic fibrosis
- Renal – acute or chronic renal failure
- Neurological – e.g. multiple sclerosis, epilepsy, cerebrovascular disease
- Musculoskeletal – e.g. scoliosis ± surgery, connective tissue disorders
- Haematological – thrombocytopenia, thrombophilias
Pregnancy-related disease
- Pre-eclampsia
- Haemorrhage
- Acute fatty liver
- Peri-partum cardiomyopathy
Social factors
- Social disadvantage
- Poor communities
- Ethnic minorities
- Late bookers
- Obesity
- Domestic violence
- Substance abuse
Miscellaneous factors
- Jehovah’s witness
- Needle phobia
- Anaesthetic-related issues – e.g. allergy, suxamethonium apnoea
Identification of the high risk parturient
Identification of the ‘high risk’ parturient is key to the prevention of obstetric morbidity and mortality. Early identification allows time to plan effective multidisciplinary management strategies for the high risk woman. It is the responsibility of all healthcare professionals who may be (but not necessarily routinely) involved in the care of the pregnant woman. A woman may be identified as being high risk at any stage from pre-conception ...
Table of contents
- Cover
- Contents
- Title
- Copyright
- List of abbreviations
- List of figures
- List of boxes
- Preface
- Chapter 1: Morbidity and mortality in the parturient
- Chapter 2: The maternity high dependency unit
- Part I: Emergency care
- Part II: Clinical problems
- Selected bibliography
- Index