![]()
1
Introduction
1.1 What is the recovery movement in psychiatry?
In 1999, the Surgeon General of the United States – the top physician for the country – issued a first-ever Report on Mental Health (Department of Health and Human Services, 1999). This 458-page tome included much important information and many surprises, but to those of us who consider ourselves part of the recovery movement, its most prominent feature came near the very end of the book with the simple assertion that all mental health care should be ‘consumer oriented and focused on promoting recovery’ (Department of Health and Human Services, 1999, p. 455). To naïve readers, this statement may appear simply to be asserting the obvious, that is if mental health services were not focused on promoting recovery, what else might they be for? Or perhaps some readers will see this statement as indicating that mental health care should just become more like general medical care, assuming more of the ‘customer service’ philosophy that has been spreading throughout medicine for the last decade under the rubric of ‘patient-centred’ or ‘person-centred’ care (O’Brien, 1987;O’Brien and Lovett,1992;Laine and Davidoff, 1996;Marrone, Hoff and Helm, 1997; O’Brien and O’Brien, 2000; O’Brien, 2002; Tondora et al., 2005; McCormack and McCance, 2006). The matter-of-fact tone with which this statement was made could certainly support either of these interpretations.
But for those readers who are more familiar with the history of psychiatry, and who are aware, in particular, of the history of the use of the term ‘consumer’ within psychiatry, this statement means something entirely different. Its appearance in a Surgeon General’s report on mental health in fact heralded the beginning of a new era in psychiatry, an era in which radical reforms are to be made in how we understand and treat mental illnesses and, equally importantly, how we understand and treat individuals living with mental illnesses. To those individuals who considered themselves mental health ‘consumers’, and to those other advocates of ‘recovery’ – a term we define below – who had been fighting a battle of values, principles and ideas for over 30 years, this statement indicated that we had, at last, won a prolonged – if relatively bloodless – war. One of the many surprising things about this statement appearing in an official federal report in 1999, though, was that it was not at all clear yet what war precisely it was that we had won.
The following book represents one more attempt to help to define the nature of the war and the implications of its having been won for individuals with mental illnesses, their loved ones and the mental health practitioners, programme managers and system leaders who have the privilege of serving and supporting them. Perhaps it is not unusual for wars to be won before either party realizes all of what has been at stake and what exactly is to result from victory. The current wars in Iraq and Afghanistan certainly confirm this, but so do the American and French revolutions. So perhaps it is perfectly understandable that we now are in a position of having to establish, clarify and defend what it is that has been won in the process. Unlike the American and French revolutions, and the wars in Iraq and Afghanistan, however, this was a war that the vast majority of the public, including that segment of the public involved directly in mental health care, did not even know was being waged. It was for perhaps this reason in particular that the war’s having already been won in 1999 came as such a surprise, at least to those of us who were not serving on the front line at the time.
Some readers will undoubtedly object to our use of the term ‘war’, as the mental health consumer and broader recovery movements have never involved use of force or other violent means. They have not even involved labor or hunger strikes, sit-ins, large-scale political rallies or other non-violent acts of resistance, although there have been occasional marches and the creation and dissemination of protest songs, folk ballads, inspirational poetry and manifestos. On the other hand, though, it is important to recognize that these movements were indeed in response to centuries of violence and bloodshed in which people with mental illnesses were stoned, burned at the stake, locked in cages, chained to posts and walls, confined to squalid and inhumane living conditions, insulin-shocked, hydro-shocked, electro-shocked and lobotomized.
Lest the reader think that these atrocities are all only in the distant past, or only continue to occur in the developing world, a recent report released by the US Medical Directors Council of the National Association of State Mental Health Program Directors suggests otherwise. Since the mid-1980s, there has been an increase, rather than a decrease, in the discrepancy in average lifespan between those with and those without a serious mental illness. While the discrepancy in lifespan was a ‘mere’ 12 years in 1986, it more than doubled to 25 years by 2006 (McCarrick et al., 1986; Colton and Manderscheid, 2006). That means that in 2006 in the United States people with serious mental illnesses died on average 25 years younger than their peers. This loss of one-third of their lifespan is due to a combination of factors, including higher rates of suicide and substance use; a lack of access to and/or inadequate treatment of medical conditions like diabetes, heart and respiratory diseases; and higher rates of preventable and modifiable risk factors, such as obesity, poor nutrition and lack of exercise. It is hard to imagine that a prosperous society would tolerate a loss of one-third of the expected lifespan in any other population of its own citizens, providing at least one clear and unequivocal indicator of the fact that stigma and discrimination continue to exist against individuals with mental illnesses – with concrete, tangible and appalling results.
The stigma experienced by and the discrimination against individuals with mental illnesses – while not carried out (any longer) through burnings at the stake, lobotomies or other violent means – thus remain nonetheless serious, life-or-death, matters. Add to this recognition of the huge numbers of individuals with serious mental illnesses currently being held in jails across the country for non-violent and petty crimes and one can begin to appreciate the need for radical reform. How did the Surgeon General’s assertion that mental health care should be ‘consumer oriented and focused on promoting recovery’ intend to change this picture? What kind of transformation is required in mental health care – ‘transformation’ being the term chosen by the subsequent US President’s New Freedom Commission on Mental Health to capture the degree of deep and substantive change required (Department of Health and Human Services, 2003) – and how is it to be achieved? To return to our metaphor, what war precisely is it that we have won and, perhaps even more importantly, what will we now need to do to establish and keep the peace?
We return briefly to the Surgeon General’s landmark report. The sentence which follows the assertion quoted above reads: ‘That is, the goal of services must not be limited to symptom reduction but should strive for restoration of a meaningful and productive life’ (Department of Health and Human Services, 1999, p. 455). ‘Recovery’ for the person with the illness (the ‘consumer’) is thus defined as restoration of a meaningful and productive life. This is what the mental health consumer/survivor/ex-patient movement advocated, and this has been the overarching aim of the recovery movement: to afford people with serious mental illnesses the rights, opportunities and resources needed to lead meaningful and productive lives. The New Freedom Commission’s final report which followed four years after release of the Surgeon General’s report went several steps further, defining this life as involving living, learning, working (a somewhat puritanical list to which we have added the terms ‘loving’ and ‘playing’) and participating fully in community life, having as its vision ‘a life in the community for everyone’ (Department of Health and Human Services, 2003, p. 1).
At a minimum, this vision would suggest that individuals with serious mental illnesses should no longer be confined to hospitals or other institutional settings but should be free and enabled to live in the community alongside their non-disabled peers (Davidson, 2007a). The New Freedom Commission, and the Supreme Court’s Olmstead Decision which was issued at almost the same time, stressed that this was a vision that should be accessible to everyone with a serious mental illness, no matter how disabled they may be or the nature of the supports they may require in order to live as independently as possible. It is rather an issue of (i) assisting the person in learning how to live with and manage his or her condition and (ii) identifying the services and supports needed to enable him or her to do so. The field of psychiatric rehabilitation will take on these related challenges and will develop approaches and strategies for instilling hope and encouraging the person to mobilize his or her remaining strengths and resources in order to gain mastery over the illness; identify, set, pursue and accomplish personal goals; and, in general, live a meaningful and satisfying life in the face of an ongoing, if not necessarily life-long, condition (Corrigan et al., 2008).
Two major obstacles to adopting a disability model and addressing these challenges in relation to serious mental illnesses are recognition of the fact that we do not currently have a cure for these disorders (even though many people recover fully from them nonetheless; Davidson, Harding and Spaniol, 2005) and the need to move from an acute care to a disease, or recovery, management model. Although we may already tell people with serious mental illnesses that they have ‘chronic’ diseases for which they may have to take medication for the remainder of their lives – just as people with diabetes have to take insulin – we have not taken this model very seriously ourselves. We have not fully accepted that there currently is no cure for psychosis, and that there does not yet appear to be promise of one any time soon. Instead, we insist that people adhere to prescribed treatments, including medications which have limited effectiveness (i.e. not nearly as effective as insulin), and expect them to wait until their illness abates before they resume their lives, as if they are suffering from an acute illness. We do not expect people with diabetes to put their lives on hold until the illness resolves, because we know that as of today we have no way to resolve the illness. They are thus encouraged to pursue their own hopes, dreams and aspirations – learn how to play football, drive a car, go on dates and marry – managing their illness within the context of this life as best they can. This is the meaning of the term ‘recovery’ in relation to serious mental illnesses that is used in the Surgeon General’s and New Freedom Commission’s reports, and the meaning of the term articulated and promoted by the subsequent federal Action Agenda, in which we read that the magnitude of change that will be required to implement this vision of recovery is ‘revolutionary’ (Department of Health and Human Services, 2005, p. 18).
The following book is concerned primarily with identifying what is revolutionary about this use of the term recovery and what its transformative implications for mental health practice are. Is it possible for serious mental illnesses to be treated truly the same as other chronic medical conditions? Is it possible to imagine a world in which serious mental illnesses were as well accepted, almost invisible, a part of life as diabetes? Will it be possible to develop supports and prostheses that represent the equivalent of psychiatric wheelchairs or Braille to help people compensate for the more enduring and disabling aspects of these ‘brain diseases’? Will we be able to afford people a personally meaningful and gratifying life in the communities of their choice while they continue to experience a serious mental illness? These are some of the questions that face the recovery movement in psychiatry, some of the questions that will have to be addressed in establishing, and keeping, the peace if we are to be successful in ushering in a truly new era in mental health, an era in which despair will be replaced by hope, demoralization and helplessness will be replaced by dedication and commitment and empty lives will be filled with both the joys and the sorrows of ordinary everydayness (Davidson et al., 2005; Borg and Davidson, 2007).
While the answers to these questions remain far from certain, earnest efforts are being made every day to come up with innovative and creative solutions to the problems posed by mental illness. We consider this book one of those efforts. We hope that as a result of looking backwards we will be able to offer some useful directions for moving the recovery movement, and the broader field of psychiatry, forwards.
Because we are primarily looking backwards, a note on the language used in this book is unfortunately necessary. We believe strongly in, and adhere to, person-first language in our own work, including in our own writing in this volume. We thus refer to individuals with serious mental illnesses as people with serious mental illnesses, or people in recovery, rather than as ‘the mentally ill’ or any one of the historical epithets used to refer to such individuals (e.g. ‘mental patients’, ‘schizophrenics’, ‘manic depressives’, etc.). It is, as we will repeatedly stress, a foundation of the recovery movement to view people with serious mental illnesses as people first and foremost, and only secondarily as people who have happened to develop a mental illness. The illness or diagnosis can no longer be viewed as subsuming the person.
We cannot, however, change the past. And thus, when quoting from some of these historical figures, we have had to include their own language, despite the fact that it may very well be offensive to some readers. We agree that it is offensive. But we also think it important to include their original language rather than to purge it of these offensive terms. For one reason, it is important that we be reminded of how people with serious mental illnesses were viewed and treated in the past so that we not repeat these same mistakes. Second, it can be taken as a sign of the progress we have made thus far that we no longer refer to such individuals as ‘maniacs’, ‘lunatics’ or ‘schizophrenics’. As here, when we use these terms in the text, we set them apart using single quotation marks to denote their historical significance and to remind the reader, if necessary, that these are now outdated terms of reference.
1.2 Rationale for the book
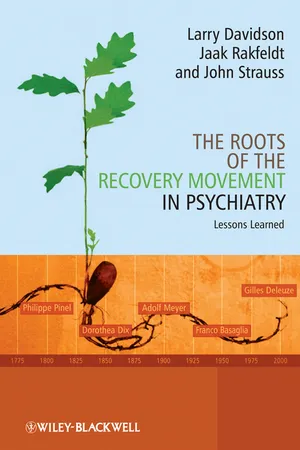
Why did we choose to write a book on the roots of the recovery movement in psychiatry? Especially for a movement so early in its evolution, and whose ultimate impact on the field is so far from certain, it may seem premature to be looking backwards and trying to discern its history. This is not that kind of history, however. We use the term ‘roots’ in a conceptual sense rather than in a historical one. In other words, this book is not a historical account of how the recovery movement actually came to be. There is a very simple answer to that question, which we and others have discussed elsewhere (Chamberlin, 1990; Deegan, 1992; Davidson et al., 2009). For a more thorough and complex answer, we will all have to wait for the historians to take the long view of the role of this movement as a social, political and intellectual force in psychiatry; but many more years will need to pass before we will be able to look back on and determine that history. It will be a very different history, for example, should recovery represent no more than a temporary fad, going the way of phrenology in the nineteenth century or problems in living in the 1970s, as opposed to bringing about the transformation of care that it currently promises to achieve (Department of Health and Human Services, 2003; Department of Health and Human Services, 2005). We will leave that determination for others.
What, then, do we mean by the ‘roots of recovery’, and why are we interested in them? The answer to this question is not nearly as simple as the historical one, but it is one that we think cannot wait until the movement has come to its natural conclusion. In fact, we think that the answer to this question – if given clearly, persuasively and with ample illustrations of its concrete implications – may be able to contribute to the eventual success of this movement, and it is for this reason that we are offering this book now rather than waiting until the movement has attained greater maturity. Briefly stated, many of our presentations, workshops and trainings on recovery and recovery-oriented practice have been met with the response: ‘But we are doing this already.’ Granted, this response only comes from a select few participants each time; it typically comes from those participants who have the most invested in the current system and who hold considerable power and authority over any possible changes that might be made in the future. They are, more often than not, those individuals we are most concerned about reaching in a given system, those individuals who most need to grasp and appreciate the scope and magnitude of the transformation that is involved in re-orienting mental health services to promote resilience and recovery.
As we noted above, according to the President’s New Freedom Commission on Mental Health, we are being called upon to ‘fundamentally refashion’ mental health care (Department of Health and Human Services, 2003, p. 5). According to the subsequent American federal Action Agenda that provides the blueprint for implementing the recommendations of the Commission:
Mere reforms to the existing mental health system are insufficient… Applied to the task at hand, transformation represents a bold vision to change the very form and function of the mental health service delivery system . . . It implies profound change – not at the margins of a system, but at its very core . . . (Department of Health and Human Services, 2005, p. 5)
Parallel documents in Canada (Standing Senate Committee on Social Affairs, Science and Technology, 2006), New Zealand (Mental Health Commission, 1998) and the United Kingdom (Care Services Improvement Partnership, 2006) reflect similar sentiments. Clearly, the organizations and institutions endorsing the recovery vision and recommending that all mental health services be re-oriented to promote resilience and recovery do not think that we are ‘doing it already’.
It is on this gap between a revolutionary vision for the future of mental health care and the current realities of everyday clinical and rehabilitative practice that this book will focus. When we have asked our sceptics in what ways they are already offering recovery-oriented mental health care or practising in ways that promote resilience and recovery, their responses usually land in one of several camps. They may, for example suggest that recovery is simply a throw back to the days of ‘moral treatment’, in which humane staff used gentle, supportive and primarily educational interventions to help the residents of their asylums get back on their feet and resume their normal routines and responsibilities, a time during which ‘recovery’ rates were estimated to be as high as 90%. Or they may suggest that being recovery-oriented refers to the active listening and other efforts that psychoanalytically oriented practitioners made to explore and understand the subjective experiences, or inner lives, of their patients in psychodynamic treatment within the context of long-term hospitalization. Here much attention was paid to developing respectful relationships in which the practitioner helped the person to identify and pursue his or her own goals, with adherents of this approach claiming also to have seen the successful resolution of many cases (Karon, 2008). In both of these examples, of course, what appears to be overlooked is that the care provided was institution-based and that it was extremely difficult to establish and lead ‘a life in the community’ – the vision of recovery put forth by the New Freedom Commission – when confined to a psychiatric hospital. This point is also ignored by people who point to the heyday of the large state hospitals as evidence of a time when people with serious mental illnesses were put to work as part of self-sustaining farms, work for which they, unfortunately, were never paid.
At the opposite end of the spectrum, others will suggest that we already treat people with serious mental illnesses the same way we treat people with other chronic medical illnesses, such as asthma or diabetes. They agree with the sentiments that mental illnesses are illnesses like any other, that they are treatable and that people can lives meaningful live in the face of them. Others will argue that we have been ‘doing recovery’ at least since 1976, with the emergence of the community support movement. This was the movement that introduced such advances in practice as assertive community treatment, self-help and peer support, family education and support and psychiatric rehabilitation. It is true, of course, that use of the term ‘recovery’ in relation to serious mental illnesses did develop in its contemporary form (i.e. as opposed to during the moral treatment era) within the context of this movement. In these two cases, though, what appears to be lost is the important if subtle distinction between recovery, which refers to what the person with the mental illness does, and recovery-oriented care, which refers to what practitioners provide in support of the person’s recovery (Davidson et al., 2007). We will argue in the following that the recovery movement is first and foremost a civil rights movement by and for people with serious mental illnesses (Davidson, 2006; Davidson et al., 2006). It is only secondarily a movement which has implications for the way mental health practitioners practise. To the degree to which people associate recovery solely with how practitioners practise, they miss the critical and central role played by the person him- or herself. In this case, even if we (i.e. practitioners) do actually ‘do it already’, this is of little consolation if people with serious mental illnesses have yet to reclaim their lives as citizens of their community.
In the end, however, we are not as much interested in refuting these examples as we are in learning from them. It is not helpful simply to point out how people offering up these examples have missed important aspects of recovery-oriented care, such as the desire to live in the community rather than in the hospital or the right to be paid a decent wage for one’s labor. What is more interesting is the way in which these examples were right about certain aspects of care, and what we can learn from these prior efforts. We could argue, for instance, that one thing that was common to all of these efforts was the recognition – as partial as it might have been – that people with serious mental illnesses remained people who had certain interests and capacities. If we agree with Patricia Deegan, an international leader of the recovery movement, that ‘The concept of recovery is rooted in the simple yet profound realization that people who have been diagnosed with a mental illness are human beings’ (Deegan, 1993, p. 8), then this insight was a core element of these earlier approaches that is shared by the contemporary notions of recovery and recovery-oriented care. Rather than argue that we are not proposing a return to moral treatment or to exploratory psychoanalytic treatment, it is useful to acknowledge that the recovery movement does share certain values, principles and perhaps even strategies with some of these approaches. We certainly understand that this is not the first time in the history of psychiatry that we have attempted to treat people with serious mental illnesses as people. What we take up in the following volume is what lessons have been learned by these previous attempts, and how these lessons can help us in our current efforts to get it right this time round.
It is useful to note, for example, that people with serious mental illnesses participated actively in music, art, exercise and educational activities when offered such opportunities within well-staffed and therapeutically oriented hospitals. It is also useful to note that even within largely custodial institutions people with serious mental illnesses were able to work with little, if any, support. It is equally useful to know that many more people can work with supports, and that work has an ameliorative effect on symptoms (Drake et al., 1994; Drake et al., 1999). Each of these camps thus has im...