- English
- ePUB (mobile friendly)
- Available on iOS & Android
Hoffbrand's Essential Haematology
About this book
The new and fully updated edition of the definitive haematology textbook for undergraduate and postgraduate students and trainees
Hoffbrand's Essential Haematology is widely regarded as the most authoritative introduction to the subject available, helping medical students and trainee doctors understand the essential principles of modern clinical and laboratory haematology for nearly four decades. Now in its eighth edition, this market-leading textbook introduces the formation and function of blood cells and the diseases that arise from dysfunction and disruption of these processes.
Beautifully presented with over 300 stunning colour illustrations, the new edition has been thoroughly updated to reflect recent advances in knowledge of the pathogenesis of blood diseases and their diagnosis and treatment. This new text:
- Describes disorders and diseases of the blood such as the various anaemias and white cell disorders, leukaemias, lymphomas and myeloma, as well as bleeding and thrombotic disorders
- Incorporates the latest World Health Organization (WHO) classification of haematological neoplastic diseases
- Reviews contemporary application of multiparameter flow cytometry, DNA sequencing and other technologies in evaluating patients with suspected haematological disease
- Discusses the therapeutic use of chimeric antigen T-cells, mono- and bi-specific monoclonal antibodies, inhibitors of intracellular signalling pathways and direct orally acting anticoagulants
- Includes sections on blood transfusion and the haematological aspects of systemic diseases, pregnancy and the neonate
Hoffbrand's Essential Haematology is a vital resource for all students and trainees, and a valuable reference for practicing specialists wishing to update their knowledge.
Frequently asked questions
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Information
CHAPTER 1
Haemopoiesis
Key topics
- Site of haemopoiesis
- Haemopoietic stem and progenitor cells
- Bone marrow stroma
- The regulation of haemopoiesis
- Haemopoietic growth factors
- Growth factor receptors and signal transduction
- Adhesion molecules
- The cell cycle
- Transcription factors
- Epigenetics
- Apoptosis
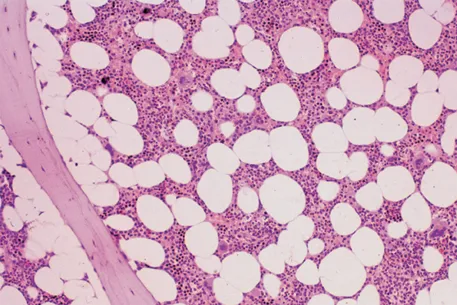
Site of haemopoiesis
| Fetus | 0–2 months (yolk sac) |
| 2–7 months (liver, spleen) | |
| 5–9 months (bone marrow) | |
| Infants | Bone marrow (practically all bones); dwindling post-parturition contribution from liver/spleen that ceases in the first few months of life |
| Adults | Vertebrae, ribs, sternum, skull, sacrum and pelvis, proximal ends of femur |
Haemopoietic stem and progenitor cells
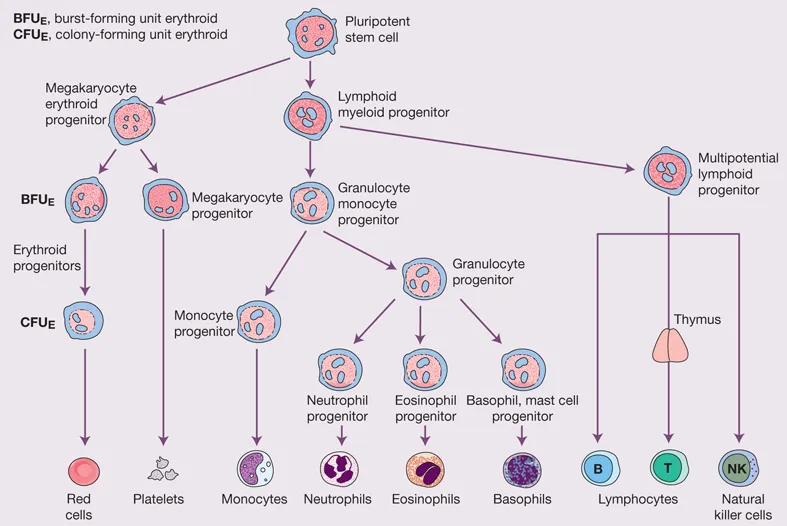
Table of contents
- Cover
- Title Page
- Copyright
- Preface to the Eighth Edition
- Preface to the First Edition
- How to use your textbook
- About the companion website
- Chapter 1 Haemopoiesis
- Chapter 2 Erythropoiesis and general aspects of anaemia
- Chapter 3 Hypochromic anaemias
- Chapter 4 Iron overload
- Chapter 5 Megaloblastic anaemias and other macrocytic anaemias
- Chapter 6 Haemolytic anaemias
- Chapter 7 Genetic disorders of haemoglobin
- Chapter 8 The white cells, part 1: granulocytes, monocytes and their benign disorders
- Chapter 9 The white cells, part 2: lymphocytes and their benign disorders
- Chapter 10 The spleen
- Chapter 11 The aetiology and genetics of haematological neoplasia
- Chapter 12 Management of haematological malignancy
- Chapter 13 Acute myeloid leukaemia
- Chapter 14 Chronic myeloid leukaemia
- Chapter 15 Myeloproliferative neoplasms
- Chapter 16 Myelodysplastic syndromes
- Chapter 17 Acute lymphoblastic leukaemia
- Chapter 18 The chronic lymphocytic leukaemias
- Chapter 19 Hodgkin lymphoma
- Chapter 20 Non-Hodgkin lymphomas
- Chapter 21 Multiple myeloma and related plasma cell neoplasms
- Chapter 22 Aplastic anaemia and bone marrow failure
- Chapter 23 Haemopoietic stem cell transplantation
- Chapter 24 Platelets, blood coagulation and haemostasis
- Chapter 25 Bleeding disorders caused by vascular and platelet abnormalities
- Chapter 26 Coagulation disorders
- Chapter 27 Thrombosis 1: pathogenesis and diagnosis
- Chapter 28 Thrombosis 2: treatment
- Chapter 29 Haematological changes in systemic diseases
- Chapter 30 Blood transfusion
- Chapter 31 Pregnancy and neonatal haematology
- Appendix
- Index
- End User License Agreement