- 290 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Self Assessment in Musculoskeletal Pathology X-rays by in PDF and/or ePUB format, as well as other popular books in Medicine & Diagnostics Imaging. We have over one million books available in our catalogue for you to explore.
Information
1
Arthritis
Karen Sakthivel-Wainford
Introduction
Arthritis is a collection of diseases that affect the true or diarthrodial joint (see Figure 1.1). A diarthrodial joint consists of cartilage covering the articular ends of the bones forming the joints, the articular capsule which is reinforced by ligamentous structures and the joint space which is lined with synovial membrane and filled with synovial fluid.
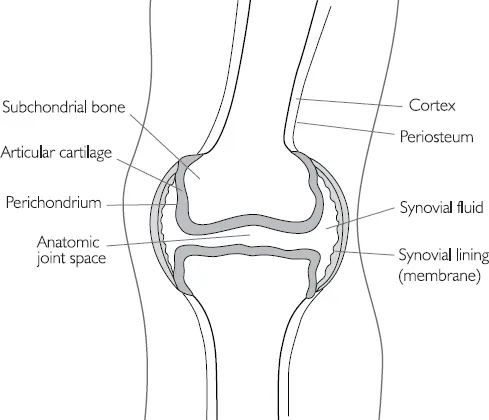
Figure 1.1 Diarthrodial joint
The abnormality of the joint in arthritis usually consists of destruction of the articular cartilage which appears on the radiograph as a narrowing of the joint space; narrowing of the joint is the cardinal sign of arthritis. However in some arthritic processes the joint space may become expanded instead, for example in the early stages of some arthrides, when there is joint effusion and ligament laxity.
However this does not help in distinguishing one arthropathy from another radiographically. The rest of this chapter will give brief descriptions of some of the most common arthropathies, but mainly will attempt to give some guidance in distinguishing one arthropathy from another.
In order to focus our minds when looking at arthrides, Debbie Forrester (Forrester and Brown, 1998) suggests the following ABCS search pattern:
Alignment (is there subluxation or dislocation?)Bone mineralisation (is sclerosis or osteopenia present?)Cartilage (including a search for erosions, plus loss of joint space)Soft tissues (is there soft tissue swelling, tophi of gout, calcification in the soft tissues as in scleroderma?)
Helms (1995) expands on this by including D for distribution, making it ABCDS. For example, in the hands what is the distribution of the disease process? Is it distal (as in osteoarthritis), or proximal (as in rheumatoid arthritis)? Also does the distribution affect the spine, or the sacroiliac joints? According to Helm if the distribution can be determined the differential diagnosis can become quite short. However sometimes in the hands it can be difficult to assess the distribution, particularly when there is severe rheumatoid arthritis and the proximal nature of disease is not evident.
Below are some of the many arthropathies, for which I will give some key points in their radiographic appearance, in order to help you recognise them. Radiographic examples of arthropathies and more information will be found in the case studies.
Arthrides and Arthropathies
Osteoarthritis
Diffuse idiopathic skeletal hyperostosis
Inflammatory arthritis
• Rheumatoid arthritis
Rheumatoid variants:
• Ankylosing spondylitis
• Reiter’s syndrome
• Psoriatic arthritis
Metabolic and endocrine:
• Calcium pyrophosphate disease
• Gout
Charcot joint
Connective tissue arthropathy:
• Systemic lupus erythematosus
• Scleroderma
• Dermatomyositis
Synovial osteochondromatosis
Infectious arthritis
Osteoarthritis
Osteoarthritis (OA) is the commonest chronic joint disease, characterised by the progressive erosion of articular cartilage. The association between OA and aging is well documented but is in fact non-linear; the prevalence increases exponentially over the age of 50 years. About 80% to 90% of individuals of both sexes have evidence of OA by the time they reach 65 years of age.
In the majority of instances OA appears insidiously, without apparent initiating cause as an aging phenomenon (idiopathic or primary OA). In these cases, the disease is usually oligoarticular but may be generalised. In about 5% of cases OA may appear in younger individuals with some predisposing conditions, such as previous macro trauma or repeated micro trauma to a joint, a congenital development deformity of a joint, or some underlying systemic disease such as diabetes, haemochromatous or marked obesity. In these cases the disease is called secondary OA and often involves one or several predisposed joints. OA is sometimes referred to as degenerative joint disease.
Gender has some influence on distribution, for example, the knees and hands are more commonly affected in women and hips in men. Primary general OA sometimes with familial influence is more common in women. Primary OA is seen only in the hands, where it affects the distal interphalangeal joints, the proximal interphalangeal joints and the base of the thumb in a bilateral symmetrical way.
The radiographic hallmarks of OA are:
• sclerosis
• osteophytes
• joint space narrowing
• distal distribution in the hands.
Joint space narrowing is the least specific (as mentioned earlier), but is always present in OA. Subchondral sclerosis is always present unless severe osteoporosis is present, which causes sclerosis to be diminished; osteophytosis may also be diminished in the presence of osteoporosis.
Another type of OA, although relatively rare, is erosive OA. It tends to be very painful and debilitating with identical distribution to primary OA (it affects the hands, the distal interphalangeal joints, proximal interphalangeal joints and the base of the thumb), but it is associated with severe osteoporosis and erosions of the hands.
Several other joints may demonstrate erosions as part of OA changes:
• temporomandibular joints
• sacroiliac joints
• acromioclavicular joints
• symphysis pubis.
Subchondral cysts or geodes may also be seen in OA, often in the shoulder or hip. In the hip they are sometimes called Edgars’ cysts.
Pathology
In the early stages of OA the chondrocytes proliferate forming ‘clones’. This is accompanied by biochemical changes as the water content of the matrix increases and the concentration of proteoglycins from the superficial zone of articular cartilage decreases. Disruption of the smooth surface of cartilage follows; parallel collagen fibres initially become tangential to the surface (flaking) and then extend vertically into the deeper zones (fibrillation) and cracking of the matrix occurs.
Gross examination at this stage would reveal a granular articular surface that is softer than normal. Friction smoothes the exposed bone, giving it the appearance of polished ivory (bone eburnation). At the same time there is thickening of the subchondral bone plate, rebuttressing and sclerosis of the underlying cancellous bone. Small fractures of the articulating bone are common and the dislodged pieces of cartilage and subchondral bone fall into the joint forming loose bodies (joint mice). The gaps at these fracture sites allow synovial fluid to be forced into the subchondral region in a one-way, ball-valve like mechanism. The loculated fluid collection increases in size, forming fibrous walled cysts. Mushroom shaped osteophytes develop at the margins of the articular surface and are capped by fibrocartilage and hyaline cartilage that gradually ossifies. See Figure 1.2.
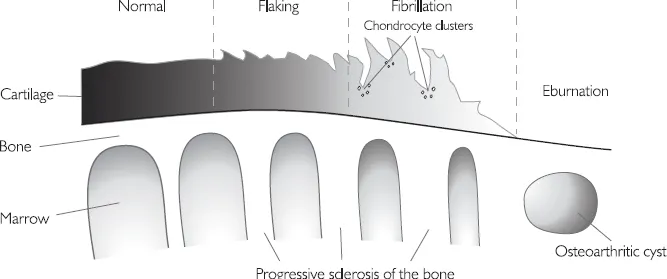
Figure 1.2 A schematic representation of the sequential changes of osteoarthritis
Diffuse idiopathic skeletal hyperostosis (DISH)
DISH is the only disease that causes osteophytes without loss of joint space, or sclerosis. It is of unknown aetiology. It results in severe productive changes of the spine, including annulus fibrosus, anterior longitudinal ligament, and sometimes paravertebral connective tissue.
Three criteria exist for diagnosis:
• flowing ossification of the anterolateral aspect of at least four continuous vertebral bodies
• preservation of disc height
• sacroiliitis and facet joint ankylosis are not present.
Inflammatory Arthritis
Rheumatoid Arthritis
Rheumatoid arthritis (RA) is a common arthritis of unknown aetiology which causes synovial inflammation and articular destruction that is often polyarticular. The term ‘classic RA’ is used to refer to one form of arthritis of unknown aetiology, other forms being considered a variant of this standard type. Classic RA may be described as follows: the patient is a young adult, more often female, complaining of pains in many joints, particularly fingers, wrists, elbows, knees and ankles. The same joints are affected in both limbs, though not necessarily with equal severity. Patients with classical RA normally have signs of an inflammatory, erosive arthritis and a positive rheumatoid factor. See Figure 1.3.
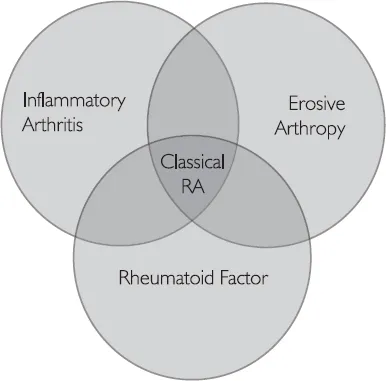
Figure 1.3 Venn diagram of classic RA
RA radiographic hallmarks are:
• soft tissue swelling
• osteoporosis
• joint space narrowing
• marginal erosions
• proximal and bilateral symmetry in the hands (unless the patient has had a stroke, in which case the affected side is spared).
Table 1.1 ...
Table of contents
- Cover Page
- Title Page
- Copyright
- Contents
- List of figures
- List of tables
- Acknowledgements
- Introduction
- 1 Arthritis
- 2 Osteoporosis
- 3 Bone Tumours
- 4 Avascular Necrosis and the Osteochondroses
- 5 Arthropathies
- 6 Tumours
- 7 Metabolic Bone Disease
- 8 Miscellaneous Cases
- 9 Mixed Cases
- Reading list/bibliography
- Index