Implant Therapy
Clinical Approaches and Evidence of Success, Second Edition
- 544 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
Implant Therapy
Clinical Approaches and Evidence of Success, Second Edition
About this book
Since the publication of the first edition of this book 20 years ago, the landscape of implant dentistry has changed dramatically. Both the industry and patient demand have expanded exponentially, leaving the clinician with many decisions to make (and often as many questions to ask) regarding patient selection, surgical timing and techniques, implant types, and restorative approaches. This volume brings together the knowledge of the foremost leaders in implant dentistry, covering all aspects of the treatment process, from decision-making and treatment planning through imaging, surgical techniques, bone and soft tissue augmentation, multidisciplinary approaches, loading protocols, and finally strategies for preventing and treating complications and peri-implantitis as well as providing effective implant maintenance therapy. Filled with expert knowledge based on decades of research and clinical experience as well as abundant illustrations and clinical case presentations, this book is an indispensable resource for clinicians seeking to provide implant treatment at the highest standard of care.
Tools to learn more effectively

Saving Books

Keyword Search

Annotating Text

Listen to it instead
Information




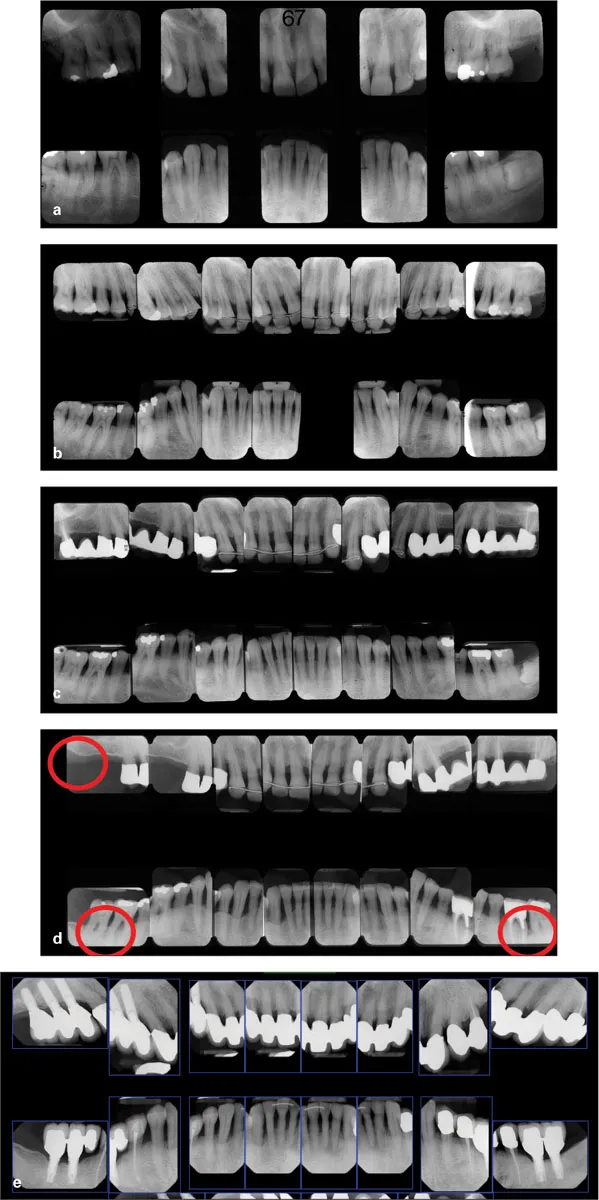
Table of contents
- Cover
- Half Title
- Title Page
- Copyright Page
- Contents
- Dedications
- Foreword
- Preface
- Contributors
- 1 A Clinical Decision: Save the Tooth or Place an Implant?: MYRON NEVINS • RICHARD I. HERMAN • YOSHIHIRO ONO
- 2 From Osseointegration to Predictable Long-Term Implant Stability: Clinicians’ Perspectives
- 3 Introduction to Implant Surgery: Optimal Positioning of the Dental Implant: HOM-LAY WANG • JIA-HUI FU
- 4 Implant Placement for the Mandibular Posterior Quadrant: HSUN-LIANG CHAN • HOM-LAY WANG • MYRON NEVINS
- 5 An Introduction to the Success of Short Dental Implants: CRAIG M. MISCH
- 6 The Evolution of Imaging and Associated Applications for Implant Surgery: GEORGE A. MANDELARIS • BRADLEY S. DEGROOT
- 7 Decision Making for Implant Therapy in the Maxillary Esthetic Zone: SVEN MÜHLEMANN • DAVID SCHNEIDER • RONALD E. JUNG • CHRISTOPH H. F. HÄMMERLE
- 8 Management of the Extraction Site: Socket Grafting: GUSTAVO AVILA-ORTIZ • HOMAYOUN H. ZADEH
- 9 Placement of Dental Implants into Extraction Sockets: DAVID M. KIM • JERRY CHING-YI LIN • CHIA-YU (JENNIFER) CHEN
- 10 Seeking the Optimal Esthetic Result in the Maxillary Anterior: DANIELE CARDAROPOLI
- 11 Predictable Esthetic Anterior Maxillary Reconstruction with Dental Implants and Maxillary Tuberosity Grafts: JOSÉ CARLOS MARTINS DE ROSA • LUÍS ANTÔNIO VIOLIN PEREIRA
- 12 Immediate Loading of Implants in Edentulous and Partially Dentate Patients: TIZIANO TESTORI • FABIO GALLI • RICCARDO SCAINI • MATTEO DEFLORIAN • ANDREA PARENTI • HOM-LAY WANG • MASSIMO DEL FABBRO
- 13 Sinus Elevation in the Posterior Maxilla via the Lateral Window Approach: STEPHEN S. WALLACE • TIZIANO TESTORI
- 14 Maxillary Transcrestal Sinus Floor Elevation Procedures: HOM-LAY WANG • ANN DECKER • TIZIANO TESTORI
- 15 The Use of Zygomatic Implants for Maxillary Edentulous Patients: JAMES K. F. CHOW • GLEN LIDDELOW
- 16 Treatment of the Edentulous Patient Using All-on-Four and the Zygoma Implant: STEPHEN M. PAREL • PAULO MALÓ • MIGUEL DE ARAÚJO NOBRE
- 17 Horizontal Bone Augmentation Procedures: A GBR Approach: MARCO RONDA • MASSIMO SIMION • FORTUNATO ALFONSI
- 18 Vertical Bone Augmentation with Advanced Flap Design: ISTVAN URBAN
- 19 Growth Factors: Clinical Development for Periodontal and Implant Applications: MARC L. NEVINS • WILLIAM V. GIANNOBILE • YOUNG-DAN CHO • (JEFF) CHIN-WEI WANG
- 20 The Introduction of Tissue Engineering for Bone Regeneration: ROBERT E. MARX
- 21 Soft Tissue Management to Augment Implant Success: GIOVANNI ZUCCHELLI • MARTINA STEFANINI
- 22 Implant-Abutment Junction: A Crestal Bone and Soft Tissue Determinant: LUIGI CANULLO
- 23 Effective Application of Orthodontics with Implant Therapy for Periodontally Compromised Patients: YOSHIHIRO ONO • TAKESHI SASAKI • MITSUHIRO IWATA • SACHIKO MAEDA • TOKOU MATSUI • KIMIO NAKAMURA • KIYONOBU SABURI • SATOKO ONO RUBIN
- 24 The Interaction Between Implantology and Orthognathic Surgery: LEANDRO G. VELASCO
- 25 Etiology and Management of Post-Loading Complications: Implant Loss or Failure and Peri-implantitis: STUART J. FROUM • PARNWARD HENGJEERAJARAS • KUAN-YOU LIU • PANPICHA MAKETONE • YE SHI
- 26 Regenerative Protocol to Treat Peri-implantitis: STEFANO PARMA-BENFENATI • CARLO TINTI • MARISA RONCATI
- 27 The Importance of Dedicated Maintenance Therapy for Long-Term Success: MARISA RONCATI
- 28 Peri-implant Maintenance Therapy for Long-Term Success: ALBERTO MONJE • HOM-LAY WANG
- 29 Implant Complications: A Reality Requiring Prevention: MARK E. LUDLOW • LYNDON F. COOPER
- Index
Frequently asked questions
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app