- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
About this book
Foodborne illness is a big problem. Wash those chicken breasts, and you're likely to spread Salmonella to your countertops, kitchen towels, and other foods nearby. Even salad greens can become biohazards when toxic strains of E. coli inhabit the water used to irrigate crops. All told, contaminated food causes 48 million illnesses, 128,000 hospitalizations, and 3,000 deaths each year in the United States.
With Outbreak, Timothy D. Lytton provides an up-to-date history and analysis of the US food safety system. He pays particular attention to important but frequently overlooked elements of the system, including private audits and liability insurance.
Lytton chronicles efforts dating back to the 1800s to combat widespread contamination by pathogens such as E. coli and salmonella that have become frighteningly familiar to consumers. Over time, deadly foodborne illness outbreaks caused by infected milk, poison hamburgers, and tainted spinach have spurred steady scientific and technological advances in food safety. Nevertheless, problems persist. Inadequate agency budgets restrict the reach of government regulation. Pressure from consumers to keep prices down constrains industry investments in safety. The limits of scientific knowledge leave experts unable to assess policies' effectiveness and whether measures designed to reduce contamination have actually improved public health. Outbreak offers practical reforms that will strengthen the food safety system's capacity to learn from its mistakes and identify cost-effective food safety efforts capable of producing measurable public health benefits.
With Outbreak, Timothy D. Lytton provides an up-to-date history and analysis of the US food safety system. He pays particular attention to important but frequently overlooked elements of the system, including private audits and liability insurance.
Lytton chronicles efforts dating back to the 1800s to combat widespread contamination by pathogens such as E. coli and salmonella that have become frighteningly familiar to consumers. Over time, deadly foodborne illness outbreaks caused by infected milk, poison hamburgers, and tainted spinach have spurred steady scientific and technological advances in food safety. Nevertheless, problems persist. Inadequate agency budgets restrict the reach of government regulation. Pressure from consumers to keep prices down constrains industry investments in safety. The limits of scientific knowledge leave experts unable to assess policies' effectiveness and whether measures designed to reduce contamination have actually improved public health. Outbreak offers practical reforms that will strengthen the food safety system's capacity to learn from its mistakes and identify cost-effective food safety efforts capable of producing measurable public health benefits.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Outbreak by Timothy D. Lytton in PDF and/or ePUB format, as well as other popular books in Law & Food Industry. We have over one million books available in our catalogue for you to explore.
Information
Publisher
University of Chicago PressYear
2019Print ISBN
9780226611686, 9780226611549eBook ISBN
97802266117161
Trouble in the Fields:
An Introduction to the Food Safety System
The family farms of Rocky Ford, Colorado, enjoy a well-deserved reputation for producing exceptionally flavorful cantaloupes. The surrounding Arkansas River Valley offers ideal conditions for melon cultivation—hot days and cool nights that enhance the plants’ sugar production. But in 2011, cantaloupes from this region attracted attention for a different reason. They were the source of one of the deadliest food poisoning outbreaks in US history.
Eric and Ryan Jensen, two hardworking brothers in their mid-thirties, raised and packed cantaloupes ninety miles east of Rocky Ford. Fourth-generation melon farmers, the brothers inherited 160 acres from their father and expanded their operations to 6,000 acres. During the 2011 harvest, Jensen Farms produced three hundred thousand cases of cantaloupes, labeled “Sweet Rocky Fords,” which were sold through a distributor to leading retail supermarkets, such as Walmart, Kroger, and Safeway. Many of these melons were contaminated with a virulent bacterial pathogen, Listeria monocytogenes, and they caused 147 reported cases of serious illness and thirty-three deaths in twenty-eight states.1
No one has ever conclusively identified the source of the contamination. One possibility is organic fertilizer. At the time of the outbreak, the brothers were in the midst of a three-year process of converting their operations from conventional to organic production, which requires replacing mineral fertilizers and chemical pesticides with alternatives derived from plants and animals. From a business perspective, the brothers sought to profit from the growing consumer demand for organic fruits and vegetables. They also had a deeply personal reason for the shift. Their father, Robert Jensen, had died in March 2010, at the age of fifty-nine, from cancer, which the brothers suspected might have been caused by pesticide or other chemical exposure. They believed that organic production would redeem Jensen Farms from decades of synthetic fertilizer and pesticide application. However, organic fertilizers also pose risks to human health. If not properly treated, they can harbor microorganisms, including bacterial pathogens such as Salmonella, E. coli, and Listeria.2
The Jensen brothers were not unmindful of the risk of bacterial contamination. They began post-harvest processing by immersing the melons in a dunk tank filled with chlorinated water to remove dirt and reduce harmful bacteria on the surface of the fruit. The melons were then dried, packed into crates, placed in cold storage, and later shipped to a distributor for sale to retail stores. In August 2010, a private food safety auditor inspected the fields and packinghouse operations, awarding Jensen Farms a score of 95 percent and a “superior” rating. When one of the brothers asked how they could improve their processing, the auditor responded that the dunk tank, with its recirculating water, was a potential food safety “hot spot” and that they should consider replacing it.3
The following spring, with advice from a local equipment supplier, the brothers purchased and installed spray-washing equipment originally designed to clean potatoes and modified for melon processing. The new equipment used non-recirculating city water to wash the melons as they passed along a conveyer belt. A subsequent July 2011 audit awarded Jensen Farms a score of 96 percent and another “superior” rating. The audit report noted that the spray wash system “does not have anti-microbial solution injected,” but this was not characterized as a deficiency, nor did it detract from the audit score. To the Jensens, the new non-recirculating spray wash system appeared more sanitary than the old dunk tank, which became increasingly dirty during the course of each production run. However, without antimicrobial solution added to the wash water, the spray wash spread bacterial contamination from melon to melon and dispersed it all over the processing equipment.4
By late August, Colorado health officials began receiving reports of individuals suffering from listeriosis. On September 2, they notified the federal Centers for Disease Control and Prevention (CDC) of seven cases in the state. Within a week, state and federal investigators traced the source of the outbreak to Jensen Farms cantaloupe. Four investigators arrived at the farm on September 9 and 10 to collect samples. Tests confirmed that samples taken from Jensen Farms melons, equipment, and facilities contained the same pathogenic strains of Listeria as those found in recently reported cases of listeriosis. The Jensens immediately ceased shipment of their cantaloupes and destroyed their remaining crops, and on September 14, the company voluntarily ordered a seventeen-state recall of its melons.5
The recall came too late for forty-eight-year-old Shelly Occhipinti-Krout, who left behind a husband and three children when she died from listeriosis, which she contracted from eating Jensen Farms cantaloupe. “It started with just flu-like symptoms,” her daughter Tiffany recalls. “Then she collapsed . . . and was taken to the hospital. While she was getting a CAT scan, she went into cardiac arrest, and doctors put her into a medically induced coma.” After three weeks in the hospital, her body was so swollen from the infection that she was unrecognizable. “I kept thinking that she was going to come home,” says Tiffany. “She went like a normal person to the grocery store, got her stuff, came home, and ate it. From that my mom got sick, and I’m never going to see her again.”6
Eighty-seven-year-old William Beach also died of listeriosis from eating Jensen Farms cantaloupe. “He was in and out of the hospital several times,” remembers his wife, Monette. “About a month before he died, we were in the living room watching TV one night, and he said, ‘Honey, we’ve got trouble; there is something wrong with me, and I don’t know what it is.’” In the hospital, when doctors attempted to insert a feeding and medication tube, he began to hemorrhage through his mouth and nose. William eventually succumbed to the infection. “The bottom line here is that my father died because somebody didn’t do their job,” says William’s daughter Debbie, expressing a view held by many victims and their families. “I think it’s unconscionable. All of us hope that when we go it’s quick. But never, ever, do we ever think that it’s going to come with us spewing blood out of our mouth and our nose in terror because we don’t know what’s going on but we know it’s over. Somebody’s responsible for it.”7
In the end, public health authorities attributed 147 reported cases of listeriosis to tainted cantaloupes from Jensen Farms. Thirty-three victims died within weeks of consuming the melon, and another ten died months later, possibly as a result of the infection. Some of those who survived sustained brain injuries and other long-term disabilities. Victims and their families were left with large medical bills—in several cases exceeding a million dollars.8
Researchers at the CDC in Atlanta estimate that “48 million people get sick, 128,000 are hospitalized, and 3,000 die from foodborne diseases each year in the United States.” (For a detailed account of how researchers estimate the number of cases and the economic costs of foodborne illness, see appendix A.) These statistics have led many commentators to declare the food safety system “broken” and in need of significant reform. A report by the US Public Interest Research Group analyzing outbreaks and recalls in 2011 and 2012 concludes that foodborne illness caused by microbial contamination “has stayed stagnant and potentially grown worse, taking a substantial toll on public health and the economy,” and that “the rules and inspection systems we have now are not up to the task.”9
Not everyone agrees that outbreaks signify that the system is broken. Even highly effective regulatory programs tolerate a certain amount of risk. There will always be some residual risk in the food system—zero risk is simply not possible. As one food safety professional with more than thirty years of experience in the poultry sector puts it: “People who demand bacteria-free eggs just don’t understand where they come from—there’s only one way out of the chicken.” Nor is zero risk a desirable goal, because at a certain point, the costs of additional risk reduction would outweigh the benefits. Tom Vilsack, secretary of agriculture in the Obama administration, expressed a view widely shared within the food industry when he boasted in 2012 that, although there is admittedly room for improvement, the United States has the world’s “safest food supply—an achievement made possible by a wide range of skilled, dedicated people.”10
Leaving aside for the moment the question of how well the food safety system performs, available data suggest that foodborne illness in the United States is a problem of noteworthy magnitude comparable to other common sources of illness and injury that have attracted the attention of public health authorities. (The analysis that follows relies on data drawn from a variety of sources, collected using various methods, and covering different years. Some of the numbers represent direct tallies from health records, while others are estimates that rely on surveys and statistical models. The aim is to provide general perspective not precise comparisons.) By using the CDC estimate, figure 1.1 shows that annual deaths from foodborne illness are far fewer in number than those caused by tobacco smoking, obesity, and alcohol use; considerably fewer than those caused by poisoning, motor vehicles, and falls; comparable to those caused by drowning, fire, and natural disasters; and significantly greater than those caused by machinery, firearms, cycling, and cutting and piercing.
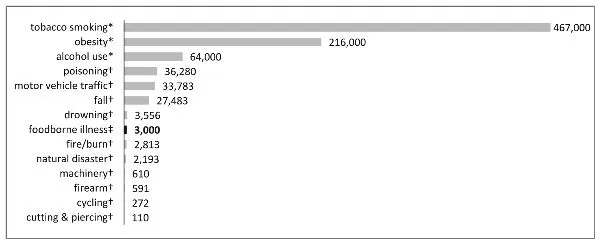
FIGURE 1.1. Leading causes of death annually from illness and unintentional injury.
* Estimates from 2005 data: Goodarz Danaei et al., “The Preventable Causes of Death in the United States Comparative Risk Assessment of Dietary, Lifestyle, and Metabolic Risk Factors,” PLOS Medicine 6, no. 4 (2009): https://doi.org/10.1371/journal.pmed.1000058.
† Based on census of medical records: CDC, “20 Leading Causes of Unintentional Injury Death, United States 2011,” WISQARS Leading Cause of Death Report, archived at http://perma.cc/U828-3VDH.
‡ Estimate from Elaine Scallan et al., “Foodborne Illness Acquired in the United States—Unspecified Pathogens,” Emerging Infectious Diseases 17, no. 1 (January 2011): 20.
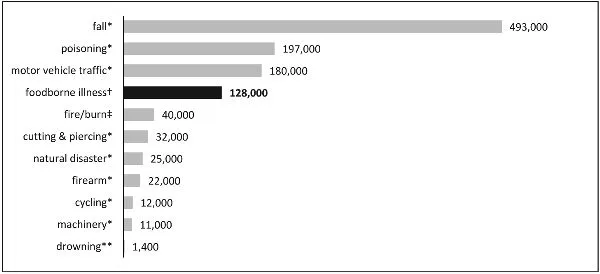
FIGURE 1.2. Annual hospitalization from foodborne illness and leading causes of nonfatal injury.
* Average annual hospital discharges 2004–2005, from G. Bergen, L. H. Chen, M. Warner, and L.A. Fingerhut, Injury in the United States: 2007 Chartbook (Hyattsville, MD: National Center for Health Statistics, 2008), 126, https://www.cdc.gov/nchs/data/misc/injury2007.pdf, archived at https://perma.cc/D99P-M9WT. The figure for firearms includes intentional injuries.
† Estimate from Elaine Scallan et al., “Foodborne Illness Acquired in the United States—Unspecified Pathogens,” Emerging Infectious Diseases 17, no. 1 (January 2011): 20.
‡ Based on hospital discharge data from 2010, American Burn Association, “Burn Incidence and Treatment in the United States: 2016, http://ameriburn.org/who-we-are/media/burn-incidence-fact-sheet/, archived at https://perma.cc/P3A3-MNMA.
** Estimate based on reports of emergency department visits for 2010 from CDC, “Data and Statistics (WISQARS): Cost of Injury Reports” (2,646 emergency department visits), archived at https://perma.cc/284C-DYHC; CDC, “Unintentional Drowning: Get the Facts” (stating that more than 50 percent of drowning victims treated in emergency departments require hospitalization), https://www.cdc.gov/homeandrecreationalsafety/water-safety/waterinjuries-factsheet.html, archived at https://perma.cc/TQY4-3PJT. Compare Stephen Bowman et al., “Trends in US Pediatric Drowning Hospitalizations, 1993–2008,” Pediatrics 129, no. 2 (February 2012) (2000 annual hospitalizations from drowning for children age 0–19).
Figure 1.2 compares the estimated number of hospitalizations from foodborne illness to those from leading sources of injury.11 Although hospitalizations from foodborne illness are fewer than those of the top three sources of nonfatal injury—falls, poisoning, and motor vehicle accidents—they exceed several other leading sources, such as burns, cutting and piercing, natural disasters, firearms, cycling, machinery, and drowning.
Figure 1.3 suggests that the estimated number of foodborne illness episodes involving acute illness far exceeds that of other leading forms of unintentional injury.12
Using estimates from researchers at the US Department of Agriculture (USDA) Economic Research Service, figure 1.4 compares the cost of medical care due to foodborne illness and leading forms of illness and unintentional injury. The medical costs of foodborne illness rank below those of tobacco smoking, obesity, falls, cycling, alcohol use, motor vehicle accidents, and poisoning, but they exceed those of burns, drowning, and firearms.
The burden of foodborne illness falls most heavily on the elderly, who are at greatest risk of death or severe complications. Half of the reported listeriosis cases in the Jensen Farms melon outbreak were among individuals older than seventy-seven years, and most who died were older than eighty. In a 2011 report on foodborne illness caused by major pathogens, the CDC found that 13 percent of infections, 24 percent of hospitalizations, and 57 percent of deaths occurred among adults sixty-five or older. Thus, the elderly not only face a higher risk of infection; they are also far more likely to suffer serious illness and death as a result. Young children and those who are immunosuppressed—for example, cancer patients receiving chemotherapy—also face a higher risk.13
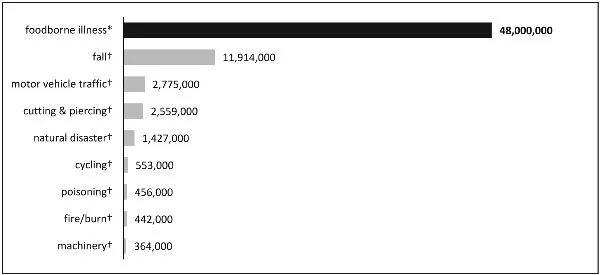
FIGURE 1.3. Annual episodes of foodborne illness and unintentional injury.
* Estimate of episodes of illness from Elaine Scallan et al., “Foodborne Illness Acquired in the United States—Unspecified Pathogens,” Emerging Infectious Diseases 17, no. 1 (January 2011): 20. The definition of an episode of foodborne illness includes only acute illness, for example, gastroenteritis involving three or more loose stools in twenty-four hours or vomiting, lasting more than one day or resulting in restricted daily activities (see Scallan et al., 17).
† Average annual injury episodes 2004–2005, from G. Bergen, L. H. Chen, M. Warner, and L.A. Fingerhut, Injury in the United States: 2007 Chartbook (Hyattsville, MD: National Center for Health Statistics, 2008), 127, https://www.cdc.gov/nchs/data/misc/injury2007.pdf, archived at https://perma.cc/D99P-M9WT. The definition of an episode of injury includes only acute injury, defined as a fatal or medically attended injury (see Chartbook, 8).
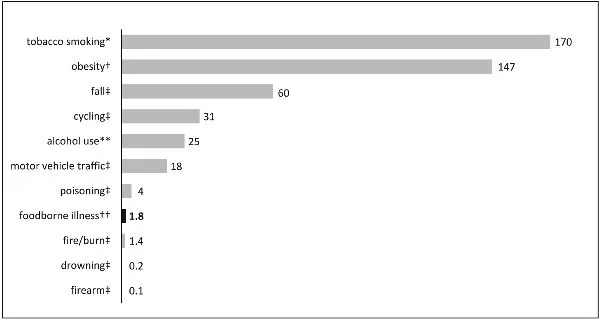
FIGURE 1.4. Annual cost of medical care for leading causes of death, illness, and unintentional injury ($ billion).
* Estimate for 2014 from CDC, “Smoking and Tobacco Use, Costs and Expenditures,” https://www.cdc.gov/tobacco/data_statistics/fact_sheets/fast_facts/, archived at https://perma.cc/S6KB-QQDE.
† Estimate for 2008 from CDC, “Adult Obesity Facts,” https://www.cdc.gov/obesity/data/adult.html, archived at https://perma.cc/XQE4-T77C.
‡ Estimates for 2010 from CDC, “Data and Statistics (WISQARS): Cost of Injury Reports,” archived at https://perma.cc/R8RX-YWGC.
** Estimate for 2006 from CDC, “Excessive Drinking Is Draining the U.S. Economy,” https://www.cdc.gov/features/costsofdrinking/, archived at https://perma.cc/VM45-GQFN.
†† Estimate for 2013 from Sandra Hoffmann, Bryan Maculloch, and Michael Batz, “Economic Burden of Major Foodborne Illnesses Acquired in the United States,” Economic Research Service of the USDA, Economic Information Bulletin, no. 140, May 2015, 11 (includes cost of medical care for fifteen leading foodborne illnesses, which constitute app...
Table of contents
- Cover
- Title Page
- Copyright Page
- Dedication
- Contents
- 1 Trouble in the Fields
- 2 The Gospel of Clean Milk
- 3 Canned Foods under Pressure
- 4 Building a Better Burger
- 5 Making Salad Safe Again
- 6 Bean Counting
- 7 From Fork to Farm
- 8 Recipes for Reform
- 9 Food for Thought
- Appendix A
- Appendix B
- Appendix C
- Appendix D
- List of Abbreviations
- Timeline of Significant Events
- Acknowledgments
- Notes
- Index